Accessory head of flexor pollicis longus and its significance in anterior interosseus nerve neuropathies and precision handlingclinical entity
Shanmuga Sundaram Mani*, Vishnumaya G and Madhan Kumar SJ
Department of Anatomy, SRM Medical College, Tamil Nadu, India
- *Corresponding Author:
- Shanmuga Sundaram Mani
Assistant Professor, Department of Anatomy, SRM Medical College, SRM Nagar, Potheri, Kancheepuram District, Chennai – 603203, Tamil Nadu India
Tel: +91 944 3419528
E-mail: drshanmugas@gmail.com
Date of Received: September 19th, 2009;
Date of Accepted: January 21st, 2010
Published Online: April 15th, 2010
© IJAV. 2010; 3: 46–48.
[ft_below_content] =>Keywords
flexor pollicis longus, accessory head, anterior interosseus nerve, precision handling
Introduction
Flexor pollicis longus is one of the deep flexors of the forearm. It takes its origin from the grooved anterior surface of the radius and from the adjacent interosseus membrane and gets inserted onto the base of the distal phalanx of the thumb [1]. It has been noted that it frequently arises from a variable slip from the lateral or more rarely from the medial border of the coronoid process or also from the medial epicondyle of the humerus. This variable slip has also been called as the Gantzer’s muscle or occasional head [2]. The presence of Gantzer’s muscle has been noted to be around 50-60% by Al-Quattan [3] and Oh [4]. There have been various reports of occurrence of the additional head of flexor pollicis longus. The prevalence’s ranged from 75 % [2], 5.3 % [5], 54.2% [6], 55% [7], 66.66% [8], 62% [9]. There have also been reports of bilateral and unilateral presentation of the accessory head saying that there are more chances for it to occur bilaterally than unilaterally [3,4,8,10,11,12]. There have also been reports of variations in the origin of the accessory head [2,3,6,7,9,10,11,13].
The flexor pollicis is supplied by the anterior interosseus nerve which descends on the interosseus membrane between the flexor pollicis longus and the flexor digitorum profundus. It traverses down the forearm to supply three muscles of the forearm namely, flexor pollicis longus, flexor digitorum longus and pronator quadratus. The anterior interosseus nerve syndrome is a relatively rare handlingclinical entity which produces a square pinch deformity [14,15,16,17].
