RELATIONSHIP BETWEEN RIGHT VENTRICULAR SYSTOLIC FUNCTION, MEAN PULMONARY ARTERIAL PRESSURE AND LEFT VENTRICULAR EJECTION FRACTION IN HYPERTENSIVE HEART FAILURE PATIENTS SEEN AT THE OBAFEMI AWOLOWO UNIVERSITY TEACHING HOSPITALS COMPLEX, ILE-IFE
2 Department of Medicine, Obafemi Awolowo University Teaching Hospital Complex, Ile-Ife, Osun State, Nigeria
Received: 27-Dec-2022, Manuscript No. PULCJ-22-6001; Editor assigned: 29-Dec-2022, Pre QC No. PULCJ-22-6001 (PQ); Reviewed: 12-Jan-2023 QC No. PULCJ-22-6001; Revised: 22-Mar-2023, Manuscript No. PULCJ-22-6001 (R); Published: 30-Mar-2023
Citation: Atendi AB, Ogunyemi SA, Adebayo RA, et al.. Relationship between right ventricular systolic function, mean pulmonary arterial pressure and left ventricular ejection fraction in hypertensive heart failure patients seen at the obafemi awolowo university teaching hospitals complex, Ile-Ife. Clin Cardiol J 2023;7(1):1-6.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: The role of the Right Ventricle (RV) has been largely underestimated compared to left ventricle in cardiac diseases. Nowadays the importance of RV has been recognized as independent risk factor for mortality in heart failure. Elevated mean Pulmonary Arterial Pressure (mPAP) is also a recognized independent predictor in heart failure patients. There is a scarcity of data evaluating this relationship in heart failure patients in sub-Sahara Africa. This study was therefore designed to establish the relationship between RV systolic function, Left ventricular ejection fraction and mPAP in hypertensive heart failure patients in Obafemi Awolowo university teaching hospitals complex.
Methodology: Eighty patients with heart failure secondary to hypertension and 80 normal controls underwent clinical, electrocardiographic and echocardiographic evaluation. Indices of right ventricular systolic function that were measured include Tricuspid Annular Plane Systolic Excursion (TAPSE), and Right Ventricular Myocardial Performance Index (RVMPI) and mPAP was derived from RV outflow tract acceleration time after pulse interrogation at level of pulmonary valve.
Results: forty two (52.5%) and 22 (27.5%) heart failure patients had right ventricular systolic dysfunction and right ventricular global dysfunction respectively as measured by TAPSE and RVMPI. Elevated mean pulmonary artery pressure was found in 38 (47.5%) of the hypertensive heart failure patients. There was no relationship between the indices of right ventricular systolic function and the estimated mean pulmonary artery pressures. There were also no significant relationships between left ventricular ejection fraction and estimated mPAP. The independent predictor of right ventricular systolic dysfunction was the LV ejection fraction.
Conclusion: Right ventricular systolic function is impaired in patients with heart failure secondary to hypertensive heart disease. There is no relationship between the indices of right ventricular systolic function and mean pulmonary artery pressure. Further studies are needed to assess right ventricular systolic function in Nigerians.
Keywords
Heart failure; Hypertension; Nigeria; Right ventricular dysfunction; Sub-Saharan Africa
Introduction
Heart failure is a major public health problem affecting approximately 26 million patients worldwide.
There had been a tremendous improvement in the prevention, diagnosis and management of heart failure patients; however, outcome is still suboptimal. Therefore, identification of other predictors of mortality in heart failure patients is rapidly evolving as an area of extensive research. Studies have shown right ventricular dysfunction as independent predictors of exercise tolerance and mortality in heart failure patients. Pulmonary hypertension is also increasingly recognized as an important predictor of mortality in heart failure patients.
There have been conflicting reports about the relationship between RV function and pulmonary hemodynamics in heart failure patients and most of these studies were carried out in Caucasians with scarcity of data from sub-Sahara Africa.
Hypertensive Heart Failure (HHF) had been reported in many studies in Sub-Sahara Africa as the commonest cause of heart failure in contrast to ischemic heart disease and diabetes mellitus as major causes of heart failure in the Caucasians.
