Abnormalities in airway assessment and it`s relation to difficult endotracheal intubation among elderly patients in Ibrahim Malik teaching Hospital 2022
Received: 04-Jan-2023, Manuscript No. puljedpm-23-6019; Editor assigned: 07-Jan-2023, Pre QC No. puljedpm-23-6019 (pq) ; Accepted Date: Jan 26, 2023; Reviewed: 21-Jan-2023 QC No. puljedpm-23-6019 (Q); Revised: 23-Jan-2023, Manuscript No. puljedpm-23-6019 (R); Published: 27-Jan-2023, DOI: 10.37532/ PULJEDPM. 2023; 6(1):8-14.
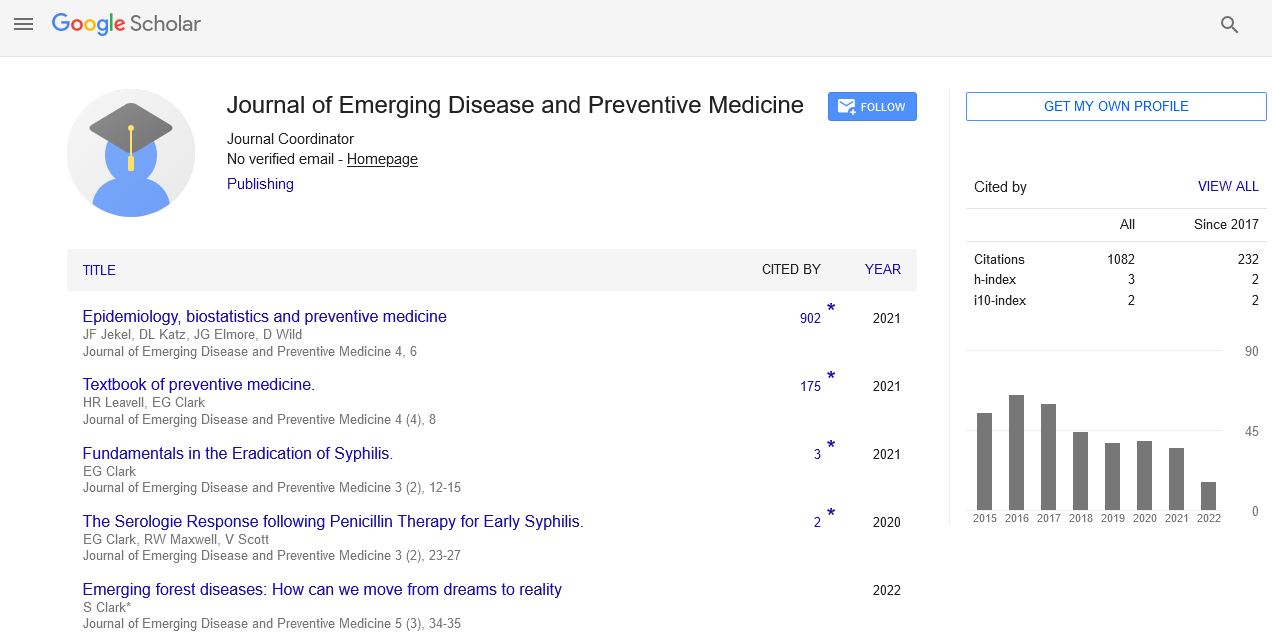
Citation: Ahmed YHE, Yousif IMAB.. Abnormalities in airway assessment and it`s relation to difficult endotracheal intubation among elderly patients in Ibrahim Malik teaching Hospital 2022. J Emer Dis Prev Med 2023;6(1):08-14.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: General anesthesia may need insertion of ETT to secure the airway that may be more difficult to insertion in elderly patients. There are many anatomical, physiological, and cognitive changes that occur in the elderly that affect different components of airway management: intubation, ventilation, oxygenation.