Case Report
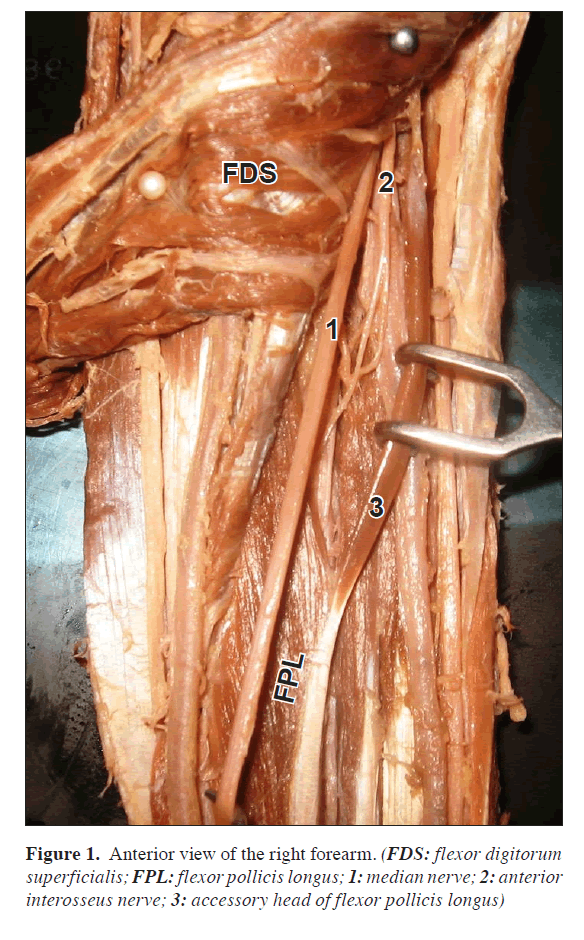
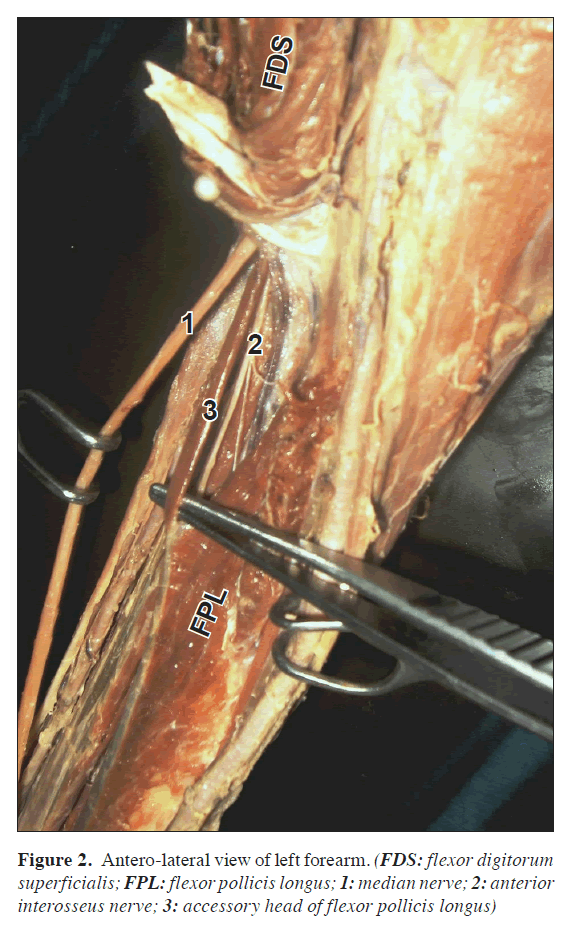
During routine dissection of of a 65-year-old female cadaver, we noted the bilateral presence of an additional head of the flexor pollicis longus. This variable slip took its origin from the lateral border of the coronoid process of ulna as demonstrated in Figure 1. The further course of the slip ran laterally and got inserted into the medial border of middle third of the belly of the flexor pollicis longus muscle (Figure 2).
Discussion
The accessory head of flexor pollicis longus usually presents itself as lying between the median nerve and the anterior interosseus nerve, the former lying anteriorly and the latter posteriorly [2,7,8,10,12]. There have also been reports by Dellon & Mackinnnon [11] and Al – Quattan [3] stating that the nerve passed anteriorly to the muscle belly. According to a study done on 240 limbs prevelance of accessory head of flexor pollicis longus (AHFPL) was observed in 149 specimens. In these 149 specimens, four patterns of relationships of AHFPL with anterior interosseous nerve (AIN) were noted: 1) AIN passed anterior to AHFPL, 13.4% (20/149); 2) AIN passed lateral to AHFPL, 65.8% (98/149); 3) AIN passed posterior to AHFPL, 8.1% (12/149); and 4) AIN passed both lateral and posterior to AHFPL, 12.8% (19/149) [9]. Anterior interosseus nerve is susceptible to entrapment by soft tissue, vascular and bony structures. Palsy of the anterior interosseus nerve has been described in association with neuralgic amyotrophy, isolated neuritis and entrapment neuropathy [18]. Repetitive trauma to the forearm and structural anomalies cause anterior interosseous nerve syndrome [19] Hence it would be plausible that anterior interosseus nerve passing posteriorly or laterally to the additional head of flexor pollicis longus muscle would be more likely to be associated with anterior interosseous nerve syndrome due to anatomic considerations.