The advent of reliable and reproducible echocardiographic measures of RV function such as Tricuspid Annular Plane Systolic Excursion (TAPSE), RV Myocardial Performance Index (MPI) had made the assessment of RV function in cardiac diseases easier and helped identify the important role of RV in HF subjects.
Therefore, we undertook this study to evaluate right ventricular function, pulmonary hypertension as well as their relationship in hypertensive heart failure subjects in relation to their left ventricular ejection fraction [1-3].
Materials and Methods
This study was carried out at the Obafemi Awolowo university teaching hospitals complex, Ile-Ife Osun state. The study protocol was approved by the ethics committee of the hospital and each participant signed an informed consent form in accordance with the declaration of Helsinki. The study was cross sectional in design [4,5].
Eighty patients with heart failure secondary to hypertensive heart disease and 80 apparently healthy controls were recruited using the simple random technique. The exclusion criteria among subjects with heart failure included those with heart failure due to etiology other than hypertension even if coexisting with hypertension, co-morbidities such as ischemic heart disease/ myocardial infarction, diabetes mellitus, thyroid disease, chronic kidney disease, anaemia, asthma and Chronic Obstructive Pulmonary Disease (COPD). Other exclusion criteria among subjects and controls included pregnancy, current smokers, significant alcohol use of more than 14 units per week for women and 21 units per week for men, gout, poor echocardiographic window and refusal to give consent [6-8].
Echocardiographic studies
Trans thoracic echocardiography was performed using a general electronics vivid T8 cardiac ultrasound system on all subjects and controls in the left lateral decubitus position and measurements were taken according to the recommendations of the American society of echocardiography and European society of echocardiography. Measures of right ventricular systolic function evaluated included Tricuspid Annular Plane Systolic Excursion (TAPSE) which was acquired by placing an M-mode cursor through the tricuspid annulus, in the apical four chamber view, and measuring the amount of longitudinal excursion of the annulus at peak systole and Right Ventricular Myocardial Performance Index (RVMPI) which was also acquired by tissue doppler pulse interrogation of the tricuspid lateral annulus, in the apical four chamber view and measuring the ratio of the sum of isovolumic periods (isovolumic relaxation time plus isovolumic contraction time) to ejection fraction of Right Ventricle (RV). TAPSE <1.6 was taken as impaired RV systolic function, and value of RVMPI >0.55 as impaired RV global dysfunction [9,10].
Pulmonary hypertension was derived from the mean Pulmonary Arterial Pressure (mPAP) which is estimated from the Acceleration Time (AT) during pulse doppler interrogation of the right ventricular outflow tract just proximal to pulmonary valve at the parasternal short axis view. mPAP was then calculated using the regression equation by Dabestani, et al., which is 90-(0.62*AT). However, in patients with heart rate >100 beats per min, or <70 beats per min, the formula was corrected for by multiplying AT by 75, and dividing it by the heart rate of the patient to improve its accuracy. Value greater than or equal to 25 mmHg was taken as pulmonary hypertension [11].
Data management and analysis
Data was analysed using international business machines statistical software version 24. Data were presented using descriptive statistics such as tables. Categorical variables were represented as proportions and percentages. Normally distributed numerical data was expressed as mean ± standard deviation; while skewed numerical data was expressed as median+(Inter-Quartile Range (IQR).
The Shappiro-Wilk's test was used to test for normality. Student's ‘t’ test, or the Mann Whitney's test (non-parametric testing for non-nominal data) were used to test for the differences in the continuous variables between the two groups while chi-squared analysis was used to test for the differences in the categorical variables between the groups. Pearson's correlation was used to evaluate the bivariate relationship between the parameters of RV systolic function, mPAP and some clinical and echocardiographic indices. A stepwise logistic regression model was used to determine the independent correlates of RV systolic dysfunction. A two tailed p-value of <0.05 was considered significant [12-15].
Results
Eighty subjects with hypertensive heart failure and eighty apparently healthy subjects were studied.
Demographic characteristics of study participants
Table 1 showed the clinical characteristics of the study subjects. HHF subjects were matched for age and sex with healthy controls in a ratio of 1:1.