Objectives: this study aim to study the abnormalities in airway assessment and its relation to difficult endotracheal intubation in elderly patients in Ibrahim Malik teaching Hospital 2022
Methodology: This study is an observational cross-section descriptive study it was conducted in Ibrahim Malik teaching hospital, during the period from February 2022 to March 2022, Data was collected by observation using a well-designed questionnaire, Data was entered, cleaned, and analyzed using SPSS 25.0
Results: this study reveal that: the mean age was 67.46 years, and the mean BMI was 26.44 kg/m2, 62% are male and 38% are female, most of them have a mouth opening > 6cm, TMD > 6 cm, SMD > 12 cm, Mallampati score 1, Mandible protrusion Score A, Normal Cervical spine movement, Cooks score class 1. 61% of the doctors notify that the intubation was not difficult, while 39% say it is difficult, the most frequent complications are Hypoxia and Mucosal injury, there is a significant correlation between difficulties in intubation with Mouth opening TMD score SMD score, and Cervical movement, there is a significant correlation between intubation difficulties and presence of complication.
Conclusion: Abnormalities in Airways in elderly are common. TMD, Cervical Spine movement, and Cooks Modified Score have the most important significant value in prediction of intubation difficulties and risk of complications.
Key Words
Anesthesia; Abnormalities; Hypoxia; Mucosal injury
Introduction
Endotracheal intubation is placement of flexible plastic tube into the trachea to maintain an open airway, breathing, oxygenation of the blood, reduce the risk of aspiration and to serves as conduit through which to administer certain drugs [1].
It is frequently performed in critically injured, ill patient with decreased level of consciousness, hypoxia, airway obstruction an anesthetized patient to facilitate oxygenation a ventilation of the lungs, mechanical ventilation and for diagnostic or therapeutic manipulation of the airway may intermittently interfere with the ability to breath. Intubation may be necessary in such situations [1, 2].
According to the Eastern Association for the Surgery of Trauma guidelines, indications for endotracheal intubation include airway obstruction, hypoventilation, severe hypoxemia, sever cognitive impairment (Glasgow coma scale 8 or less), cardiac arrest and sever hemorrhagic shock [3-5].
General anesthesia may need insertion of ETT to secure the airway that may be more difficult to insertion in elderly patients.
There are many anatomical, physiological, and cognitive changes that occur in the elderly that affect different components of airway management: intubation, ventilation, oxygenation.
We can evaluate the airway by taken a history and examining the airway of the patient and additional investigations may be needed. A patient’s medical history or previous medical records may be related to the likelihood of encountering a difficult airway [6-8]. Observational studies of non-selected patients report associations between several preoperative patient characteristics (e.g., age, obesity, obstructive sleep apnea, history of snoring, diabetic patient) and difficult laryngoscopy or intubation and other studies report difficult intubation or extubation occurring in patients with mediastinal masses [7]. Case reports of difficult laryngoscopy or intubation among patients with a variety of acquired or congenital disease states (e.g., ankyloses, degenerative osteoarthritis, subglottic stenosis, lingual thyroid or tonsillar hypertrophy) are also reported [7]. Physical Examination of anatomical features and physical features of head and neck (Mouth opening, thyro-sternomental distance, Mallampatti score, Cervical spine movement, Mandible protrusion) and the likelihood of a difficult airway [9]. The presence of upper airway pathologies or anatomical anomalies may be identified by conducting a pre-procedure physical examination.
The airway history or physical examination may provide indications for additional diagnostic testing in some patients. Observational studies and case reports indicate that certain diagnostic tests (e.g., radiography, computed tomography scans, fluoroscopy) can identify a variety of acquired or congenital features in patients with difficult airways.