Flexor pollicis longus stabilizes the flexed phalanx of the thumb. In precision handling (finger- thumb prehension) and powerful grip (full hand prehension) the flexor pollicis longus acts as a stabilizer [20]. Kaplan [21] has described a case of a long standing flexion contracture of the inter- phalangeal joint of the thumb following a fracture dislocation of the elbow which was later found to be due to the cicatricial contraction of the accessory belly of the flexor pollicis longus and had to be subsequently elongated to correct the deformity. Hence in a flexion deformity of the thumb, involvement of the occasional head has to be kept in mind [10]. According to Levangie and Norkin [20], the architecture of the whole muscle may be important in determining muscle function, structural variations affect not only the overall shape and size of the muscle but also function of the skeletal muscle especially range of motion. The additional head of flexor pollicis longus is made of fusiform muscle fibers in opposition to unipennate muscle fibres of flexor pollicis longus. The function of fusiform muscle fiber is in direct opposition to unipennate fibres.
Hence it could be said that this could lead to an extra strain on the normal functional movements of the flexor pollicis longus, which could in turn lead to loss of precise and skilful movements. Hemmady [8] also states that the presence of the occasional head has to be borne in mind during anterior approaches to the proximal radius and the elbow joint, as also during a decompressive fasciotomy for compartment syndrome of the forearm.
A large number of accessory muscles have been chronicled in surgical and radiological literature, but the number of case reports is limited. Hence the presence of an accessory muscle must not be ruled out while diagnosing neuropathies of different types, a few of which are carpal tunnel, Guyon’s canal, cubital tunnel and tarsal tunnel.
To conclude a careful evaluation of fibrous tunnels for an accessory muscle may help identify such a muscle as the causative factor.
References
- Williams PL, Bannister LH, Berry MM, Collins P, Dyson M, Dussek JE, Ferguson MW, eds. Gray’s Anatomy. 38th Ed., New York, Churchill Livingstone. 1995; 848.
- Wood J. Variations in human myology. Proceedings of the Royal Society of London 1868; 16: 483–525.
- Al-Qattan MM. Gantzer’s muscle. An anatomical study of the accessory head of the flexor pollicis longus muscle. J Hand Surg Br. 1996; 275: 269–270.
- Oh CS, Chung IH, Koh KS. Anatomical study of the accessory head of the flexor pollicis longus and the anterior interosseus nerve in Asians. Clin Anat. 2000; 13: 434–438.
- Dykes J, Anson BJ. The accessory tendon of the flexor pollicis longus muscle. Anat Rec. 1944; 90: 83–89.
- Malhotra VK, Sing NP, Tewari SP. The accessory head of the flexor pollicis longus muscle and its nerve supply. Anat Anz. 1982; 151: 503–505.
- Jones M, Abrahams PH, Sanudo JR, Campillo M. Incidence and morphology of accessory heads of flexor pollicis longus and flexor digitorum profundus (Gantzer’s muscle). J Anat. 1997; 191: 451–455.
- Hemmady MV, Subramanya AV, Mehta IM. Occasional head of flexor pollicis longus muscle: a study of its morphology and clinical significance. J Postgrad Med. 1993; 39: 14–16.
- Mahakkanukrauh P, Surin P, Ongkana N, Sethadavit M, Vaidhayakarn P. Prevalence of accessory head of flexor pollicis longus muscle and its relation to anterior interosseus nerve in Thai population. Clin Anat. 2004; 17: 631–635.
- Mangini U. Flexor pollicis longus muscle. Its morphology and clinical significance. J Bone Joint Surg Am. 1960; 42: 467–470.
- Dellon AL, Mackinnon SE. Musculoaponeurotic variations along the course of the median nerve in the proximal forearm. J Hand Surg Br. 1987; 12: 359–363.
- Shirali S, Hanson M, Branovacki G, Gonzalez M. The flexor pollicis longus and its relation to the anterior and posterior interosseus nerves. J Hand Surg Br. 1998; 23: 170–172.
