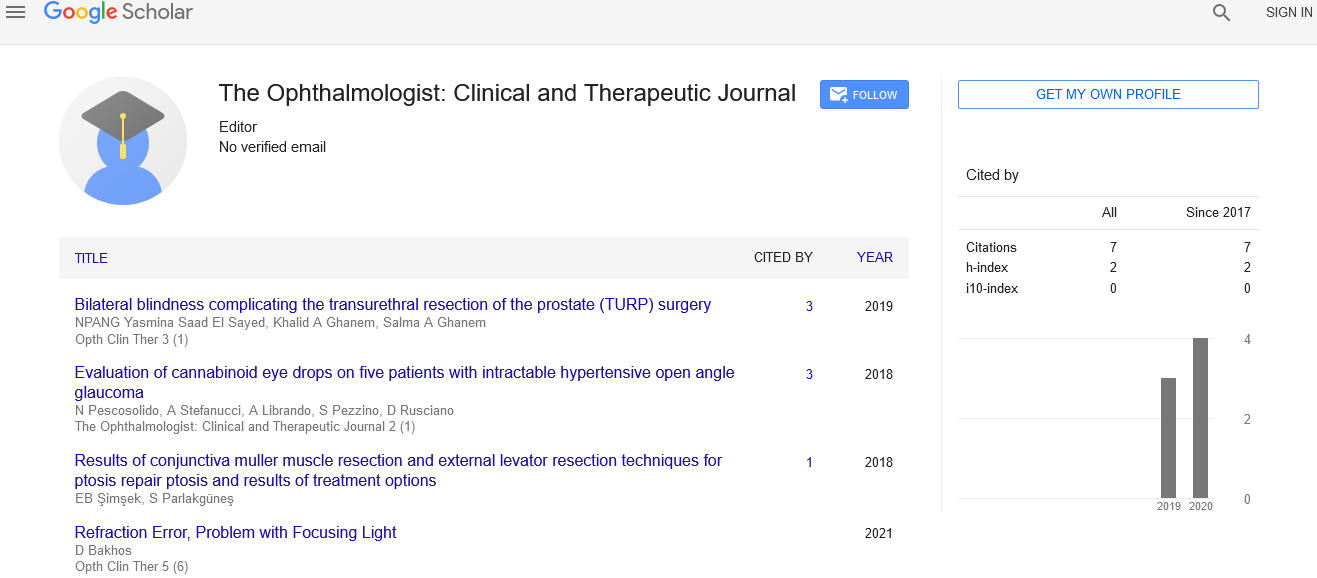
Results of conjunctiva muller muscle resection and external levator resection techniques for ptosis repair ptosis and results of treatment options
2 Department of Ophthalmology Yeditepe University Medical School, Istanbul, Turkey, Email: ilke.simsek@dogalzeka.com.tr
Received: 28-May-2018 Accepted Date: May 09, 2018; Published: 16-Jun-2018
Citation: Citation: Simsek BI and Parlakgünes Z,et al. Results of conjunctiva muller muscle resection and external levator resection techniques for ptosis repair ptosis and results of treatment options. Opth Clin Ther. 2018;2(1):8-12.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Objective: To evaluate the results of levator aponeurosis surgery (LS) and conjunctiva- Müller muscle resection (CMR) operations for correction of upper eyelid ptosis. Materials and Methods: This is a prospective study of 85 patients who had undergone either LS or CMR for ptosis from January 2015 to May 2016. Detailed information including age, gender, etiology, type of surgery, laterality of surgery, preoperative levator function, pre- and postoperative palpebral fissure height (PFH), postoperative PFH change, postoperative day 1 pain, edema, ecchymosis, cosmetic outcome, reoperation rate and operating time from initial maneuver to wound closure were recorded. Patients with good levator function (over 12 mm) were included to the study. Postoperative measurements at the 6th month visit were used for analysis. Results: Of the surgical procedures 67% (57/85) were LS, 33% (28/85) were CMR operation. For the patients who underwent LS, preoperative PFH was statistically lower than CMR patients (p=0.016). Postoperative PFH and PFH change between two operation groups were not statistically significant (p=0.1 for postop PFH, p=0.073 PFH change). Postoperative PFH change in both groups was statistically significant (p=0.001 for both evaluations). There were no significant differences between the 2 groups regarding postoperative 1st day pain, edema, ecchymosis (p=0.128), reoperation rate, and final cosmetic outcome (p=0.724). In LS group, the operation time (28.86±5.09 mins) was statistically significantly higher than CMR group (17.71±3.11 mins) (p=0.001). Conclusion: Although the CMR provides a shorter operation time both the LS and CMR lead to good surgical results with equivalent final cosmetic satisfaction, reoperation rates and postoperative 1st day pain, edema, ecchymosis. Key Words: conjunctiva-Müller muscle resection; levator aponeurosis surgery; ptosis; ptosis surgery.