Body mass index, systolic blood pressure and diastolic blood pressure were significantly higher in HHF patients compare to control.
| Characteristics | HHF cases (n=80) | Controls (n=80) | Statistical indices | |||
|---|---|---|---|---|---|---|
| Age in years | n | % | N | % | ||
| <55 | 10 | 12.5 | 10 | 12.5 | χ2=0.024 | |
| 55-64 | 38 | 47.5 | 39 | 48.8 | p=0.986 | |
| ≥ 65 | 32 | 40 | 16 | 32 | ||
| Mean ± SD | 62.03 ± 6.4 | 61.33 ± 5.8 | P=0.474 | |||
| Gender | ||||||
| Male | 38 | 47.5 | 38 | 47.5. | χ2=0.000 | |
| Female | 42 | 52.5 | 42 | 52.5 | p=1.000 | |
| Wt (Kg) | 70.0 (64.0-80.0) | 68 (65.0-72.0) | 0.052 | |||
| Ht (m) (mean ± SD) | 1.67 ± 0.1 | 1.69 ± 0.1 | 0.021 | |||
| BMI (kg/m2) | 24.37 (23.39-28.40) | 23.50 (22.40-24.68) | <0.001 | |||
| SBP (mmHg) | 120.0 (110.0-140.0) | 110.0 (100.0-120.0) | <0.001 | |||
| DBP (mmHg) | 80.0 (80.0-90.0) | 77.5 (70.0-80.0) | <0.001 | |||
| NYHA functional classification | ||||||
| Mild limitation of physical activity (Class II) | 35 | 43.6 | ||||
| Marked Limitation of physical activity (Class III) | 45 | 56.3 | ||||
χ2: Chi square; LR: Likelihood Ratio; SD: Standard Deviation; HHF: Hypertensive Heart Failure; *p value statistically significant
Key: Wt: Weight; Ht: Height; BMI: Body Mass Index; SBP: Systolic Blood Pressure; DBP: Diastolic Blood Pressure; TC: Total Cholesterol; FBG: Fasting Blood Glucose; HDL: High Density Lipoprotein; LDL: Low Density Lipoprotein; TG: Triglyceride; T test.
Table 1: Demographic characteristics of the study participants.
Echocardiographic parameters of study subjects
Table 2 shows the echocardiographic parameters in study subjects. All echocardiographic variables were significantly different between subjects and controls. The median LV Ejection Fraction (LVEF) was significantly lower in subjects with HF than controls, while LV End Diastolic Diameter (LVEDD) and left atrial diameter were significantly higher in HF subjects than controls [16-18]. TAPSE was significantly lower in HF subjects than in controls while RV MPI and mPAP were significantly higher in HF subjects than in controls.
RV systolic dysfunction was prominent in HHF subjects at 52.5% and 27.5% as measured by TAPSE and RVMPI respectively [19,20]. Similarly, elevated mean pulmonary arterial pressure was observed in about 47.5% of HHF subjects. About 53% percent of HHF subjects in this study were in reduced LVEF (LVEF <40%) (Table 3).