- Macalister A. Additional observations on muscular anomalies in human anatomy (3rd series), with a catalogue of the principal muscular variations hitherto published. Transactions of the Royal Irish Academy. 1875; 25: 1–134.
- Potu BK, Gorantla VR, Pulakunta T, Rao M S, Mamatha T, Vollala VR, Nayak SR. Accessory head of flexor pollicis longus muscle and its significance in anterior interosseous nerve syndrome: case report and review. Int J Morphol. 2007; 25: 911–914.
- Spinner M, Spencer PS. Nerve compression lesions of the upper extremity: a clinical and experimental review. Clin Orthop Relat Res. 1974; 104: 46–67.
- Hill NA, Howard FM, Huffer BR. The incomplete anterior interosseous nerve syndrome. J Hand Surg Am. 1985; 10: 4–16.
- Proudman TW, Menz PJ. An anomaly of the median artery associated with the anterior interosseous nerve syndrome. J Hand Surg Br. 1992; 17: 507–509.
- Nagano A. Spontaneous anterior interosseous nerve palsy. J Bone Joint Surg Br. 2003; 85: 313–318.
- Plancher KD, Peterson RK, Steichen JB. Compressive neuropathies and tendinopathies in the athletic elbow and wrist. Clin Sports Med. 1996; 15: 331–371.
- Levangie PK, Norkin CC. Joint Structure and Function: A Comprehensive Analysis. 4th Ed., Philadelpia, F. A. Davis Company. 2006; 120–121.
- Kaplan EB. Correction of a disabling contracture of the thumb. Bull Hosp Joint Dis. 1942; 3: 51–54.
Shanmuga Sundaram Mani*, Vishnumaya G and Madhan Kumar SJ
Department of Anatomy, SRM Medical College, Tamil Nadu, India
- *Corresponding Author:
- Shanmuga Sundaram Mani
Assistant Professor, Department of Anatomy, SRM Medical College, SRM Nagar, Potheri, Kancheepuram District, Chennai – 603203, Tamil Nadu India
Tel: +91 944 3419528
E-mail: drshanmugas@gmail.com
Date of Received: September 19th, 2009;
Date of Accepted: January 21st, 2010
Published Online: April 15th, 2010
© IJAV. 2010; 3: 46–48.
Abstract
During routine cadaveric dissection of the volar surface of the forearm of a South Indian female of 65 years, we came across a variant of occasional/accessory head of the flexor pollicis longus muscle. It was seen bilaterally arising from the deep surface of the flexor digitorum superficialis. It terminated by inserting into the principle (middle one-third) tendon of flexor pollicis longus. Its clinical significance in the formation of anterior interosseus nerve neuropathies and its probable significance in the loss of precision handling are discussed in detail. The usage of non-invasive methods such as cross sectional imaging techniques to detect the presence of such accessory heads of flexor pollicis muscle is also discussed.
-Keywords
flexor pollicis longus, accessory head, anterior interosseus nerve, precision handling
Introduction
Flexor pollicis longus is one of the deep flexors of the forearm. It takes its origin from the grooved anterior surface of the radius and from the adjacent interosseus membrane and gets inserted onto the base of the distal phalanx of the thumb [1]. It has been noted that it frequently arises from a variable slip from the lateral or more rarely from the medial border of the coronoid process or also from the medial epicondyle of the humerus. This variable slip has also been called as the Gantzer’s muscle or occasional head [2]. The presence of Gantzer’s muscle has been noted to be around 50-60% by Al-Quattan [3] and Oh [4]. There have been various reports of occurrence of the additional head of flexor pollicis longus. The prevalence’s ranged from 75 % [2], 5.3 % [5], 54.2% [6], 55% [7], 66.66% [8], 62% [9]. There have also been reports of bilateral and unilateral presentation of the accessory head saying that there are more chances for it to occur bilaterally than unilaterally [3,4,8,10,11,12]. There have also been reports of variations in the origin of the accessory head [2,3,6,7,9,10,11,13].