The literature does not provide a basis for using specific diagnostic tests as routine screening tools in the evaluation of the difficult airway [9, 10]. The consultants and ASA members strongly agree that airway history, physical examination and should be conducted, whenever feasible, before the initiation of anesthetic care and airway management in all patients and additional evaluation may be indicated in some patients to characterize the likelihood or nature of the anticipated airway difficulty [11]. Anatomical changes occur in different areas of elderly airway from the oral cavity to the larynx. Common changes to the airway include tooth decay, head and neck tumors, goiters, COPD, OSA, Oro-pharyngeal tumors, and decreases in neck range of motion. These changes may make intubation challenging by making it difficult to visualize the vocal cords and place of the endotracheal tube [12]. Patient with tumors or decreased neck range of motion may require a device with more finesse and maneuverability, such as flexible fiber optic Broncho-scope [12, 13]. Difficult intubation also referred to more than three attempts at laryngoscopy or more than 10 minutes of laryngoscopy. Although the definitions are arbitrary, the inability to maintain a patent airway (with or without intubation) may be associated with anoxic brain injury and death. Difficult airway defined as the clinical situation in which a conventionally trained anesthesiologist experience difficulty with tracheal intubation, face mask ventilation of upper airway or both [9,12-15]. The authors state that the ASA task force on management of difficult airway defines difficult tracheal intubation as follows; when proper insertion of the tracheal tube with conventional laryngoscopy requires more than three attempts or more than 10 minutes. That definition belongs to the 1995 ASA guidelines. In 2003 update report the ASA task force has revised the old numerical definition and now define difficult tracheal intubation simply as (requiring multiple attempts) [13]. Repeated airway interventions may potentiate tissue trauma, bleeding and mucosal edema and may transform an airway that cannot (ventilate, intubate) situation [13]. Difficult laryngoscope (it is not possible to visualize any portion of vocal cords after multiple attempts at conventional laryngoscopy).
Difficult tracheal intubation (tracheal intubation requires multiple attempts, in the presence or absence of tracheal pathology).
Failed intubation (placement of the ETT fails after multiple attempts) [16].
The goal of this study is to assess the relation between airway abnormalities and endotracheal intubation in elderly patient and to determine the frequency of the abnormalities.
Problem statement
The elderly population represents a heterogeneous group of individuals with widely varying functional and reserve capacity. Anesthesia of geriatrics associated with increased risk of airway difficulty due to anatomical changes that occur in elderly which affect airway management and it can be one of the causes of mortality. Degradation of the airway along with other physiopathologic and cognitive changes makes the elderly population more prone to complications related to airway management.
Justification
The elderly patient is associated with increased incidence of difficult endotracheal intubation that make the airway management is challenging for anesthesiologist. Good assessments for the airway and good preparation of elderly patients decrease risk of difficult endotracheal intubation so that decrease the mortality rate in the hospital. This study provides an overview of available data of the frequency of abnormalities of elderly airway makes us to focus more on airway assessment to anticipate any difficulty in endotracheal intubation and to prepare the most appropriate equipment for elderly patients and improving the quality of the health system.
Objectives
General objective
To study the abnormalities in airway assessment and its relation to difficult endotracheal intubation in elderly patients in Ibrahim Malik teaching Hospital 2022.
Specific objectives
• To assess the frequency of the airway abnormalities in the elderly patients.
• To measure the Mouth opening, Thyromental distance, Sternomental distance, Mallampatti score, Mandible protrusion, cervical spine movement and Wilson risk score preoperatively.
• To identify the comorbidity of difficult intubation in elderly.
• To identify the complications of difficult endotracheal intubation.
Literature Review
General knowledge
Anatomical and physiological changes of elderly
There are many anatomical, physio-pathological, and cognitive changes that occur in the elderly that affect different components of airway management: intubation, ventilation, oxygenation, and risk of aspiration. Anatomical changes occur in different areas of the airway from the oral cavity to the larynx. Common changes to the airway include tooth decay, oropharyngeal tumors, and significant decreases in neck range of motion. These changes may make intubation challenging by making it difficult to visualize the vocal cords and/or place the endotracheal tube.