| Parameter | Case (n=80) median (IQR) | Control (n=80) median (IQR) | P value |
|---|---|---|---|
| LAD | 4.4 (4.2-4.5) | 3.3 (3.0-3.9) | <0.001* |
| LVPWD | 1.3 ± 0.1 | 1.0 ± 0.2 | <0.001* |
| LVEF | 38.5 (33.0-56.0) | 58.0 (56.0-62.0) | <0.001* |
| LVEDD | 5.8 (5.5-5.9) | 4.5 (4.2-4.8) | <0.001* |
| Mitral E/A Ratio | 0.88 (0.68-2.26) | 1.11 (0.79-1.37) | 0.232 |
| Mitral E/E’ | 15.2 (14.4-18.0) | 7.5 (6.8-8.7) | <0.001* |
| RVBD | 3.7 (2.8-4.1) | 3.0 (2.5-3.5) | <0.001* |
| TAPSE | 1.4 (1.2-1.8) | 1.9 (1.6-2.2) | <0.001* |
| RV MPI | 0.51 ± 0.1 | 0.46 ± 0.01 | <0.001* |
| mPAP | 24.7 (22.0-48.1) | 15.6 (9.4-21.4) | <0.001* |
| Tricuspid Ratio E/A | 1.09 ± 0.3 | 1.14 ± 0.3 | 0.299* |
| LVMI | 163.2 (142.5-181.8) | 76.4 (66.0-89.2) | <0.001* |
Key: LAD: Left Atrial Dimension; LVPWD: Left Ventricular Posterior Wall Thickness in Diastole; LVEF: Left Ventricular Ejection Fraction; LVEDD: Left Ventricular End Diastolic Dimension; RVBD: Right Ventricular Basal Dimension; TAPSE: Tricuspid Annular Plane Systolic Excursion; RV MPI: Right Ventricular Myocardial Performance Index; mPAP: Mean Pulmonary Arterial Pressure; LVMI: Left Ventricular Mass Index; ± mean ± standard deviation; T test; Mann-Whitney U test for Median (IQR); *p value statistically significant
Table 2: Distribution of echocardiographic variables in study participants.
| Parameter | Cases (n=80) | Control (n=80) | Statistical indices | ||
|---|---|---|---|---|---|
| N | % | N | % | ||
| TAPSE | 42 | 52.5 | 2 | 2.5 | **χ2 P<0.001* |
| RVMPI | 22 | 27.5 | 0 | 0 | **χ2 P<0.001* |
| mPAP | 38 | 47.5 | 1 | 1.3 | **χ2 P<0.001* |
TAPSE: Tricuspid Annular Plane Systolic Excursion; RVMPI: Right Ventricular Myocardial Performance Index; mPAP: Mean Pulmonary Arterial Pressure; *p value statistically significant.
Table 3: Comparison of right ventricular functional and structural abnormalities in study participants.
RV systolic dysfunction in HF subjects
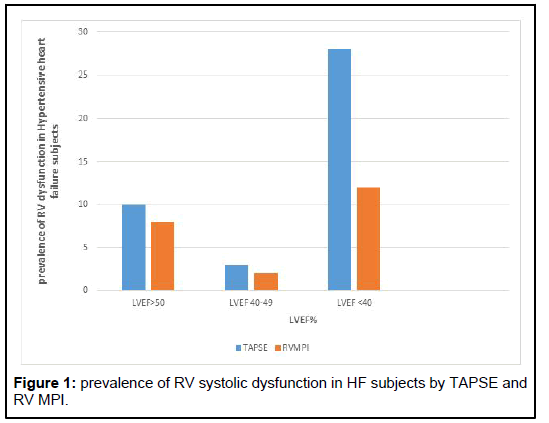
Figure 1 shows the prevalence of RV systolic dysfunction in HF subjects by TAPSE and RV MPI. Prevalence of RV systolic dysfunction in HF subjects with preserved EF (LVEF >50%) was 35.7% by TAPSE and 28.6% by RV MPI. The prevalence of RV systolic dysfunction was highest in HF subjects with LVEF <40% (66.7% by TAPSE and 28.6% by RV MPI) and subjects with LVEF between 40-49% (30.0% by TAPSE and 20.0% by RV MPI)(Table 4).
| Parameter | LVEF ≥ 50 n=28 (100%) | LVEF 40-49 n=10 (100%) | LVEF<40 n=42 (100%) | Statistical indices |
|---|---|---|---|---|
| TAPSE | 10 (35.7) | 3 (30.0) | 28 (66.7) | **χ2 P=0.014* |
| RVMPI | 8 (28.6) | 2 (20.0) | 12 (28.6) | **χ2 P=0.848 |
| Elevated mPAP | 14 (50.0) | 4 (40.0) | 20 (47.6) | **χ2 P=0.848 |
Key: RVBD: Right Ventricular Basal Diameter; TAPSE: Tricuspid Annular Plane Systolic Excursion; RVMPI: Right Ventricular Myocardial Performance Index; AT: Acceleration Time of pulsed doppler interrogation of right ventricular outflow tract; **χ2: Fisher’s exact; *P value is statistically significant.
