Block vertebra: fusion of axis with the third cervical vertebra – a case report
Veena Vidya Shankar* and Roopa R Kulkarni
Department of Anatomy, M. S. Ramaiah Medical College, Bangalore, India
- *Corresponding Author:
- Dr. Veena Vidya Shankar, MD
Lecturer, Department of Anatomy, M. S. Ramaiah Medical College, MSRIT post, Bangalore, 560054, India
Tel: +91 80 23605408/408
E-mail: veenavidyashankar@yahoo.com
Date of Received: June 15th, 2010
Date of Accepted: December 19th, 2010
Published Online: January 24th, 2011
© Int J Anat Var (IJAV).2011; 4: 15–16.
[ft_below_content] =>Keywords
cervical vertebra, axis, fusion, lamina, pedicle, block vertebra
Introduction
The distinguishing feature of the 2nd cervical vertebra (axis) is presence of odontoid process (dens) which articulates with anterior arch of atlas, and acts as a pivot around which atlas with skull rotates [1]. Severe neck pain and sudden unexpected death may occur due to skeletal abnormalities at the cranio-cervical junction or cervical region and is associated with neurological signs and symptoms [2]. Symptoms vary according to the extent of pathology.
Case Report
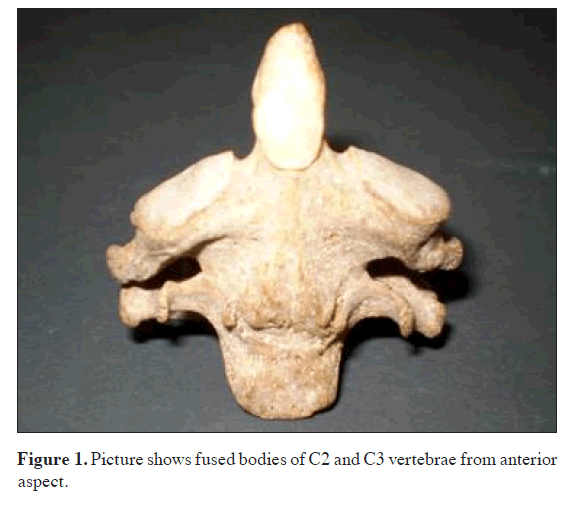
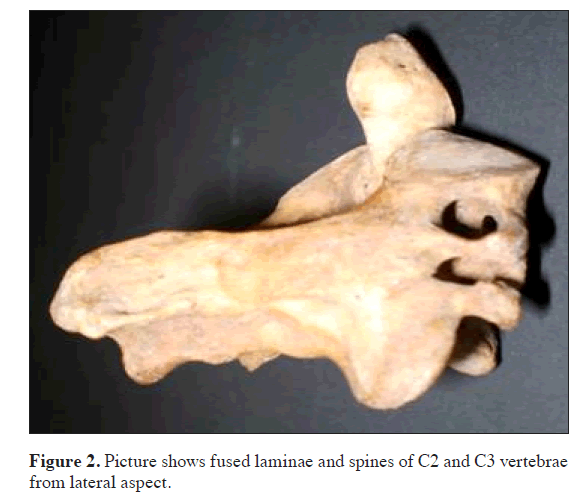
During the osteology demonstration of cervical vertebrae for the MBBS Phase I students at M. S. Ramaiah Medical College, it was observed that the axis was fused with 3rd cervical vertebra. The features of this fused cervical vertebrae was analyzed and the specimen was photographed from different aspects.
Observations:
• Body, laminae and spines of C2 and C3 were completely fused on both anterior and posterior aspects.
• Pedicles and transverse processes were not fused.
Foramina transversaria were present, and the diameter in C2 on the left side measured 4.72 mm and on right side 5.71 mm. Foramina transversaria in C3 on the left side measured 6.80 mm and on the right side it was 7.12 mm. The diameters were measured from superior aspect in C2 and from the inferior aspect in C3.