Anatomic changes
Nasal cavity
Nasal polyps are significantly more prevalent in adults over 60 years old as compared to those younger than 40 years [17]. Nasal polyps, if present, may make intubation through the nostrils difficult and/or bloody. Not only might a nasal polyp interfere with the placement of a nasopharyngeal airway or nasoendotracheal tube, the airway or tube themselves might cause the polyp to dislodge, which could then obstruct the airway [10]. During oral surgery and for patients with oropharyngeal/laryngeal tumors, nasal intubation is common. Since oropharyngeal tumors are also common in octogenarians, these patients may need to undergo nasal intubation; thus, it is important to ensure that the patients do not have polyps or that the nostril with the polyp is avoided [18].
Oral cavity
The lips are often overlooked in the elderly; however, they are prone to being lacerated due to excessive dryness and fragility. The cutis in the lip thins with age and collagen fibers also begin to separate [19]. This is consistent with the general tendency of the epidermis and dermis to thin with aging. Therefore, it is important to take caution while using laryngoscopes as lip lacerations are common. Accordingly, we recommend using a device with less force, such as a Video Laryngoscope (VL) to minimize lip damage. Additionally, atrophy of the orbicularis Oris muscle occurs with advancing age which might lead to a mild facial droop near the corners of the mouth. This age-related esthetic change could affect BMV as it may be more difficult to create a good face-mask seal about the oral cavity. If ventilation using a conventional bag mask proves to be challenging, a Supralaryngeal Device (SLD), such as a Laryngeal Mask Airway (LMA), may be used.
Pharyngeal/laryngeal
Oropharyngeal cancer is common in elderly patients, especially at the base of the tongue and other tonsillar regions [18]. As a result, it may be difficult to obtain a view of the vocal cords during intubation and/or in actually placing the ETT [20]. These tumors may also be present as masses on the neck, which may decrease the ROM of the neck and the distance between the thyroid notch to the tip of the jaw with the head extended, further challenging the act of direct laryngoscopy [20]. Therefore, use of an SAD such as a lightwand, optical stylet, or FFB to improve maneuverability, or even a VL is recommended.
Obstructive Sleep Apnea (OSA)
Occurs in the elderly due to changes in the pharynx. There is also an increase of parapharyngeal fat accumulation due to aging independent of BMI, which leads to OSA19. It may also make intubation more difficult; therefore, a VL is suggested for better visualization of the vocal cords. In addition, the elderly experience a decrease in the genioglossus negative-pressure reflex, and since the genioglossus muscle is an upper airway dilator which protects pharyngeal patency, any impairment in this muscle or reflex increases the chances of airway obstruction and pharyngeal collapse [21]. As a result, it is recommended that the patient be positioned in reverse Trendelenburg to decrease the amount of force pushing directly down on the posterior pharynx, which prevents an airway collapse. OSA may create an increased risk of desaturation events, so it is imperative that it be closely monitored during airway management, by providing CPAP
Neck
Changes that occur in the neck due to aging include rheumatoid arthritis, myelopathy, and development of thyroid masses, which affect rotation and ROM, making intubation more difficult [22].
Rheumatoid arthritis occurs mostly in the second and third cervical vertebrae, causing ligament destruction, inflammation, swelling of the synovial membrane, and atlantoaxial subluxation, making rotation difficulty [23]. Arthritis is often associated with osteophytes, which can result in neurologic symptoms if they interfere with spinal nerves. As people age, the intervertebral discs begin to lose their supporting capabilities and shrink; thus shortening the distance between the vertebrae [24]. The shortening of the discs puts stress on the cartilage of the vertebrae, causing a decrease in size of the spinal canal. This narrowing puts pressure on the spinal cord resulting in cervical spondylitis myelopathy. This results in stiffness of the neck, and may manifest as pain in the neck, arms, and shoulders [24]. Video laryngoscopy is recommended if there is limited neck ROM, and if there is virtually no motion in the neck; FFB should be used to enhance maneuverability for ETT placement. The incidence of goiters increases in the elderly, and if large enough, may cause thyroid failure [25]. The thyroid plays a role in mental functioning, so a condition that affects the ability of the thyroid to work properly may also affect patient cooperation during airway management. Elderly patients with hypothyroidism are more likely to suffer from myxedema coma.
