Measuring blood glucose in a non-invasive manner based on nearinfrared and automatically sending information to the medical center
2 Student, Department of Biomedical Engineering, Sheikhbahaee University, Iran, Email: mahtab.khanahmadi@shbu.ac.ir
Received: 21-Feb-2018 Accepted Date: May 30, 2018; Published: 08-Jun-2018
Citation: Shirzadfar H, Khanahmadi M. Measuring blood glucose in a non-invasive manner based on near-infrared and automatically sending information to the medical center. Biomed Engg Cur Res. 2018;1(1): 01.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Introduction
Diabetes mellitus is a type of metabolic disorder that causes blood sugar to rise. In this type of disease, insulin is insufficient in the body or insulin cannot function. The insulin hormone secretes by the beta cells in the pancreas, which reduces the sugar. Diabetes mellitus has early-onset complications such as diabetic ketoacidosis, hyperglycemic, hypoglycemic and Hyperosmolar coma, and over time it causes cardiovascular disease, nephropathy, retinopathy and neuropathy [1]. Diabetes is divided into four categories: type 1, type 2, pregnancy, and certain types of diabetes. In type 1 diabetes, insulin-producing cells are damaged by the immune system, which means patients do not produce insulin in their bodies. Insulin is produced in type 2 diabetes, but its amount is not enough or the body resists insulin. Type 1 diabetes can be detected using randomized blood sugar, fasting blood sugar and oral glucose tolerance testing [2]. The number of people with diabetes will reach 438 million by 2030 [3]. So measuring blood glucose in today’s society is very important with this number of patients.
Blood glucose measurement methods are divided into invasive and noninvasive methods. Invasive methods such as sampling a patients blood and a glucometer device with a finger piercing. These methods are painful and can cause infectious diseases. Therefore, non-invasively and continuously blood glucose measurement methods were developed. Non-invasive methods such as optical methods, microwave waves, epic health apps, freestyle libre patches, body-sweats, teardrop and saliva measurements. Optical methods include: Infrared spectroscopy, Raman spectroscopy, photoacoustic, fluorescence, polarimetric, and so on.
Using an infrared LED, the wavelength radiates to the body close to infrared range, and the reflected light from the body is absorbed by a photodiode sensor, and the blood glucose level is determined which is based on comparison of radiation intensity before and after interactions [4].
In Raman spectroscopy, a laser light source, an optical probe, a spectrometer [5,6] and a computer are needed. The laser light radiates on the body, and then the Raman Effect is generated, causing diffusing scattered and recessive Raman light to the probe, then focuses on the fiber optic cable, and then the light is sent to the spectrometer, that is divided to separated wavelengths and appears on CCD (charge-coupled devices) camera. The basis of its work is the elasticity of photon scattering [3].
In a photo-acoustic method, light is absorbed by the subject in terms of its optical properties and stimulates subject’s molecules. The absorbed energy is released in the form of heat, causing the sample volume to expand, which causes to form a pressure wave that depends on the optical and physical properties of the sample. The amount of glucose is determined through stimulated wavelengths associated with glucose molecules. In general, the basis of this method is the conversion of optical energy to acoustic energy [7].
The fluorescence method is based on the diffusion of light from molecules in different states. This method is fast and does not require a reactive and it is very sensitive. In another method, you can measure blood glucose using body sweat. In this method, a paper biosensor has an enzymatic fuel cell. This label is placed exactly on the skin and stores the sweat in a container and then converts its chemical energy into electrical energy, which can be used to control the blood sugar in the sweat [8,9].
One of the methods of non-invasive blood glucose measurement is the use of microwave waves. A microwave reflector, which includes a voltage control oscillator and two semiconductor interference couplers, with connectors and detectors connected to a microcontroller. These microwave waves have been attenuated to 1000 times to not have detrimental effects on people [10].
The freestyle libre patch has a very small sensor 0.2 inches (about a thickness of a hair) that is embedded under the skin and connected to a plastic patch that is resistant to water. By placing it on the arm, it starts reading glucose amounts after an hour. By holding a touch-screen reader on the front of the patch, glucose levels are displayed on the device at the same time and a chart of blood glucose levels is plotted on the device over the last eight hours [11,12].
In different methods, you should refer to the physician and show the results to the physician in order to check the information and give the patient the appropriate medication and diet for continuing the treatment. But this method has a lot of problems. For example, in an emergency, the patient can not immediately contact his doctor or when they receive insulin for constant control of their blood sugar, they have to be admitted to the hospital, which will take time and money and that the hospital is the place where various diseases are transmitted to those who are admitted there.
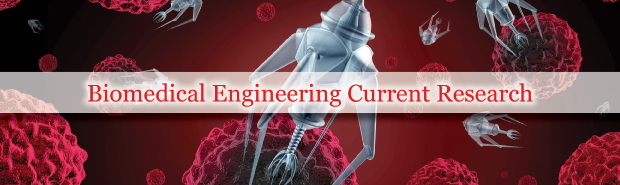
In the future, in the relevant project, we plan to provide a non-invasive measurement method that measures blood glucose levels continuously and, in addition, measures and evaluates other parameters from the patient’s body, and at the same time notifies the doctor and even the patient’s relatives and the doctor’s instructions are sent as a message on the patient panel that is on the mobile phone and a real-time two-way communication between the patient and the doctor will be created, the block diagram of this method is shown in (Figure 1).
