A summary on conjunctival melanoma
Received: 03-Dec-2021 Accepted Date: Dec 17, 2021; Published: 24-Dec-2021
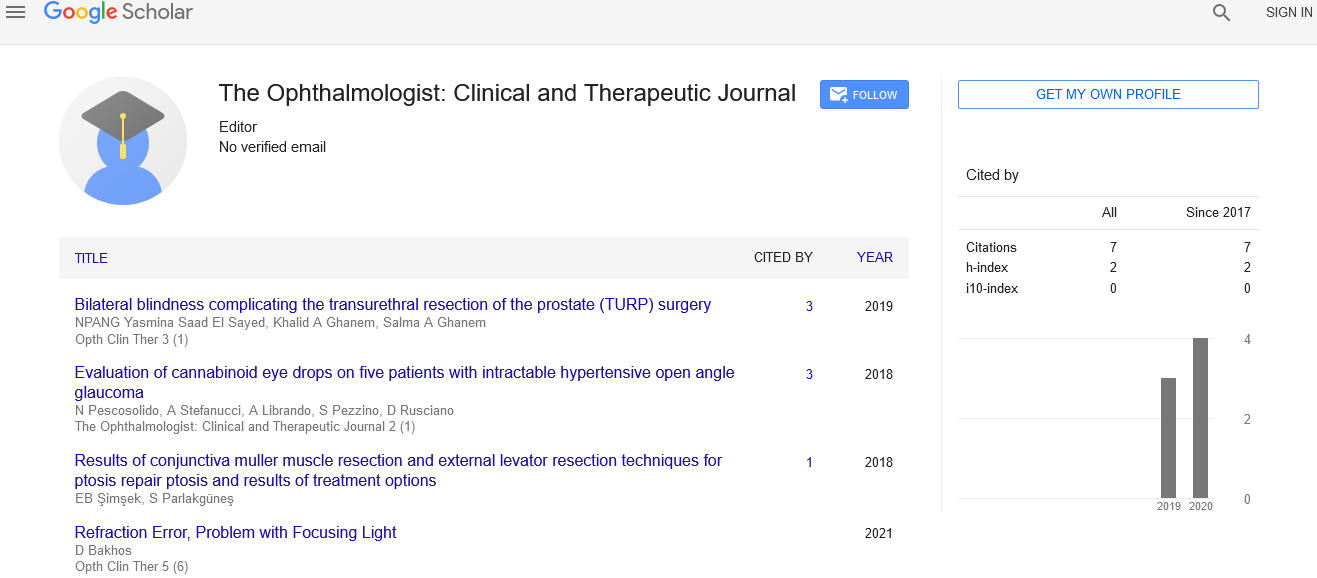
Citation: Phillpotts BA. A summary on conjuctival melanoma. Opth Clin Ther. 2021; 5(6):6.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
About the Study
Conjunctival malignant melanoma appears as a raise pigmente or nonpigmented lesion. Invasive melanoma of the conjunctiva is an uncommon but life-threatening disease of the conjunctiva.Conjunctival melanomas are uncommon tumours that behave aggressively locally. They are most commonly caused by a primary acquired melanosis. Conjunctival melanoma (CM) is a rare malignant tumour that accounts for 5 percentage of all ocular melanomas and has a death rate of up to 30 percentages. Tumour size, extra bulbar placement (fornical or palpebral), or caruncular location, as well as invasion of neighbouring tissues, have all been linked to a high death rate. The treatment of CM is debatable and has largely evolved through medical experience and case series findings. Previously, orbital exoneration was used to treat many individuals with primary conjunctival malignant melanoma. Many primary therapeutic techniques include local excision and cryotherapy, adjuvant topical mitomycin and brachytherapy. Excision without adjuvant therapy and incisional biopsies are discouraged because they appear to be linked to higher tumour recurrence rates, CM metastasis, and CM related death.Local recurrence has been linked to an elevated mortality rate and has been observed toccur in roughly 50 percentage of patients. This is a rare but possibly fatal lesion. It can develop in previously blemished and unpigmented areas (about 10 percentage of instances), from a preexisting nevus (about 20 percentage of cases), or from the flat, spreading pigmentation of primary acquired melanosis with atypia (about 20 percentage of cases) (60 percent -70 percent of cases). Conjunctival melanoma can develop on the bulbar, forniceal, or tarsal conjunctiva, as well as the caruncle, and can develop spontaneously or as a result of pigmented lesions such as PAM or naevi. It accounts for 2 percent to 5 percentage of all ocular cancers and 5 percentage to 7 percentage of all primary ocular melanoma. Constitutive activation of the Ras-Raf-MEK-ERK (MAPK) signalling pathway via somatic activating mutations in BRAF is found in 40 percent of cutaneous melanoma patients. In cutaneous melanoma, BRAF mutations have been linked to a unique clinical appearance and a poor prognosis. As a result, individuals with BRAF- mutated metastatic melanoma who were treated with BRAF and MEK inhibitors had a better prognosis. PAM with atypia is the most common pre-malignant lesion in adults, with a high chance of developing into conjunctival melanoma. The majority of PAM and naevi in children are considered benign and do not proceed to melanoma. Approximately half of the cases in a large series of pediatric conjunctival tumours (n=806) were benign. Pigmented lesions,with naevi and PAM accounting for the bulk, and melanoma accounting for about 2% of all conjunctiva lesions and 3% of all melanocytic tumours. Melanoma was found to be more common in older children (>15 years), to be thicker lesions with wider bases, to have more hemorrhagic areas, and to have less inclusion cysts in this series. Conjunctival tumors observed at a tertiary ocular cancer unit discovered that 3% of all conjunctival melanoma cases were in patients under the age of 20. The majority of the youngsters (median age 11 years) came with pigmented or developing conjunctival lesions, which were diagnosed histologically. Importantly, in several cases, the lesion had been present for several years prior to the assessment, and the change was significant. A change in the size or type of the lesion that necessitated medical intervention Adult conjunctival melanoma is also uncommon with the biggest case series included many patients in a tertiary centre with a median age of 62 years at diagnosis. Malignant melanoma of the conjunctiva is a very uncommon tumor that can create severe morbidity and diagnostic challenges for both ophthalmologists and pathologists.