Physio-pathological changes
Integumentary system
As mentioned in the Oral cavity section, aging results in less collagen fiber production, making the skin thinner and frailer in the elderly. The extracellular matrix within the dermis deteriorates with age, which impairs wound healing and increases bleeding and bruising susceptibility. Scleroderma, an autoimmune disease that occurs in the elderly, is characterized by the hardening and tightening of the skin. It may make it more challenging to open the patient’s mouth for intubation, which may prompt the use of a device that has more flexibility such as an FFB [26]. Patients with Sjogren’s syndrome, eg, characterized by dryness of the eyes and mouth, would also benefit from a video-assisted approach to laryngoscopy.
Cardiovascular system
Progressive stiffening of the arteries and decreases in compliance of the myocardium are natural occurrences of cardiac aging due to the combined effects of glycosylation and deposition of free radicals in collagen and connective tissue, leading to a gradual loss of elasticity. Ventricular compliance is further impaired as systolic BP and pulse wave velocity increase, leading to greater impedance to ventricular outflow which is followed by left ventricular hypertrophy and diastolic dysfunction. Early diastolic left ventricular filling is further impaired by reductions in myocardial relaxation.
Pulmonary system
Besides the aforementioned upper airway dysfunction that predisposes elderly patients to airway obstruction, there are several physiologic changes of the respiratory system associated with aging that may be stressed during airway manipulation upon induction or emergence from anesthesia to be considered. With aging, chest wall compliance decreases due to structural changes of the intercostal muscles, joints, and rib–vertebral articulations that increase the work of breathing.
These changes can lead to fatigue and delayed weaning from mechanical ventilation. Airway resistance increases as the diameter of small airways decrease with age [27]. This leads to air trapping and a greater propensity for developing intraoperative atelectasis. Air trapping and the potential for dynamic hyperinflation during mechanical ventilation might also occur as a result of increases in lung compliance, as lung elastic recoil decreases with advancing age. Importantly, closing volume increases even with normal tidal volume breathing which predisposes these elderly patients to hypoxemia, particularly after induction of anesthesia when mean lung volumes are reduced. Due to increased ventilation/perfusion heterogeneity and decreased diffusing capacity, gas exchange is impaired in elderly patients predisposing them to hypoxemia. Moreover, dysfunction of central chemoreceptors and peripheral chemoreceptors leads to a decrease in hypoxemia and hypercapnic ventilator drive. This can result in a significant increase in susceptibility to opioid-induced apnea, leading to unexpected hypoxemia and hypercapnia. To counteract these predictable changes of aging, preoxygenation for several minutes of 100% oxygen breathing is recommended, particularly to avoid oxyhemoglobin desaturation.
Gastrointestinal system
The elderly tend to have complications with their gastrointestinal tract, especially with their esophagus. In general, there is an association of decreased motility of the esophagus with aging possibly related to the increased incidence of comorbidities (eg diabetes and cognitive issues) that may lead to esophageal diseases. The decreased motility includes slower peristalsis and weaker peristaltic contractions [28]. This allows some substances to remain in the esophagus, rather than transferring completely to the stomach. In addition, it is common for gastric pressure to increase with age, which affects the pressure gradient between the stomach and the esophagus, leading to reflux. The decrease in motility of the esophagus and lower esophageal sphincter pressure both contribute to GERD, a common disease in octogenarians that may lead to aspiration (Figure 1). Due to other issues they present with, GERD’s effects are worse in the elderly population [29]. For instance, the slower peristalsis increases the exposure to acid during reflux. Also, a decrease in saliva secretion worsens the effects of the acid since saliva would help to neutralize the acid.