Discussion
Fused cervical vertebrae (FCV) have clinical and embryological importance. The anomalies of cervical region are of interest to anatomists, orthopedists, neurologists, neurosurgeons and even orthodontists. In FCV two vertebrae appear both structurally and functionally as one. This fusion may be congenital or acquired [3].
It is important to identify the cause of FCV – whether it is congenital or acquired or pathologic condition. Acquired FCV is generally associated with diseases like tuberculosis, other infections, juvenile rheumatoid arthritis and trauma. Clinical symptoms may vary from asymptomatic to myelopathy, limitation of the neck movement, or the muscular weakness, atrophy and neurological sensory loss or associated with Klippel-Feil syndrome [3].
The orthodontist may be the first person to detect cervical spine abnormalities as they are asymptomatic until adolescence or young adulthood. Early diagnosis is based on incidental radiographic findings.
According to Farman and Escobar, the radiographic appearance of congenital anomalies of the vertebral bodies may be due to defects in fusion or normal segmentation, occipitalization of the atlas, odontoid and atlas malformations, spina bifida and abnormal ossifications. There is increased incidence of osteophyte formation in the adjacent levels in cervical fusion. Up to 70% of occipitalizations have an accompanying C2–C3 fusion with instability at the C1–C2 articulation [4].
Early diagnosis of these anomalies will be helpful in documenting the change due to an injury, aging, or progression of a degenerative process and also motivates the patients to change their lifestyles to lead a normal life. Surgical intervention for block vertebra carries a higher risk of morbidity and mortality. On the contrary, cervical vertebral fusions are commonly done following traumatic, degenerative and inflammatory dislocations of upper and lower cervical spine [5]. The awareness and monitorization of complications like anesthetic risk during intubation with neck extension needs to be considered. Appropriate counseling on the management of known risk factors, including therapeutic options that can precipitate complication should be encouraged (like avoiding undue trauma, extension and rotational maneuvers which may place the spinal cord and vertebral artery at risk) [4].
Embryological significance
Sacrum is an example for block vertebra [6]. The body, posterior arch and transverse process of C2 vertebra is derived from second cervical sclerotome, tip of dens is derived from cranial half of 1st cervical sclerotome [7]. Block vertebra results from embryological failure of normal spinal segmentation due to decrease in local blood supply during the third to eighth week of fetal development. The commonly encountered anomaly is block vertebrae [8], and the common site is C2–C3 with an incidence of 0.4% to 0.7% with no sex predilection [4]. The location of block vertebra in order of frequency are cervical spine (C2-3, C5-6), lumbar spine (L4-5) and thoracic spine (any section) [9]. According to recent report long-standing congenital or acquired fusion of upper cervical vertebrae may lead to stretching and laxity of the ligaments between the occiput and the atlas, resulting in excessive motion and brainstem or cord compression [10].
The presence of block vertebra results in a greater biomechanical stress in the adjoining segments leading to premature degenerative changes at adjoining motion segments. The other common consequences are discal tear, rupture of the transverse ligament, fracture of the odontoid process, and spondylosis [4]. Embryological vascular disorders like subclavian artery supply disruption sequence have been hypothesized to result in Klippel-Feil syndrome [2].
References
- Susan Standring, ed. Gray’s Anatomy. 39th Ed. Elsevier Churchill Livingstone. 2005; 742–744.
- Tiwari A, Chandra N, Naresh M, Pandey A, Tiwari K. Congenital abnormal cervical vertebrae - a case report. J Anat Soc India. 2002; 51: 68–69.
- Erdil H, Yildiz N, Cimen M. Congenital fusion of cervical vertebrae and its clinical significance. J Anat Soc India. 2003; 52: 125–127.
- Soni P, Sharma V, Sengupta J. Cervical vertebrae anomalies-incidental findings on lateral cephalograms. Angle Orthod. 2008; 78: 176–180.
- Sherekar SK, Yadav YR, Basoor AS, Baghel A, Adam N. Clinical implications of alignment of upper and lower cervical spine. Neurol India. 2006; 54: 264–267.