The flexor pollicis is supplied by the anterior interosseus nerve which descends on the interosseus membrane between the flexor pollicis longus and the flexor digitorum profundus. It traverses down the forearm to supply three muscles of the forearm namely, flexor pollicis longus, flexor digitorum longus and pronator quadratus. The anterior interosseus nerve syndrome is a relatively rare handlingclinical entity which produces a square pinch deformity [14,15,16,17].
Case Report
During routine dissection of of a 65-year-old female cadaver, we noted the bilateral presence of an additional head of the flexor pollicis longus. This variable slip took its origin from the lateral border of the coronoid process of ulna as demonstrated in Figure 1. The further course of the slip ran laterally and got inserted into the medial border of middle third of the belly of the flexor pollicis longus muscle (Figure 2).
Discussion
The accessory head of flexor pollicis longus usually presents itself as lying between the median nerve and the anterior interosseus nerve, the former lying anteriorly and the latter posteriorly [2,7,8,10,12]. There have also been reports by Dellon & Mackinnnon [11] and Al – Quattan [3] stating that the nerve passed anteriorly to the muscle belly. According to a study done on 240 limbs prevelance of accessory head of flexor pollicis longus (AHFPL) was observed in 149 specimens. In these 149 specimens, four patterns of relationships of AHFPL with anterior interosseous nerve (AIN) were noted: 1) AIN passed anterior to AHFPL, 13.4% (20/149); 2) AIN passed lateral to AHFPL, 65.8% (98/149); 3) AIN passed posterior to AHFPL, 8.1% (12/149); and 4) AIN passed both lateral and posterior to AHFPL, 12.8% (19/149) [9]. Anterior interosseus nerve is susceptible to entrapment by soft tissue, vascular and bony structures. Palsy of the anterior interosseus nerve has been described in association with neuralgic amyotrophy, isolated neuritis and entrapment neuropathy [18]. Repetitive trauma to the forearm and structural anomalies cause anterior interosseous nerve syndrome [19] Hence it would be plausible that anterior interosseus nerve passing posteriorly or laterally to the additional head of flexor pollicis longus muscle would be more likely to be associated with anterior interosseous nerve syndrome due to anatomic considerations.
Flexor pollicis longus stabilizes the flexed phalanx of the thumb. In precision handling (finger- thumb prehension) and powerful grip (full hand prehension) the flexor pollicis longus acts as a stabilizer [20]. Kaplan [21] has described a case of a long standing flexion contracture of the inter- phalangeal joint of the thumb following a fracture dislocation of the elbow which was later found to be due to the cicatricial contraction of the accessory belly of the flexor pollicis longus and had to be subsequently elongated to correct the deformity. Hence in a flexion deformity of the thumb, involvement of the occasional head has to be kept in mind [10]. According to Levangie and Norkin [20], the architecture of the whole muscle may be important in determining muscle function, structural variations affect not only the overall shape and size of the muscle but also function of the skeletal muscle especially range of motion. The additional head of flexor pollicis longus is made of fusiform muscle fibers in opposition to unipennate muscle fibres of flexor pollicis longus. The function of fusiform muscle fiber is in direct opposition to unipennate fibres.
Hence it could be said that this could lead to an extra strain on the normal functional movements of the flexor pollicis longus, which could in turn lead to loss of precise and skilful movements. Hemmady [8] also states that the presence of the occasional head has to be borne in mind during anterior approaches to the proximal radius and the elbow joint, as also during a decompressive fasciotomy for compartment syndrome of the forearm.
A large number of accessory muscles have been chronicled in surgical and radiological literature, but the number of case reports is limited. Hence the presence of an accessory muscle must not be ruled out while diagnosing neuropathies of different types, a few of which are carpal tunnel, Guyon’s canal, cubital tunnel and tarsal tunnel.
To conclude a careful evaluation of fibrous tunnels for an accessory muscle may help identify such a muscle as the causative factor.