Figure 1: Anatomical variation in young and elderly.(A) Teeth present and undamaged; (B) thick lips, ability to open mouth widely; (C) long, thick, muscular neck; (D) damaged and missing teeth, thin and fragile lips, inability to open mouth widely; (E) posterior view of oropharyngeal cancer at base of tongue; (F) short, stiff neck; and (G) thyroid mass.
Measures for assessing changes and difficult intubation
The modified Mallampati classification for difficult laryngoscopy and intubation
The modified Mallampati classification is a simple scoring system that relates the amount of mouth opening to the size of the tongue and provides an estimate of space available for oral intubation by direct laryngoscopy. According to the Mallampati scale, class I is present when the soft palate, uvula, and pillars are visible; class II when the soft palate and the uvula are visible; class III when only the soft palate and base of the uvula are visible; and class IV when only the hard palate is visible. The pharyngeal view was determined according to the modified Mallampati method. Patients were instructed to sit upright with the head in the neutral position (Figure 2). Next they were asked to open their mouth fully and maximally protrude their tongue. The observer sat in front of the patient and inspected the pharynx. The classification is based on the structures seen: class 1, soft palate, fauces, uvula, tonsillar pillars; class 2, soft palate, fauces, uvula; class 3, soft palate, base of uvula; class 4, soft palate not visible. Patients with class 3 and 4 of the modified Mallampati score were classified as “predicted difficult.”
Thyromental Distance (TMD)
Measurement is a method commonly used to predict the difficulty of intubation and is measured from the thyroid notch to the tip of the jaw with the head extended. If it is less than 7.0 cm with hard scarred tissues it indicates possible difficult intubation.
Wilson risk score
The Wilson risk sum score was calculated according to multiple anatomical parameters. The measured parameters included head and neck movement, jaw movement (incisor gap and subluxation of the mandible), receding mandible, prominent maxillary incisors, and body weight [30]. Each parameter was graded as 0 risk level–2 risk levels (Figure 3). Patients with a sum of risk levels equal to or greater than 2 were classified as predicted to be difficult to tracheally intubate (“predicted difficult”).
Cooks modified classification
Cormack and Lehane described a classification of the laryngeal view during aryngoscopy. The classification was described to allow simulated difficult intubation. It has been widely adopted and is used by most anaesthetists but is applied inaccurately by the majority. There have been attempts to amend the classification to improve its sensitivity in delineating increasing difficulty with intubation. Yentis recently evaluated a modification in which grade 2 was divided into 2a and 2b.
Methodology
Study area
This study was conducted in Ibrahim Malik teaching hospital which is ocated in Khartoum state. It is one of the biggest governmental and central hospital in Khartoum (Figure 4). This hospital considered among of important referral hospitals in Sudan. Where education opportunities provided for medical students and registrars (Figure 5).
Study duration
This study was conducted during the period from February 2022 to March 2022 (Figure 6).
Study population
Geriatric patients presenting for surgeries under general anesthesia (Figure 7).
Inclusion criteria
• Patients who are schedules for surgery under general anesthesia (Figure 8).
• Elderly patient (age 60 years and more).
• Preoperative assessment.
Exclusion criteria
• Any patient planned for awake fiber-optic intubation.
• Non-cooperative patients (Table 1).
TABLE 1. Table showing how the statistical analysis for the Age and BMI of the study population
| Statistical Analysis | |||||
|---|---|---|---|---|---|
| Maximum | Minimum | Std. Deviation | Median | Mean | |
| 88 | 63 | 6.31042 | 68 | 67.4625 | Age (years) |
| 34.1 | 19.4 | 2.83234 | 26.55 | 26.44 | BMI (Kg/m2) |
• Patients who refused to participate in this study.
• Airway malformation.