Keywords
Conjunctiva-Müller Muscle Resection; Levator aponeurosis surgery; Ptosis; Ptosis Surgery
Introduction
Ptosis is a condition of drooping upper eyelid. The descended upper eyelid results in partial or complete obscuration of the superior visual field. Ptosis repair is one of the most common and challenging procedures in oculoplastic practice. The appropriate surgical technique is determined according to the levator function, severity of ptosis and result of the phenylephrine test. [1-10] Surgical repair can be done by both posterior or anterior surgical approaches in patients with good levator function. During anterior approach through an eyelid crease incision, the levator aponeurosis, with or without shortening, is usually reattached to the anterior tarsal plate [5-11].
Posterior approach by transconjunctival resection of Müller’s muscle and conjunctiva has been used to correct mild to moderate ptosis; its widespread use is need of a positive response to the phenylephrine test [11-15].
In the literature and oculoplastic practice, the appropriate surgical decision is still controversial. There are limited number of studies evaluating this issue. These studies declare, based on the severity of ptosis and the levator function measurements surgeon can use different techniques.[2,5,6,7,16] So, our study aims to prospectively examine the patients who have had either a levator aponeurosis surgery (LS) or a CMR surgery for ptosis. We evaluated their functional and cosmetic outcome following these surgeries.
Material and Methods
The patient population was selected from an ophthalmology clinic oculoplastic department prospectively. All consecutive patients who underwent ptosis repair either LS or CMR operation by one oculoplastic surgeon (IBS) during the year January 2015 - May 2016 were included.
Information included age, gender, type of surgery, preoperative and postoperative palpebral fissure height (PFH), PFH change, preoperative levator function, etiology, laterality of surgery, postoperative day 1 pain, edema and ecchymosis, cosmetic outcome, reoperation rate and operating time from initial maneuver to wound closure. Patients were examined on the 1st day, 1st week and 1st, 3rd and 6th months postoperatively. Postoperative measurements at the 6th month visit were used for analysis.
Patients were excluded if they had levator function under 12 mm, undergone prior ptosis surgery, concomitant eyelid or brow surgery, cases with neurogenic and mechanical ptosis. The study was conducted in compliance with the principles of the Declaration of Helsinki and complies with the policies of the local institutional review board.
Cosmetic outcome was graded on the basis of final eyelid position, symmetry and eyelid crease, on a scale of good, moderate and poor. Operating doctor checked the results and were considered good when final inter eyelid height asymmetry ≤1 mm, with good eyelid contour and crease. If there is a problem with one of these parameters, cosmetic score was moderate. If outcome was not satisfactory and need reoperation, cosmetic outcome was poor.
Before the operation, all patients underwent phenylephrine test. Elevation of the eyelid to the desired level after instillation of one drop of topical 5% phenylephrine hydrochloride (Mydfrin 5% ophthalmic solution, AlconR) within 10 to 15 minutes of instillation is considered a positive response, indicating that CMR can be successfully executed. The operations were done under local anesthesia unless the patients’ age were under 18 years.
Surgical Technique
Two curved hemostats were placed at the superior tarsal border after the desired level of tissue is engaged 6-0 PROLENE® Polypropylene suture was passed back and forth proximal to the hemostats in a horizontal mattress fashion. The tissue in the hemostats were excised and 6-0 PROLENE® Polypropylene suture was used to close the wound. The ends of the sutures, medial and lateral, were directed through the wound edges on the conjunctiva side out through the lid crease. Each end of the suture was tied on itself to the skin. 4 mm of conjunctiva- Müller resection was performed for each 1 mm of desired elevation.