- Congenital vertebral anomaly – Wikipedia, the free encyclopedia. http://en.wikipedia.org/wiki/Congenital_vertebral_anomaly (accessed May 2010).
- Jayanthi V, Kulkarni R, Kulkarni RN. Atlanto-occipital fusion-report of two cases. J Anat Soc India. 2003; 52: 71–73.
- de Graaff R. Congenital block vertebrae C2-C3 in patients with cervical myelopathy. Acta Neurochir (Wien). 1982; 61: 112–126.
- Block vertebra. http://www.e-radiography.net/radpath/b/blockvertebra.htm. (date accessed).
- Yochum T, Chad M. C2 to C3 Congenital Block Vertebra. http://www.theamericanchiropractor.com/articledetail.asp?articleid=75&category=1 (Accessed May, 2010).
Veena Vidya Shankar* and Roopa R Kulkarni
Department of Anatomy, M. S. Ramaiah Medical College, Bangalore, India
- *Corresponding Author:
- Dr. Veena Vidya Shankar, MD
Lecturer, Department of Anatomy, M. S. Ramaiah Medical College, MSRIT post, Bangalore, 560054, India
Tel: +91 80 23605408/408
E-mail: veenavidyashankar@yahoo.com
Date of Received: June 15th, 2010
Date of Accepted: December 19th, 2010
Published Online: January 24th, 2011
© Int J Anat Var (IJAV).2011; 4: 15–16.
Abstract
Skeletal abnormalities at the craniocervical junction or cervical region may result in severe neck pain and sudden unexpected death. During the osteology demonstration of cervical vertebrae for the MBBS Phase I students at M. S. Ramaiah Medical College, it was observed that the axis vertebra is fused with the 3rd cervical vertebra. In this case, the vertebral bodies, vertebral arches and spines were completely fused. This is a condition of block vertebra which has embryological importance and clinical implications.
-Keywords
cervical vertebra, axis, fusion, lamina, pedicle, block vertebra
Introduction
The distinguishing feature of the 2nd cervical vertebra (axis) is presence of odontoid process (dens) which articulates with anterior arch of atlas, and acts as a pivot around which atlas with skull rotates [1]. Severe neck pain and sudden unexpected death may occur due to skeletal abnormalities at the cranio-cervical junction or cervical region and is associated with neurological signs and symptoms [2]. Symptoms vary according to the extent of pathology.
Case Report
During the osteology demonstration of cervical vertebrae for the MBBS Phase I students at M. S. Ramaiah Medical College, it was observed that the axis was fused with 3rd cervical vertebra. The features of this fused cervical vertebrae was analyzed and the specimen was photographed from different aspects.
Observations:
• Body, laminae and spines of C2 and C3 were completely fused on both anterior and posterior aspects.
• Pedicles and transverse processes were not fused.
Foramina transversaria were present, and the diameter in C2 on the left side measured 4.72 mm and on right side 5.71 mm. Foramina transversaria in C3 on the left side measured 6.80 mm and on the right side it was 7.12 mm. The diameters were measured from superior aspect in C2 and from the inferior aspect in C3.
Discussion
Fused cervical vertebrae (FCV) have clinical and embryological importance. The anomalies of cervical region are of interest to anatomists, orthopedists, neurologists, neurosurgeons and even orthodontists. In FCV two vertebrae appear both structurally and functionally as one. This fusion may be congenital or acquired [3].
It is important to identify the cause of FCV – whether it is congenital or acquired or pathologic condition. Acquired FCV is generally associated with diseases like tuberculosis, other infections, juvenile rheumatoid arthritis and trauma. Clinical symptoms may vary from asymptomatic to myelopathy, limitation of the neck movement, or the muscular weakness, atrophy and neurological sensory loss or associated with Klippel-Feil syndrome [3].
The orthodontist may be the first person to detect cervical spine abnormalities as they are asymptomatic until adolescence or young adulthood. Early diagnosis is based on incidental radiographic findings.