Results and Discussion
It is very important to validate the diagnostic accuracy of various airway predictors in elderly patients as they have different anatomy as compared to young adults because of degenerative changes (decreased strength of airway muscles, head and neck joint changes, atrophy of alveolar bone, osteoarthritis) which may result in unanticipated difficult airway. These progressive changes in anatomy of geriatric patients warranted us to calculate the optimal cut-off point of TMD, SMD, Mallampati score and Cooks score, and mouth protrusion for prediction of difficult laryngoscopy by using Receiver Operating Curves (ROC).
The ideal airway predictor should have high sensitivity and specificity with low false NPV. The goal of this study is to assess the relation between airway abnormalities and endotracheal intubation in elderly patient and to determine the frequency of the abnormalities. This study involved 80 elderly patients, most of them have a mouth opening>6cm, TMD>6 cm, SMD>12 cm, Mallampati score 1, Mandible protrusion Score A, Normal Cervical spine movement, Cooks score class 1. The presence of Abnormalities was not that common among study population in which most of them were within normal ranges. This study also reveals that 39% of cases were difficult to intubate according to the intubating doctor in which almost all of them were Registrars either junior or Senior registrars. So here is rising the question: what is the factors associated with difficulties in intubation? To answer this question, I correlated between intubation difficulties and different measures and I found that there is a significant correlation between difficulties in intubation and Mouth opening in which patients with mouth opening<6 cm are more prone to difficult intubation. Also it is significant with TMD score in which when it<6 cm are more prone to difficult intubation. SMD score is highly significant. Moreover; the cervical spine movement also has a significant correlation with intubation difficulties in which the patients with limitation in movement have more intubation difficulties. Cooks Modified score have also a significant correlation in which the higher scores like 3 and 4 have more intubation difficulties. On the other hand, there was no significant correlation with both Mallampati score and Mandible protrusion. These findings agree with the findings of Pratibha Panjiar whom emphasized the accuracy and sensitivity of TMD in assessing the difficulties in intubation. And from this point we can deduce that: Mouth opening, SMD, TMD, Cervical spine movement, and Cooks score have more sensitivity for intubation difficulties than other measures like Mallampati score and mandible protrusion. In More than that in this study I found that there is a significant correlation between intubation difficulties and presence of complication. Logically the difficulty in intubation is associated with increase the number of attempts, forceful intubation which increase the risk if complication. The presence of Complication was also significant with the TMD, Cervical Spine movement, and Cooks Modified Score. This finding support the previous deduction in which measures or score have the most important significant value in prediction of intubation difficulties and risk of complications.
Conclusion
From this study we can conclude that abnormalities in airways in elderly are common. TMD, Cervical Spine movement, and Cooks Modified Score have the most important significant value in prediction of intubation difficulties and risk of complications.
References
- Kheterpal S, Healy D, Aziz MF, et al. Incidence, predictors, and outcome of difficult mask ventilation combined with difficult laryngoscopy: a report from the multicenter perioperative outcomes group. Anesthesiology. 2013;119(6):1360-9.
- Apfelbaum JL, Hagberg CA, Caplan RA, et al. American Society of Anesthesiologists Task Force on Management of the Difficult Airway Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2013;118(2):251-70.
- Amathieu R, Combes X, Abdi W, et al. An algorithm for difficult airway management, modified for modern optical devices (airtraq laryngoscope; LMA CTrach™) a 2-year prospective validation in patients for elective abdominal, gynecologic, and thyroid surgery. J Am Soc Anesthesiol. 2011;114(1):25-33.
- Kheterpal S, Han R, Tremper KK, et al. Incidence and predictors of difficult and impossible mask ventilation. J Am Soc Anesthesiol.2006;105(5):885-91.
- Kheterpal S, Martin L, Shanks AM, et al. Prediction and outcomes of impossible mask ventilation: a review of 50,000 anesthetics. J Am Soc Anesthesiol. 2009 ;110(4):891-7.
- Shiga T, Wajima ZI, Inoue T, Sakamoto A. Predicting difficult intubation in apparently normal patients: a meta-analysis of bedside screening test performance. J Am Soc Anesthesiol. 2005; 1;103(2):429-37.
