Successful and Integrated Dental Management of Bilateral Ranula in Child: Two Different Approaches for One Case
2 Department of Pathology and Oral Diagnosis, School of Dentistry, Brazil, Email: dentist123@gmail.com
Received: 20-Sep-2017 Accepted Date: Oct 06, 2017; Published: 17-Oct-2017
Citation: Clarissa F, Lucianne CM, Maria EJ. Successful and Integrated Dental Management of Bilateral Ranula in Child: Two Different Approaches for One Case. J Dent and Oral Res 2017;1(1):1-2.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
This paper reports a case of a 10 year old female patient with a chief complaint of swelling in the floor of the mouth. During clinical examination, a large, floating, dome-shaped swelling was observed bilaterally. The probable clinical diagnosis was bilateral ranula. The treatment was performed through oral surgery, in which marsupialization of one injury and enucleation of the other was performed. Histopathological examination revealed extravasated mucin, surrounded by reactive granulation tissue containing foamy histiocytes. Despite the different types of treatment, both ranulas had good prognosis. During dental appointments, there was a significant improvement in oral hygiene. No recurrence was observed over an 18 month follow-up period. An accurate diagnosis and an appropriate treatment plan are fundamental for a successful treatment of ranulas in children. Regardless of the surgical technique, conservative maneuvers associated with careful clinical monitoring were indispensable for the longevity and success of treatment.
Keywords
Ranula, Child, Pediatric Dentistry.
Introduction
Ranula is a benign oral cystic lesion, infrequent in children, in the floor of the mouth and may extend into the cervical structures [1-3]. The treatment depends on the size and location, and is still quite controversial [3]. Treatment options can be surgical or not, and includes observation for possible spontaneous regression, aspiration of mucus, marsupialization, enucleation, resection/excision of the lesion and sublingual gland, among others [2-5].
Thus, this case reports a child, with bilateral ranula, in the floor of the mouth and her successful dental management, which includes two different types of treatment, with a rigorous clinical follow-up of 18 months.
Case Report
The patient, a 10 year old female, was referred to the Clinic of Pediatric Dentistry, with a chief complaint of swelling in the floor of the mouth realized 2 months previously.
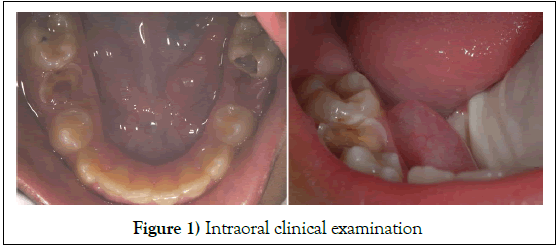
According to anamnesis, the medical history is not relevant. The extra oral clinical examination showed normality. During the intraoral clinical examination, a large floating, dome-shaped swelling was observed in the floor of the mouth bilaterally, associated with poor oral hygiene and gingival bleeding, was observed (Figure 1). Furthermore, the presence of extended active caries lesions, active white spots and root residual were observed.
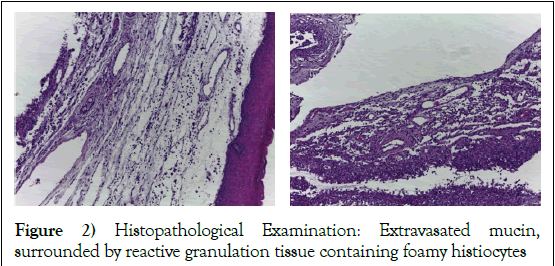
The treatment plan focused on solving the main complaint, because the size of the lesion compromised eating and speech, causing severe damage to the physical and social well being of the patient. During surgery, it was decided to perform the marsupialization of the smaller injury and enucleation of the bigger one, maintaining both glands. Histopathological examination revealed extravasated mucin, surrounded by reactive granulation tissue containing foamy histiocytes (Figure 2). These findings confirmed the initial clinical diagnosis of bilateral ranula.