The patients with giving no response to the phenylephrine test was performed external LS. A central upper eyelid skin crease incision was marked at the natural crease 8-10 mm from the ciliary margin. After incising the orbicularis muscle and opening the orbital septum, the preaponeurotic fat pad was retracted to observe the levator aponeurosis. The levator aponeurosis was released and sutured to the tarsus with three 6-0 vicryl® (polyglactin) sutures. First the central suture was adjusted until the height and contour were optimal, and the nasal and temporal ones are placed afterwards. At last the skin was closed with 6-0 vicryl® (polyglactin) suture. For the levator resection, especially for the local anesthesia patients the eyelid level was adjusted when the patient is at the sitting position. For the general anesthesia patients, resection was done according to the level of ptosis.
For the statistical evaluation of the data, NCSS (Number Cruncher Statistical System) 2007 (Kaysville, Utah, USA) software was used. Measurable data of our study were presented as mean± SD. The range of the variable data was measured using a Mann Whitney U test. When comparing the two groups, quantitative data were analyzed with independent samples using a Mann Whitney-U test. Intergroup quantitative data were analyzed using a Wilcoxon Signed Ranks test. Qualitative data were analyzed using a Pearson chi-square test, Fisher’s exact test, Yates’ continuity correction test and Fisher Freeman Halton test. A value of p < 0.01 and p <0.05 was taken to be statistically significant.
Results
Of the 85 patients selected for the study, 40 (47.1 %) were female, 45 (52.9 %) were male, with an average age of 48.52 ± 21.90 (8-80) years. There were no statistically significant differences considering age (p= 0.215) and gender (p=0.283) between 2 groups. Of the surgical procedures, 67% (57/85) were LS, 33% (28/85) were CMR operation. Patient demographics are summarized in (Table 1).
| Total | LR (n=57) | CMR (n=28) | p | ||
|---|---|---|---|---|---|
| Age (Year) | Mean±Sd | 48.52±21.90 | 45.77±22.18 | 54.11±20.57 | a0.215 |
| Min-Max.(average) | 8 – 80 (54) | 8-79 (35) | 20-80 (62) | ||
| n (%) | n (%) | n (%) | |||
| Gender | Female | 40 (47.1) | 24 (42.1) | 16 (57.1) | b0.283 |
| Male | 45 (52.9) | 33 (57.9) | 12 (42.9) | ||
| aMann Whitney U Test bYates Continuity Correction Test | |||||
Table 1: Patient demographics related to operation technique. (LS: levator levator aponeurosis surgery CMR: Conjunctiva- Müller Muscle Resection)
Patients who underwent LS had more ptotic eyelids preoperatively (mean preoperative PFH was 6.19±1.41 for LS group and 6.75±1.14 for CMR group). Postoperative PFH (8.58±1.31 for LS vs 8.79±0.92 for CMR) and PFH change (2.39±0.73 for LS vs 2.04±0.79 for CMR) between two operation groups were not statistically significant (p=0.127 for PFH and p=0.073 for PFH change). In both groups, mean postoperative PFH change was 2.42±0.73 mm in LS group, 2.04±0.79 mm in CMR group. PFH change in both groups was statistically significant compared with the preoperative PFH values (p=0.001 for both group) (Table 2).
| Total | LR (n=57) | CMR (n=28) | p | ||
|---|---|---|---|---|---|
| Preop PF (mm) | Mean±Sd | 6.38±1.3 | 6.19±1.4 | 6.75±1.1 | a0.016* |
| Min-Max (Median) | 3-9 (6) | 3-9 (6) | 4-9 (7) | ||
| Postop PF (mm) | Mean±Sd | 8.65±1.1 | 8.58±1.3 | 8.79±0.9 | a0,127 |
| Min-Max (Median) | 7-12 (8) | 7-12 (8) | 7-10 (9) | ||
| PF Change (mm) | Mean ±Sd | 2.27±0.7 | 2.39±0.7 | 2.04±0.7 | a0.073 |
| Min-Max (Median) | 1-4 (2) | 1-4 (2) | 1-3 (2) | ||
| p | c0.001** | c0.001** | |||
| aMann Whitney U Test, cWilcoxon Signed Ranks Test , *p<0.05, **p<0.01 | |||||
Table 2: Preoperative palpebral fissure height (PF) and change in PF for patients operated on levator aponeurosis surgery (LS) or Conjunctiva-Müller Muscle Resection (CMR).