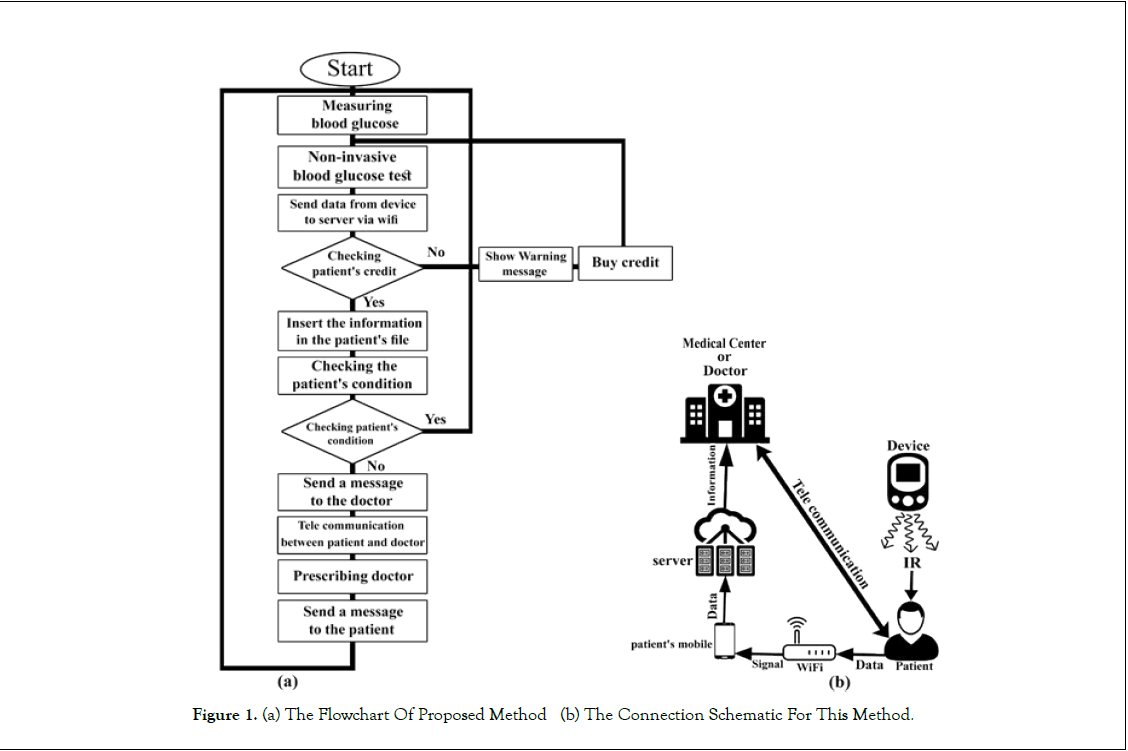
First, we use an optical diode with near infrared radiation (NIR) to measure blood glucose. The light is radiated to the finger, then the reflection light collides with an optical sensor and converts it to a voltage through the transducer and, based on this voltage, a signal will be created, and filtered and amplified. It then converts to a digital and specific value by analog-to-digital converter (A/D). These values are analyzed by microcontroller, and blood glucose level is predicted, the block diagram of this device is shown in (Figure 2). After measuring blood glucose, the values are automatically transferred through a Wi-Fi connection to the server and stored there and sent as an alert for the doctor’s user panel. Doctor will send an online prescription according to the blood glucose and meals, which will be displayed on the patient’s panel. Here it is possible to communicate bilaterally and online between patient and doctor.
Because this method measures blood glucose in a non-invasive method does not transmit infectious and contagious diseases, and also does not cause ulcers or pain in the patient’s body. It also facilitates communication between the patient and the doctor, and the patient communicates with the doctor remotely and his treatment is more quickly and accurately, saves the time and expenses and makes the diabetic patient more relaxed.
REFERENCES
- Fulvio Pomero, Matteo Nicola Dario Di Minno, Luigi Fenoglio, Monica Gianni, Walter Ageno, Francesco Dentali. Is diabetes a hypercoagulable state? A critical appraisal. 2015.
- American Diabetes Association. Classification and Diagnosis of Diabetes.2016.
- M.S. Wróbel. Non-invasive blood glucose monitoring with Raman spectroscopy: prospects for device miniaturization.2016
- Komal Lawand, Mahesh Parihar, Shital N.Patil. Design and Development of Infrared LED Based Non Invasive Blood Glucometer.2015
- Shirzadfar, H., Claudel, J., Hauet, T., Nadi, M., Yamada, S., Kourtiche, D., “Caractérisation d’un biocapteur à base de GMR pour la spectroscopie magnétique sur ferrofluide”, Materiaux et Applications aux Dispositifs et Capteurs, Poster presentation, November 7-9, 2012, Sousse, Tunisie.
- Claudel, J., Ibrahim, M., Shirzadfar, H., Nadi, M., Elmazria, O., Kourtiche, D., “Hybrid Microfluidic Biosensor for Single Cell Flow Impedance Spectroscopy: Theoretical Approach and First Validations”, XIII Mediterranean Conference on medical and biological engineering and computing (MEDICON 2013), Poster presentation, September 25-28, pp. 841-844, Vol. 41, Springer International Publisher, 2013, Seville, Spain.
- Praful P. Pai, Pradyut K. Sanki, Swapna Banerjee. A Photoacoustics based Continuous Non-Invasive Blood Glucose Monitoring System.
- Rujuta D. Munje, Sriram Muthukumar, Shalini Prasad. Lancet-free and label-free diagnostics of glucose in sweat using Zinc Oxide based flexible bioelectronics.2017
- Joseph Wang. Electrochemical Glucose Biosensors.2008
- Maximilian Hofmann, GeorgFischer, Robert Weigel, Dietmar Kissinger. Microwave-Based Noninvasive Concentration Measurements for Biomedical Applications.2013
- https://www.freestylelibre.co.uk/libre/
- https://diatribe.org/abbott-freestyle-libre-transforming-glucose-monitoring-through-utter-simplicity-fingersticks#How%20FreeStyle%20Libre%20Works