According to Farman and Escobar, the radiographic appearance of congenital anomalies of the vertebral bodies may be due to defects in fusion or normal segmentation, occipitalization of the atlas, odontoid and atlas malformations, spina bifida and abnormal ossifications. There is increased incidence of osteophyte formation in the adjacent levels in cervical fusion. Up to 70% of occipitalizations have an accompanying C2–C3 fusion with instability at the C1–C2 articulation [4].
Early diagnosis of these anomalies will be helpful in documenting the change due to an injury, aging, or progression of a degenerative process and also motivates the patients to change their lifestyles to lead a normal life. Surgical intervention for block vertebra carries a higher risk of morbidity and mortality. On the contrary, cervical vertebral fusions are commonly done following traumatic, degenerative and inflammatory dislocations of upper and lower cervical spine [5]. The awareness and monitorization of complications like anesthetic risk during intubation with neck extension needs to be considered. Appropriate counseling on the management of known risk factors, including therapeutic options that can precipitate complication should be encouraged (like avoiding undue trauma, extension and rotational maneuvers which may place the spinal cord and vertebral artery at risk) [4].
Embryological significance
Sacrum is an example for block vertebra [6]. The body, posterior arch and transverse process of C2 vertebra is derived from second cervical sclerotome, tip of dens is derived from cranial half of 1st cervical sclerotome [7]. Block vertebra results from embryological failure of normal spinal segmentation due to decrease in local blood supply during the third to eighth week of fetal development. The commonly encountered anomaly is block vertebrae [8], and the common site is C2–C3 with an incidence of 0.4% to 0.7% with no sex predilection [4]. The location of block vertebra in order of frequency are cervical spine (C2-3, C5-6), lumbar spine (L4-5) and thoracic spine (any section) [9]. According to recent report long-standing congenital or acquired fusion of upper cervical vertebrae may lead to stretching and laxity of the ligaments between the occiput and the atlas, resulting in excessive motion and brainstem or cord compression [10].
The presence of block vertebra results in a greater biomechanical stress in the adjoining segments leading to premature degenerative changes at adjoining motion segments. The other common consequences are discal tear, rupture of the transverse ligament, fracture of the odontoid process, and spondylosis [4]. Embryological vascular disorders like subclavian artery supply disruption sequence have been hypothesized to result in Klippel-Feil syndrome [2].
References
- Susan Standring, ed. Gray’s Anatomy. 39th Ed. Elsevier Churchill Livingstone. 2005; 742–744.
- Tiwari A, Chandra N, Naresh M, Pandey A, Tiwari K. Congenital abnormal cervical vertebrae - a case report. J Anat Soc India. 2002; 51: 68–69.
- Erdil H, Yildiz N, Cimen M. Congenital fusion of cervical vertebrae and its clinical significance. J Anat Soc India. 2003; 52: 125–127.
- Soni P, Sharma V, Sengupta J. Cervical vertebrae anomalies-incidental findings on lateral cephalograms. Angle Orthod. 2008; 78: 176–180.
- Sherekar SK, Yadav YR, Basoor AS, Baghel A, Adam N. Clinical implications of alignment of upper and lower cervical spine. Neurol India. 2006; 54: 264–267.
- Congenital vertebral anomaly – Wikipedia, the free encyclopedia. http://en.wikipedia.org/wiki/Congenital_vertebral_anomaly (accessed May 2010).
- Jayanthi V, Kulkarni R, Kulkarni RN. Atlanto-occipital fusion-report of two cases. J Anat Soc India. 2003; 52: 71–73.
- de Graaff R. Congenital block vertebrae C2-C3 in patients with cervical myelopathy. Acta Neurochir (Wien). 1982; 61: 112–126.
- Block vertebra. http://www.e-radiography.net/radpath/b/blockvertebra.htm. (date accessed).
- Yochum T, Chad M. C2 to C3 Congenital Block Vertebra. http://www.theamericanchiropractor.com/articledetail.asp?articleid=75&category=1 (Accessed May, 2010).