For both group levator palpebrae muscle function ranged from 12 to 18 mm (mean 16 mm). In both operation groups, there was no significant difference between the etiology and laterality. day 1, compared with 7.1% of the patients in the CMR group. But the difference was statistically insignificant (p=0.125). In LS group, 11 patients (19.2%) presented with surgical failure, including 8 under-corrections, 3 over-corrections. Of them, 6 patients (10.5%) had undergone reoperation; 5 patients for under correction, 1 patient for overcorrection. In CMR group 1 (3.5%) patient presented with under correction. None of the patients for this group had a reoperation. But in both groups, reoperation rates (p=0.171;p>0.05) were statistically in significant. (Figure 1).
Patients who underwent LS; good cosmetic outcome was 73%, for the CMR group good cosmetic outcome was 78%. Additionally, lower percentage of the CMR patients attained a poor outcome (0%) as compared with LS patients (5.3%). But in both groups, there was no significant difference for the final cosmetic outcome (p=0.724, p>0.05) (Table 3).
| Total | LR (n=57) | CMR (n=28) | p | ||
|---|---|---|---|---|---|
| Laterality | Right Left |
30 (35.3) 55 (64.7) |
24 (42.1) 33 (57.9) |
6 (21.4) 22 (78.6) |
b0.102 |
| Etiology | Congenital Senil Traumatic |
43 (50.6) 41 (48.2) 1 (1.2) |
33 (57.9) 23 (40.4) 1 (1.8) |
10 (35.7) 18 (64.3) 0 (0.0) |
f0.078 |
| Postoperative day 1 pain, edema, ecchymosis | None | 70 (82.4) | 44 (77,2) | 26 (92.9) | d0.128 |
| Exist | 15 (17.6) | 13 (22.8) | 2 (7.1) | ||
| Reoperation | None Exist |
75 (88.2) 10 (11.8) |
51 (89.5) 6 (10.5) |
28 (100.0) 0 (0.0) |
d0.027* |
Table 3: Outcome of 85 patients who underwent levator aponeurosis surgery (LS) or Conjunctiva-Müller Muscle Resection (CMR) for laterality, etiology, reoperation, cosmetic outcome, operating time from skin incision to wound closure, postoperative day 1 pain, edema, ecchymosis.
When evaluating the operating time for each procedure, the mean time from the beginning of the procedure to wound closure was 28.86±5.09 minutes in levator resection group, 17.71±3.11 minutes in CMR group. In levator resection group the operation time was statistically significantly higher than CMR group (p=0.001; p<0.01) (Figure 2, Table 3).
Discussion
Simon et al10 compared standard LS with CMR retrospectively for 272 upper eyelid ptosis patients, 141 undergoing concurrent blepharoplasty. Patients who had LS compared to CMR group had lower MRD1 preoperatively (MRD1: 0.33±1.5 mm for LR vs 1.0±0.9 mm for CMR; p<0.001) but attained a similar MRD1 postoperatively (2.3±1.6 mm for LR vs 2.4 ±1.0 mm for CMR p=0.6). Also, postoperative MRD1 change (1.9 ±1.7 mm vs 1.4±1.3 mm; p=0.02) was significantly higher for the LS group. These results similar with our study are, such that; in both papers, the patients selected for LS were the ones with more severe ptosis in terms of lower MRD1 to start with. However, 20% the reoperation rates are different from our study with 11.8%.
LS is an effective and more complex procedure, requiring a detailed knowledge of eyelid anatomy to establish good eyelid contour and position. However, the surgery involves dissection of the layers of the eyelid, is time consuming, and requires patient participation. On the other hand, there are several advantages of this procedure: it is effective for severe ptosis, it can be done for the phenylephrine-negative patients, and it can be adjustable during surgery. [2,5-11,16] The outcome of LS has varied in previous reports with reported success rates of 70% to 95% with the reoperation rates 8.7% to 12%. In our study, the reoperation rate for LS was 10.5% [2,7,16-22].
McCulley 17 et al studied 828 patients who had LS for ptosis, their reoperation rates were 8.7% overall, 5.2% of unilateral, and 13% of bilateral cases. 80% of the patients attained satisfactory results, defined as postoperative MRD1 was between 2.0- 4.5 mm with less than 1 mm of asymmetry between two eyelids. Additionally, they reported that patients with bilateral or severe ptosis have increased risk of under correction. Simon et al 10 reported that 18% of their LS patients and 3% of CMR patients had reoperation. Our reoperation rates were 10.5% for the levator resection group, 0% for CMR group, but in both groups reoperation rates (p=0.171; p>0.05) were statistically insignificant. These results show that CMR group had a lower reoperation rate but we must keep in mind that the patients selected for the LS procedure were the severe ptosis patients with lower MRD1.