- Yentis SM. Predicting difficult intubation--worthwhile exercise or pointless ritual?. Anaesthesia. 2002 1;57(2):105-9.
- Freundlich RE, Kheterpal S. Perioperative effectiveness research using large databases. Best Pract Res Clin Anaesthesiol. 2011 1;25(4):489-98.
- Kheterpal S. Clinical research using an information system: the multicenter perioperative outcomes group. Anesthesiol clinics. 2011 1;29(3):377-88.
[GoogleScholar] [CrossRef]
- Samsoon GL, Young JR. Difficult tracheal intubation: a retrospective study. Anaesthesia. 1987;42(5):487-90..
- El-Orbany M, Woehlck HJ. Difficult mask ventilation. Anesthesia & analgesia. 2009;109(6):1870-80.
- Han R, Tremper KK, Kheterpal S, et al. Grading scale for mask ventilation. J Amer Soc Anesthesiol. 2004;101(1):267.
- Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia. 1984; 39(11):1105-11.
- Harrell Jr FE, Lee KL, Matchar DB, et al. Regression models for prognostic prediction: advantages, problems, and suggested solutions. Cancer treatment reports.1985;69(10):1071-7.
- Langeron O, Masso E, Huraux C, et al. Prediction of difficult mask ventilation. J Amer Society Anesthesiol .2000;92(5):1229-36.
- Aziz M. Use of video-assisted intubation devices in the management of patients with trauma. Anesthesiol clinics.2013;31(1):157-66.
- Johansson L, Åkerlund A, Melén I, et al. Prevalence of nasal polyps in adults: the Skovde population-based study. Annals Otol, Rhinol & Laryngol. 2003; 112(7):625-9.
- Warnakulasuriya S. Global epidemiology of oral and oropharyngeal cancer. Oral oncology. 2009;45(4-5):309-16.
- Penna V, Stark GB, Eisenhardt SU, et al. The aging lip: a comparative histological analysis of age-related changes in the upper lip complex. Plastic reconst surgery. 2009;124(2):624-8.
- Matioc AA, Olson J. Use of the laryngeal tube in two unexpected difficult airway situations: lingual tonsillar hyperplasia and morbid obesity.d Can J Anaesth. 2004; 51(10):1018-21.
- Tuang GJ, Nik Hussin NR, Zainal Abidin ZA. Unilateral rhinorrhoea and button battery: a case report. Fam Med Com Health. 2019;7: 000137.
- Popitz MD. Anesthetic implications of chronic disease of the cervical spine. Anesthesia & Analgesia. 1997 ;84(3):672-83.
- Young WF. Cervical spondylotic myelopathy: a common cause of spinal cord dysfunction in older persons. American family physician. 2000;62(5):1064-70.
- Mariotti S, Franceschi C, Cossarizza A, et al. The aging thyroid. Endocrine reviews. 1995; 16(6):686-715.
- Li Y, Lei D, Swindell WR, et al. Age-associated increase in skin fibroblast–derived prostaglandin E2 contributes to reduced collagen levels in elderly human skin. J Invest Dermatol. 2015;135(9):2181-8.
- Schachna L, Wigley FM, Chang B, et al. Age and risk of pulmonary arterial hypertension in scleroderma. Chest.2003;124(6):2098-104.
- Groban L. Diastolic dysfunction in the older heart. J cardioth vascul anesthesia. 2005;19(2):228-36.
- Chiam B, Sin DD. The aging lung: Implications for diagnosis and treatment of respiratory illnesses in the elderly. Geriatr Aging. 2002;9(5):36-40.
- Cardus J, Burgos F, Diaz O, et al. Increase in pulmonary ventilation–perfusion inequality with age in healthy individuals. Amer J respiratory and critical care medicine. 1997;156(2):648-53.
- Scobey MW, Castell DO. Esophageal Motility: Effects of Collagen Vascular Diseases and Aging. Gastroenterol Nursing. 1986 ;8(4):16-21.