Contusive retinal tear secondary to blunt trauma: A rare case report
Received: 12-Feb-2021 Accepted Date: Feb 26, 2021; Published: 05-Mar-2021
Citation: Adusumilli H. Contusive retinal tear secondary to blunt trauma: A rare case report. Opth Clin Ther. 2021;5(2):6-7.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Peripheral retinal tears can occur secondary to blunt trauma can be divided into typical or horse shoe and atypical or irregular shaped. A type of atypical tear is a stretch tear located anterior to equator, radial, irregular and wedge shaped configuration, postulated to occur due to rapid horizontal expansion of eye ball due to coup injury. A 30 year old sustained blunt ocular trauma to the left eye with visual acuity 20/200. Examination showed a large radial wedge shaped retinal tear in temporal periphery exposing the underlying bare choroid extending close to the equator with no associated retinal detachment. This case is unique due to the shape and orientation of the tear and such radial tears are rarely described in literature.
Keywords
Closed globe injury; Horizontal retinal tear; Retinal necrosis; Atypical retinal tear
Introduction
Horizontal stretch tears of retina secondary to contusive type of closed globe injuries are very rare but theoretically described [1]. Cox MS et al. in their study about the retinal breaks due to blunt trauma at the point of impact postulated various mechanisms about the irregular retinal tears and the multifactorial mechanisms involved including retinal necrosis at the site of impact [2]. In these cases the traumatic retinal tears were irregular and primarily a result of pathology which is caused by a combination of fragmentation and mechanical tissue disruption at the site of impact. Longstaff et al. in 1987 reported a case of retinal break in superior quadrant secondary to retinal necrosis in a countercoup trauma due to blunt trauma [3]. To our knowledge this is one of the few case reports that highlight retinal necrosis due to coup injury and subsequent radially oriented retinal break following a closed globe injury.
Case History
A 30 year old male, complained of diminished vision in the left eye of 3 days duration following trauma sustained to left eye during a fall from motor bike. Other than eye, there was no history of injuries elsewhere in the body. His systemic history was unremarkable. His visual acuity was 20/20 in the right eye and 20/200 in the left eye. His intraocular pressure with noncontact tonometry was 11 and 13 mm of Hg. Ocular examination showed peri-orbital edema and ecchymosis on the left ocular adnexa. Orbital rim and margins were palpable with no evidence of any fracture. Extra-ocular movements were full and painless. Pupillary light reflex was normal. Slit lamp examination showed subconjuctival hemorrhage more prominent in the temporal conjunctiva and extending nasally. Cornea and lens were clear, anterior chamber was well formed with no reaction. Anterior vitreous face was normal.
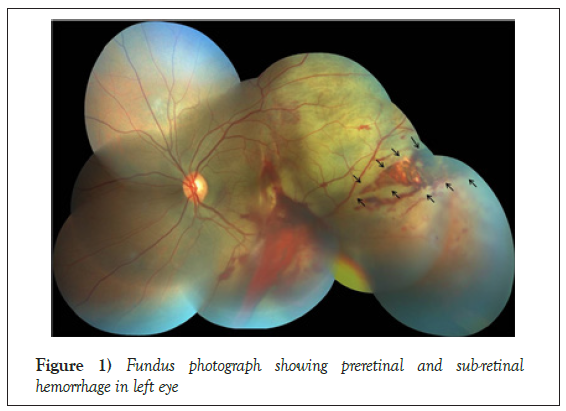
Fundus examination was done with indirect ophthalmoscopy and 90 D lens with slit lamp. Vitreous showed inferior streak vitreous hemorrhage. Optic disc was normal with CD ratio of 0.3. Posterior pole showed area of commotion retinae, sub foveal hemorrhage with vertical choroidal rupture involving the macula and posterior pole. Extensive pre retinal hemorrhages were seen over the posterior pole and temporal retina. Severe commotion retinae extending temporal 180 degree of the fundus extending till periphery suggested by the grey white opacification of the outer retina (Figure 1).
Peripheral retinal examination showed significant commotion retinae, retinal edema with a large radial, wedge shaped, horizontal retinal tear in temporal periphery exposing the underlying bare choroid and extending posteriorly till the equatorial region (Figure 1). No associated retinal detachment was noted. The diagnosis of left eye: closed globe injury; Grade B, Zone 3 was done as per Birmingham Eye Trauma Terminology (BETT) [4].