CMR surgery is quick, easier than LS, requires no skin incision, yields generally expected results, and requires no patient cooperation. But you cut out a part of Müller’s muscle does not allow intraoperative adjustment of lid height, and presumably carries a risk of dry eye. In the literature, excellent results have been reported with CMR for ptosis. [7,8,10,11,16,23-29] Simon et al10 reported that higher percentage of CMR patients attained excellent and good results (51% and 33% respectively) as compared with external LS patients (43% and 25%). In our study, although none of the CMR patients had poor outcome compared with the 5.3% in the LS group, this was statistically insignificant (p=0.724, p>0.05).
In several studies for the CMR procedure, show that excision of the tarsal conjunctiva may aggravate dry eye symptoms.28 Others found no significant effect on tear production measured by Schirmer testing, so there is no consensus about the progress of dry eye.26 There is a suggestion that excision of conjunctiva close to the tarsal border that barns several glands may cause dry eyes, however histopathological studies never confirmed this hypothesis.[26] In our study, we did not see any dry eye patient in our series.
In the literature, there is currently no consensus among oculoplastic surgeons relating to a gold standard preoperative assessment for ptosis. Cetinkaya et al5 describes ptosis algorithm with two parameters; levator function and MRD 1 measurements. For the patients with good levator function and 2 mm droop from normal position CMR is the viable option. With moderate ptosis levator surgery is usually preferred. Aakalu et al15 administered a national survey to assess the current practice patterns for management of ptosis by ASOPRS members. Nearly 100% of members performed some variant of LS for ptosis, 74% of respondents perform some type of internal levator aponeurosis advancement surgery (i.e. Fasanella Servat, Müller ‘s Muscle-conjunctival resection). Two-thirds of ASOPRS members utilized a phenylephrine test in their preoperative testing protocol. In particular, new graduates from fellowship are more prone to using internal levator advancement surgery types. Mota and Norris [30] assessed the current practice using phenylephrine test by BOPSS (British Oculoplastic Surgery Society) consultants for ptosis surgery. 76% perform levator advancement as first line surgery. Then, 40% routinely use phenylephrine test; if the test is positive majority uses posterior approach.
Limitation of our current study is, the study compares two dissimilar groups for ptosis surgery. The severity of the ptosis was different between the two groups. But our aim was not only compare but also to evaluate the results of two surgeries prospectively.
When ptosis is identified, and operation is planned, a decision on which surgical procedure to perform is important. There are several different techniques that a surgeon can use based on the severity of ptosis, the amount of levator function, and the phenylephrine test result. The amount of levator function is the major determinant of surgical approach. Which procedure is better is up for debate and it depends on the preference of the surgeon. LS and CMR operations are two standard ways to correct upper eyelid ptosis with good levator function. There are retrospective studies comparing both technique to evaluate the success of these surgeries. [1-15].
Conclusion
Postoperative cosmetic outcome, surgical failure and reoperation rates, postoperative pain, edema, ecchymosis for CMR group seems lower than LS group, but it was statistically insignificant. The operation time and preoperative PFH for CMR was statistically lower than LS. As a result, our study supports that LS and CMR operations are both give good results for ptosis. The best surgical method is the one that the experienced surgeon is most comfortable with.
REFERENCES
- Baroody M, Holds JB, Vick VL. Advances in the diagnosis and treatment of ptosis. Curr Opin Ophthalmol 2005; 16(6):351-5.
- Anderson RL.Predictable ptosis procedures: do not go to the dark side. Ophthal Plast Reconstr Surg 2012; 28(4): 239-41.
- Pang NK,Newsom RW,Oestreicher JH ,et al.Fasanella-Servat procedure:indications, efficacy, and complications. Can J Ophthalmol 2008; 43(1): 84–88.
- Anderson RL, Dixon RS. Aponeurotic ptosis surgery.Arch Ophthalmol 1979; 97(1): 1123–28.
- Cetinkaya A,Brannan PA.Ptosis repair options and algorithm. Curr Opin Ophthalmol.2008;19(5): 428-34.
- Zhang L,Pan Y,Ding J, et al. Surgical correction of myogenic ptosis using a modified levator resection technique.Can J Ophthalmol 2015;50(6):471-5.
- Finsterer J.Surgical correction of myogenic ptosis using a modified levator resection technique. Can J Ophthalmol 2015;50(6):471-5.