Table 4: Association between right ventricular functional abnormalities, mean pulmonary arterial pressure in HHF subjects and left ventricular ejection fraction.
Correlation of RV echocardiographic variables with clinical and other echocardiographic variables in HF subjects.
Bivariate correlation analysis showed that TAPSE correlated positively and significantly with LVEF (r=0.419, p<0.001) while RV MPI showed a significant negative correlation with LVEF (r=−0.270, p<0.001). TAPSE also significantly correlated negatively with LVEDD (p=0.014) and LAD (p<0.001) while RV MPI had a significant positive correlation with LVEDD (r=0.290, p=0.009) as shown in Table 5.
| Variables | Correlation coefficient | TAPSE | P value | Correlation coefficient | RVMPI | P value |
|---|---|---|---|---|---|---|
| LVEF | Correlation coefficient | 0.419** | < 0.001 | Correlation coefficient | -0.270 * | 0.015 |
| LVEDD | Correlation coefficient | -0.275* | 0.014 | Correlation coefficient | 0.290** | 0.009 |
| LAD | Correlation coefficient | -0.381** | <0.001 | Correlation coefficient | -0.036 | 0.754 |
| mPAP | Correlation coefficient | -0.05 | 0.66 | Correlation coefficient | 0.156 | 0.168 |
| RVMPI | Correlation coefficient | -0.051 | 0.65 | Correlation coefficient | 1 | NC |
| Mitral E/E’ | Correlation coefficient | -0.243* | 0.03 | Correlation coefficient | -0.156 | 0.168 |
| Mitral E/A ratio | Correlation coefficient | -0.101 | 0.373 | Correlation coefficient | -0.055 | 0.625 |
| Tricuspid E/A ratio | Correlation coefficient | 0.141 | 0.213 | Correlation coefficient | -0.086 | 0.45 |
| TAPSE | Correlation coefficient | 1 | NC | Correlation coefficient | -0.05 | 0.66 |
| RVBD | Correlation coefficient | -0.105 | 0.352 | Correlation coefficient | 0.103 | 0.364 |
| LVMI | Correlation coefficient | 0.231* | 0.039 | Correlation coefficient | 0.034 | 0.764 |
| AT | Correlation coefficient | 0.05 | 0.66 | Correlation coefficient | -0.228 | 0.042 |
NC: Not Computed; ** Correlation is significant at the 0.01 level (2-tailed); * Correlation is significant at the 0.05 level (2-tailed)
Table 5: Correlation between selected echocardiographic parameters with TAPSE and RVMPI in HHF subjects.
Predictors of RV systolic dysfunction in hypertensive heart failure subjects
On binary logistic regression on predictors of RV dysfunction, LVEF was the only determinants among co-founders. Similarly, LVEF was sole predictor of TAPSE on multiple regression analysis (Tables 6 and 7).
| Characteristics | Odds ratio | Lower | Upper | P value |
|---|---|---|---|---|
| LAD | 2.078 | 0.252 | 17.116 | 0.497 |
| LVEF | 1.053 | 1.001 | 1.107 | 0.045* |
| LVEDD | 1.99 | 0.588 | 6.729 | 0.268 |
P-value: 0.005; LAD: Left Atrial Dimension; LVEF: Left Ventricular Ejection Fraction; LVEDD: Left Ventricular End Diastolic Dimension; *p value statistically significant
Table 6: Binary logistic regression analysis of the association between TAPSE and measured echocardiographic parameters in HHF subjects.
| Characteristics | Unstandardized coefficients | Lower | Upper | P value |
|---|---|---|---|---|
| LAD | 0.164 | -0.264 | 0.552 | 0.484 |
| LVEF | 0.017 | 0.008 | 0.026 | 0.001* |
| LVEDD | 0.079 | -0.143 | 0.301 | 0.48 |
p<0.001; LAD: Left Atrial Dimension; LVEF: Left Ventricular Ejection Fraction; LVEDD: Left Ventricular End Diastolic Dimension; *P value is statistically significant
Table 7: Multiple regression analysis of the association between TAPSE and echocardiographic parameters.