References
- Williams PL, Bannister LH, Berry MM, Collins P, Dyson M, Dussek JE, Ferguson MW, eds. Gray’s Anatomy. 38th Ed., New York, Churchill Livingstone. 1995; 848.
- Wood J. Variations in human myology. Proceedings of the Royal Society of London 1868; 16: 483–525.
- Al-Qattan MM. Gantzer’s muscle. An anatomical study of the accessory head of the flexor pollicis longus muscle. J Hand Surg Br. 1996; 275: 269–270.
- Oh CS, Chung IH, Koh KS. Anatomical study of the accessory head of the flexor pollicis longus and the anterior interosseus nerve in Asians. Clin Anat. 2000; 13: 434–438.
- Dykes J, Anson BJ. The accessory tendon of the flexor pollicis longus muscle. Anat Rec. 1944; 90: 83–89.
- Malhotra VK, Sing NP, Tewari SP. The accessory head of the flexor pollicis longus muscle and its nerve supply. Anat Anz. 1982; 151: 503–505.
- Jones M, Abrahams PH, Sanudo JR, Campillo M. Incidence and morphology of accessory heads of flexor pollicis longus and flexor digitorum profundus (Gantzer’s muscle). J Anat. 1997; 191: 451–455.
- Hemmady MV, Subramanya AV, Mehta IM. Occasional head of flexor pollicis longus muscle: a study of its morphology and clinical significance. J Postgrad Med. 1993; 39: 14–16.
- Mahakkanukrauh P, Surin P, Ongkana N, Sethadavit M, Vaidhayakarn P. Prevalence of accessory head of flexor pollicis longus muscle and its relation to anterior interosseus nerve in Thai population. Clin Anat. 2004; 17: 631–635.
- Mangini U. Flexor pollicis longus muscle. Its morphology and clinical significance. J Bone Joint Surg Am. 1960; 42: 467–470.
- Dellon AL, Mackinnon SE. Musculoaponeurotic variations along the course of the median nerve in the proximal forearm. J Hand Surg Br. 1987; 12: 359–363.
- Shirali S, Hanson M, Branovacki G, Gonzalez M. The flexor pollicis longus and its relation to the anterior and posterior interosseus nerves. J Hand Surg Br. 1998; 23: 170–172.
- Macalister A. Additional observations on muscular anomalies in human anatomy (3rd series), with a catalogue of the principal muscular variations hitherto published. Transactions of the Royal Irish Academy. 1875; 25: 1–134.
- Potu BK, Gorantla VR, Pulakunta T, Rao M S, Mamatha T, Vollala VR, Nayak SR. Accessory head of flexor pollicis longus muscle and its significance in anterior interosseous nerve syndrome: case report and review. Int J Morphol. 2007; 25: 911–914.
- Spinner M, Spencer PS. Nerve compression lesions of the upper extremity: a clinical and experimental review. Clin Orthop Relat Res. 1974; 104: 46–67.
- Hill NA, Howard FM, Huffer BR. The incomplete anterior interosseous nerve syndrome. J Hand Surg Am. 1985; 10: 4–16.
- Proudman TW, Menz PJ. An anomaly of the median artery associated with the anterior interosseous nerve syndrome. J Hand Surg Br. 1992; 17: 507–509.
- Nagano A. Spontaneous anterior interosseous nerve palsy. J Bone Joint Surg Br. 2003; 85: 313–318.
- Plancher KD, Peterson RK, Steichen JB. Compressive neuropathies and tendinopathies in the athletic elbow and wrist. Clin Sports Med. 1996; 15: 331–371.
- Levangie PK, Norkin CC. Joint Structure and Function: A Comprehensive Analysis. 4th Ed., Philadelpia, F. A. Davis Company. 2006; 120–121.
- Kaplan EB. Correction of a disabling contracture of the thumb. Bull Hosp Joint Dis. 1942; 3: 51–54.