- Beard C. Ptosis surgery: past, present, and future. Ophthal Plast Reconstr Surg.1985; 1(1):69-72.
- Ünal M, Konuk O, Köksal M, Hasanreisoğlu B. Ptozisli olgunun değerlendirilmesinde ve cerrahinin seçiminde etyolojik sınıflamanın önemi. MN Oftalmoloji 1998; 5(1): 375-377.
- Ben Simon GJ, Lee S, Schwarcz RM, et al .External levator advancement vs Müller's muscle-conjunctival resection for correction of upper eyelid involutional ptosis. Am J Ophthalmol 2005;140(3):426-32.
- Sohrab MA, Lissner GS. Comparison of Fasanella-Servat and Small-Incision Techniques for Involutional Ptosis Repair. Ophthal Plast Reconstr Surg 2016;32(2):98-101.
- Samimi DB, Erb MH, Lane CJ, et al. The modified fasanella-servat procedure: description and quantified analysis. Ophthal Plast Reconstr Surg. 2013;29(1):30-4.
- Yazici B, Beden U.Use of 0,5 % apraclonidine solution in evaluation of blepharoptosis. Ophthal Plast Reconstr Surg 2008;24(4):299-301.
- Skibell BC, Harvey JH, Oestreicher JH, et all. Adrenergic receptors in the ptotic human eyelid: correlation with phenylephrine testing and surgical success in ptosis repair. Ophthal Plast Reconstr Surg 2007;23(5):367-71.
- Aakalu VK, Setabutr P.Current ptosis management: a national survey of ASOPRS members. Ophthal Plast Reconstr Surg 2011;27(4):270-6.
- Guy G Massry, Mark R Murphy, Babak Azizzadeh Master Techniques in Blepharoplasty and Periorbital Rejuvenation; Springer, 2011;125-126.
- McCulley T, Kersten RC, Kulwin DR, et al.Outcome and influencing factors of external levator palpebrae superioris aponeurosis advancement for blepharoptosis. Ophthal Plast Reconstr Surg 2003;19(5):388 –393.
- Shore JW, Bergin DJ, Garrett SN.Results of blepharoptosis surgery with early postoperative adjustment. Ophthalmology 1990;97(1):1502–11.
- Older JJ. Levator aponeurosis surgery for the correction of acquired ptosis: analysis of 113 procedures. Ophthalmology 1983; 90(1):1056–9.
- Kükner AŞ, Çelebi S, Aykan Ü, Demir T. Konjenital ptozisli olgularda levator aponevroz katlama sonuçlarımız. T Klin Oftalmoloji 2000; 9(1):171-174.
- Ünal M. Levator Cerrahisi. T Klin Oftalmoloji 1997;6(1):98-105.
- Özdal PÇ, Göka Ş, Teke MY,et al.Ptozis tedavisinde levator cerrahisi. T Klin Oftalmoloji 2001;10(1): 139-145.
- Mercandetti M, Putterman AM, Cohen ME, et al. Internal levator advancement by Müller’s muscle-conjunctival resection. Arch Facial Plast Surg 2001;3(2):104 –110.
- Weinstein G, Buerger GF Jr. Modifications of the Müller’s muscle-conjunctival resection operation for blepharoptosis. Am J Ophthalmol 1982;93(1):647– 651
- Lake S, Mohammad-Ali FH, Khooshabeh R. Open sky Müller’s muscle– conjunctiva resection for ptosis surgery. Eye 2003;17(9):1008 –12.
- Dailey RA, Saulny SM, Sullivan SA. Müller muscle-conjunctival resection:effect on tear production. Ophthal Plast Reconstr Surg 2002;18(2):421-5.
- Marcet MM, Setabutr P, Lemke BN,et al. Surgical microanatomy of the müller muscle-conjunctival resection ptosis procedure. Ophthal Plast Reconstr Surg 2010;26(5):360-4.
- Wee SW, Lee JK .Clinical outcomes of conjunctiva-Müller muscle resection: association with phenylephrine test-negative blepharoptosis and dry eye syndrome. Craniofac Surg.2014;25(3):898-901.
- Korkmaz NS , Eroğu O, Eroğul E Y. Demographic and Histopathologic Features of Eye Capsules T. Oft. Gaz. 2002;32(1):564-69.
- Mota PM, Norris JH.Review on surgical management of ptosis and the use of phenylephrine: A national survey of British Oculoplastic Surgery Society.Orbit. 2016;35(6):339-42.