Discussion
In this study, about 53% of our subjects with hypertensive heart failure have impaired RV systolic function. Also, about 48% of subjects with heart failure secondary to hypertensive heart disease in this study had elevated mean pulmonary artery pressure which however, had no significant correlation with LV ejection fraction and RV systolic dysfunction in the study population. The LV ejection fraction, LV end diastolic dimension and LAD are associated with parameters of RV systolic dysfunction while LV ejection fraction is the only independent determinants of RV systolic dysfunction in this group of subjects with hypertensive heart failure.
The finding of high prevalence of RVSD in HHF subjects seen in this study support findings from other studies that reported varying prevalence of RV systolic dysfunction in subject with heart failure between 35 and 65%.
This study found RV dysfunction using TAPSE and RVMPI in 52.5% and 27.5% respectively. Oketona, et al. studied RV systolic dysfunction in hypertensive heart failure subjects using TAPSE and RV MPI and found RV dysfunction in 53% and 56% respectively. The prevalence of TAPSE were comparable in both studies, however, the high prevalence of abnormal RVMPI reported in their study may be due to the fact that majority (84%) of subjects with heart failure in their study had reduced ejection, this study reported subjects in reduced ejection fraction in about 52% of heart failure subjects. RV dysfunction has been reported to be more prevalent in subjects with HFrEF.
A higher prevalence of RV dysfunction of 70% were also reported by the study by Meluzin, et al., using “pulsed doppler tissue imaging of the velocity of tricuspid annular systolic motion among heart failure patients in Europe” although majority of the patients in their study were candidates for heart transplantation which means they were in end-stage heart failure, thus likely to also have more RV systolic dysfunction than this present study.
TAPSE is an easily reproducible measure of RV function and has been found to correlate with the radionuclide angiographic estimate of RV global systolic function. However, TAPSE assumes that the longitudinal displacement of a single segment represents the function of a threedimensional RV structure which is angle and load dependent.
Thus, these limitations to the use of TAPSE for assessing RV function alone necessitates the validation of other methods to serve as alternatives or further validate results obtained using one method. RVMPI was shown by Karnati to correlate with radionuclide derived RV EF.
Tei found that RV MPI was a strong predictor of clinical status and survival in subjects with pulmonary hypertension. The LV Tei index has been well studied in subjects with HF. However, there is a scarcity of data on the clinical value of RV MPI. Thus, our study decided to also assess RV function in subjects with HHF using RVMPI.
Our study found significant relationship between indices of RV systolic function and LV Ejection fraction.
Result from this study showed that subject in HFrEF (66.7%) had significant RVSD as measured by TAPSE compared to those in HFpEF (35.7%) and HFmrEF (30%) respectively. This finding corroborates findings from other studies that had documented RVSD to be more prevalent in patient with HFrEF than those in HFpEF.
Puwanant, et al., in their study on “right ventricular systolic function in patients with preserved and reduced ejection fraction heart failure” found RVSD measured by TAPSE in 40% of HFpEF and 76% in HFrEF. The higher prevalence reported in their study can be explained from the different causes of HF in their study, greater than 50% of participants had coronary heart disease, 37% diabetics and 32.5% cardiomyopathy.
Coronary artery disease causes regional wall motion abnormalities which may affect indices of RV systolic functions like TAPSE. In addition, the RV may also be affected by the myopathic process in patients with cardiomyopathy.
This study also found a high prevalence of impaired RV function in HHF with mildly reduced Ejection Fraction (HFmrEF) at 30%. There is a dearth of studies assessing this relationship in African subjects with HFmrEF on echocardiography to compare with.
Impaired RV systolic function has been shown to be major adverse factor in prognosis of heart failure patients. Therefore, there is need for increased emphasis on evaluation of right heart in hypertensive heart failure patients and more efforts at investigation of therapies directed at the right heart.
This study found no relationship between the indices of RV systolic function and mean pulmonary arterial pressure.
There is conflicting data on the pulmonary vasculature haemodynamics in hypertensive subjects.