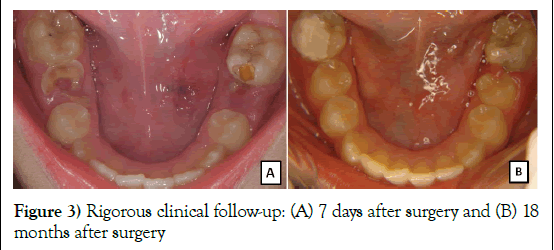
Despite the different types of treatment, both had good prognosis. Currently, the patient is in the final stage of treatment without recurrence of ranula or carious lesions and has a rigorous clinical follow-up of 18 months (Figure 3).
Figure 3: Rigorous clinical follow-up: (A) 7 days after surgery and (B) 18 months after surgery
Discussion
The major and minor salivary glands drain directly into the oral cavity and are responsible for the moisture of the mouth. In the case of obstruction in the outflow of the minor glands and mucus extravasation into tissues, this results in a mucocele. Ranula occurs by the same process, however, is usually associated with the sublingual gland [1]. In this report, beyond the relationship with the sublingual gland, the lesion appeared localized in the floor of the mouth, without expansion to the submental and submandibular spaces [4] featuring a simple ranula. Regarding the gender most affected, there is a balance between the accounts in children [3-5], although unilateral ranulas were more commonly observed [4,5] when compared to bilateral [3]. In this case, the patient was a female child with a bilateral lesion, which is more rare and complex to treat.
Clinically, the lesion presents as a floating, homogeneous and well-defined mass on the floor of the mouth [1,2] and the diagnosis is based on these features [2]. The initial clinical diagnosis of this report was confirmed by histopathological examination, corroborating other reports [4,5].
According to some authors, a 6 month observation period prior to surgery must be taken into account to assess possible spontaneous regression of the lesion (18.8% of cases, Zhi et al 2008), which may require a different treatment option for children [4]. Another study suggests that this period shall not exceed 3 months since there was no spontaneous regression, only increased lesions. In this report, there was no observation period due to the impairment of basic functions of the patient, such as feeding and speech.
The treatments reported in the literature vary according to the type, size and location of the ranula [3-5]. Marsupialization is indicated for cases of a simple ranula with a maximum of 2 cm [1,5] and also for cooperative patients [1]. The excision of the lesion and the sublingual gland has a low rate of recurrence compared to marsupialization, however, it is considered a radical treatment, and is often restricted to plunging ranulas [1,2,4,5]. In these cases, the other glands begin to compensate for the excised gland.
Despite the treatment plan including preventive, restorative and prosthetic dental procedures, its focus was on resolving the main complaint. During surgery, we opted for conservative maneuvers, because these were simple, small ranulas and involved on both sides. Although conservative treatments have higher rates of recurrence [1,2,4,5] no recurrence or complications were observed in this case.
Conclusion
An accurate diagnosis and an appropriate treatment plan are fundamental for a successful treatment of ranulas in children. Regardless of the surgical technique conservative maneuvers associated with careful clinical monitoring were indispensable for the longevity and success of treatment.
Acknowledgement
The authors are indebted to the participant and the family of the case report.
REFERENCES
- Kim MD, Alfred S. Treatment of ranulas. Operative Techniques in Otolaryngology 2008;19:240-42.
- Raju R, Digoy GP. Management of the pediatric ranula. Operat Techniq Otolaryngo 2009;20:260-62.
- Zhi KQ, Wen YM, Zhou H. Management of the pediatric plunging ranula: results of 15 years’ clinical experience. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009;107:499-502.
- Zhi K, When Y, Ren W, et al. Management of infant ranula. Int J Pediatr Otorhinolaryn 2008;72:823-26.
- Morita Y, Sato K, Kawana M, et al. Treatment of ranula–excision of the sublingual gland versus marsupialization. Auris, Nasus, Larynx 2003;30:311-14.