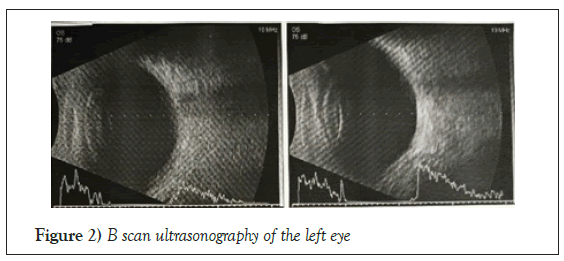
Patient was advised for orbital imaging to rule out any fracture or intraocular foreign body despite of being a closed globe injury due to the atypical retinal tear. He underwent B scan ultrasonography of the left eye which showed no evidence of retinal detachment (Figure 2). He was advised for barrage laser photocoagulation to the horizontal retinal tear. He was started on topical antibiotic and corticosteroid combination 6 times in a day and oral corticosteroids (1 mg/kg body weight) tapering dosage. He was advised a follow up 2 weekly to monitor for the risk of development of retinal detachment and need for surgical procedure in the left eye.
Results and Discussion
Traumas from blunt and sharp objects are among the two major causes for severe ocular injuries. Retina and vitreous are second only to cornea as the most frequently involved ocular tissue in these types of injuries. Posterior segment injuries and their sequelae can cause severe and permanent visual morbidity. 31% of all serious injuries have retinal involvement and among these, 34% are closed globe injuries [5]. Rate of combined vitreo-retinal involvement among all serious injuries was found to be 44%. Blunt objects are the most common source of closed globe injuries ranging around 30% [5].
In closed globe injuries, the resulting damage can be explained by a four mechanisms. They are compression, decompression, over fitting and oscillations [5].
The most common retinal defects in this type of injury are retinal dialysis and peripheral retinal tear secondary to frictional forces that are generated at the vitreous base due to rapid increase in the equatorial globe diameter. Vitreous body being inelastic causes traction during the globe compression resulting in base avulsion where the anterior border is ripped off from the retina or pars plana. This is commonly described as compression-decompression injury.
Second mechanism is the coup injury. Local trauma at the site of impact on the sclera induces a direct concussive and full-thickness necrosis of the overlying retina resulting in a large retinal tear and the directionality depends on the site of scleral impact [2,6]. This explains the atypical horizontal tear that occurred in our case, where the impact of trauma was on the temporal aspect resulting in a horizontal retinal tear at 3 o’clock position extending horizontally towards the posterior pole [2,7].
The other two common mechanisms are abnormal vitreo-retinal traction and sudden induction of posterior vitreous detachment. In the present case however the cause for the retinal break is primarily the acute edema and necrosis. There was no posterior vitreous detachment in this case which explains the lack of retinal detachment at acute presentation. However these cases need to be monitored for the development of retinal detachment in the subsequent weeks due to induction of posterior vitreous detachment. The presence of commotion retinae surrounding the area of retinal tear might reduce the visibility of laser burns. To ensure adequate barrage photocoagulation, an area of retina where the visible laser marks can be obtained surrounding the tear can be utilized to complete the laser photocoagulation. Additional augmentation laser may be required in some cases.
Declaration of Patient Consent
The authors certify that they have obtained the appropriate patient consent form. The patients understand that their names and initials will not be published with strict concealment of their identity.
Financial support and sponsorship
Nil.
Conflict of Interest
No conflict of interests.
Ethics of Human and Animal Experiments
Informed consent was obtained. Protocol was approved by the institutional review committee.
REFERENCES
- Kuhn F, Pieramici DJ. Ocular Trauma, Principles and Practice. Thieme Publishers. 2002; p215-216.
- Cox MS. Retinal breaks caused by blunt nonperforating trauma at the point of impact. Trans Am Ophthalmol Soc. 1980; 78: 414-466.
- Longstaff S, Baines PS, Roxburgh ST. Retinal break formation following contrecoup trauma: Case report. Br J Ophthalmol. 1987; 71: 375-376.
- Pieramici DJ, Paul Sternberg, Thomas M, et al. A system for classifying mechanical injuries of the eye (globe). Am J Ophthalmol. 1997; 123: 820-831.
- Kuhn F, Morris R, Witherspoon D, et al. A standardized classification of ocular trauma. Ophthalmology.1996; 103: 240-243.
- Weidenthal DT, Schepens CL. Peripheral fundus changes associated with ocular contusion. Am J Ophthalmol.1966; 62: 465-477.
- Blight R, Hart JC. Structural changes in the outer retinal layers following blunt mechanical non-perforating trauma to the globe: An experimental study. Br J Ophthalmol. 1977; 61: 573-587.