Karaye, et al., in their study on “prevalence, prognosis and outcome of pulmonary hypertension in heart failure subjects” reported no significant correlation between mPAP and RV fractional shortening (another measure of RV systolic function) (r=-0.140; p=0.248).
Similarly, Adewoye, et al., in their study on right ventricular systolic function in HHF subjects found no relationship between PH and indices of RV systolic function (TAPSE: r=-0.034; p=0.7690; S’: r=0.074; p=0.5282; RVFAC: r=-0.083; p=0.64941 respectively).
Furthermore, Kjaergaard, et al., in their study on predictors of right ventricular function in heart failure using TAPSE reported no association between pulmonary hypertension and TAPSE. However, these findings differ from what was reported in other studies.
Karaye, et al., in another study on “right ventricular dysfunction in a hypertensive population stratified by patterns of left ventricular geometry” observed that PASP was a correlate of TAPSE. However, S’ (another parameter to assess RV systolic function) had no relationship with PASP. This finding was however on hypertensive patient without any evidence of heart failure.
Ghio, et al., found an inverse relationship between PAP and RV ejection fraction. However, it was reported in their study that some patients had preserved RV function despite elevated PAP. They also observed that the inverse relationship between PAP and RV dysfunction was more common in patients with RV dysfunction arising from RV afterload mismatch seen in dilated and ischemic cardiomyopathy.
This may explain why this present study did not observe any statistical significant relationship between PAP and RV systolic function measured using RVMPI and TAPSE as the mechanism of right ventricular dysfunction in hypertension result more from ventricular interdependence than changes in pulmonary vasculature.
Another possible reason for the failure of this study to demonstrate significant relationship between mPAP and RV systolic functions may be attributed to use of diuretic therapy among our HHF patients. Diuretics have been documented to reduce pulmonary arterial pressure.
On binary logistic regression analysis for predictors of RV dysfunction, factors that were associated with abnormal RV dysfunction included LVEF, LVEDD and LAD while on multiple regression analysis; only LVEF was the sole determinants of TAPSE.
Our finding corroborates what was reported by Ojji, et al., in Nigeria who also found LVEF as only predictor of RV dysfunction using TAPSE. This is similar to previous studies in Caucasians by de Groote P, et al., in their study on “right ventricular ejection fraction is an independent predictor of survival in patients with moderate heart failure”.
Similarly, Kjaergaard, et al., in their study titled “right ventricular dysfunction as an independent predictor of short and long term mortality in patients with heart failure” reported LVEF as sole determinants of TAPSE. However; this differs from what was reported by Adewoye, et al., in south-western Nigeria where LVEF had no independent relationship with RV systolic dysfunction. They further reported that their use of composite values for TAPSE, RVFAC and S’ could have attributed to the lack of relationship between LVEF and right ventricular systolic function seen in their study.
Conclusion
RV systolic dysfunction is common in subjects with hypertensive HF and was found in >50% of such subjects using TAPSE and RV MPI and in 48% with RV S′. All three echocardiographic parameters of RV systolic function correlated with LVEF and FS.
References
- Adebayo SO, Olunuga TO, Durodola A, et al. Heart failure: Definition, classification, and pathophysiology-A mini review. Niger J Cardiol. 2017;14(1):9-14.
- Ntusi N, Mayosi BM. Epidemiology of heart failure in sub-Saharan Africa. Expert Rev Cardiovasc Ther. 2009;7(2):169-80.
[Crossref] [Google Scholar] [PubMed]
- Adewoye AI, Adeoye MA, Adesoji AA, et al. Right ventricular systolic function in Nigerians with heart failure secondary to hypertensive heart disease Ibadan. Afri Heal Sci. 2019;19(2):2130-9.
[Crossref] [Google Scholar] [PubMed]
- Michael EF, Scott DS, Eldrin FL, et al. Right ventricular dysfunction and adverse outcome in patients with advanced heart failure. J Card Fail. 2006;12(8):616-20.
[Crossref] [Google Scholar] [PubMed]
- Vasiliki VG, Andreas PK, Barry AB, et al. Left ventricular dysfunction with pulmonary hypertension circulation heart failure. Circ Hear Fail. 2013;6(2):344-54.
[Crossref] [Google Scholar] [PubMed]
- Karaye KM, Saidu H, Mohammed SB, et al. Prevalence, clinical characteristics and outcome of pulmonary hypertension among admitted heart failure patients. Ann Afr Med. 2013;12(4):197-204.
[Crossref] [Google Scholar] [PubMed]
- Ghio S, Gavazzi A, Campana C, et al. Independent and additive prognostic value of right ventricular systolic function and pulmonary artery pressure in patients with chronic heart failure. J Am Coll Cardiol. 2001;37(1):183-88.
[Crossref] [Google Scholar] [PubMed]
- Karaye KM, Saidu H, Shehu MN. Right ventricular dysfunction in a hypertensive population stratified by patterns of left ventricular geometry. Cardiovasc J Afr. 2012;23(9):478-82.
[Crossref] [Google Scholar] [PubMed]
- Kjaergaard J, Iversen KK, Akkan D, et al. Predictors of right ventricular function as measured by tricuspid annular plane systolic excursion in heart failure. Cardiovasc Ultrasound. 2009;7(51):1-7.
[Crossref] [Google Scholar] [PubMed]
- Fiorentini C, Barbier P, Galli C, et al. Pulmonary vascular over reactivity in systemic hypertension. Hypertension. 1985;7(6):995-1002.
[Crossref] [Google Scholar] [PubMed]
- Robert F, Paul L, Jan S, et al. The pulmonary circulation in essential systemic hypertension. Am J Cardiol. 1988;61(13):1061-5.
[Crossref] [Google Scholar] [PubMed]
- Arthur CO, Godspower EA. Pattern of heart failure in a Nigerian teaching hospital. Vasc Health Risk Manag. 2009;5:745-50.
[Crossref] [Google Scholar] [PubMed]
- Ojji D, Stewart S, Ajayi S, et al. A predominance of hypertensive heart failure in the Abuja heart study cohort of urban Nigerians: A prospective clinical registry of 1515 de novo cases. Eur J Heart Fail. 2013;15(8):835-42.
[Crossref] [Google Scholar] [PubMed]
- Rudski LG, Lai WW, Afilalo J, et al. Guidelines for the echocardiographic assessment of the right heart in adults: A report from the American society of echocardiography endorsed by the European association of echocardiography, a registered branch of the European society of cardiology, and the Canadian society of echocardiography. J Am Soc Echocardiogr. 2010;23:685-713.
[Crossref] [Google Scholar] [PubMed]
- Lancellotti P, Budts W, de Wolf D, et al. Practical recommendations on the use of echocardiography to assess pulmonary arterial hypertension-A Belgian expert consensus endorsed by the working group on non-invasive cardiac imaging. Acta Cardiol. 2013;68(1):59-69.
[Crossref] [Google Scholar] [PubMed]
- Fisher MR, Forfia PR, Chamera E, et al. Accuracy of doppler echocardiography in the hemodynamic assessment of pulmonary hypertension. Am J Respir Crit Care Med. 2009;179(7):615-21.
[Crossref] [Google Scholar] [PubMed]
- Milan A, Magnino C, Veglio F. Echocardiographic indexes for the non-invasive evaluation of pulmonary hemodynamics. J Am Soc Echocardiogr. 2010;23(3):225-39.
[Crossref] [Google Scholar] [PubMed]
- William V, El Kilany W. Assessment of right ventricular function by echocardiography in patients with chronic heart failure. Egypt Hear J. 2018;70(3):173-9. [ Crossref]
[Google Scholar] [PubMed]
- Gulati A, Ismail TF, Jabbour A, et al. The prevalence and prognostic significance of right ventricular systolic dysfunction in non-ischemic dilated cardiomyopathy. Circulation. 2013; 128:1623-33.
[Crossref] [Google Scholar] [PubMed]
- Meluzin J, Spinarova L, Bakala J, et al. Pulsed Doppler tissue imaging of the velocity of tricuspid annular systolic motion. Eur Heart J. 2001;22(4):340-8.
[Crossref] [Google Scholar] [PubMed]