Thymic mucosa-associated lymphoid tissue lymphoma in a patient with Sjögren's syndrome
Received: 09-Dec-2021, Manuscript No. PULHHR-21-4022; Editor assigned: 11-Dec-2021, Pre QC No. PULHHR-21-4022; Accepted Date: Dec 30, 2021; Reviewed: 22-Dec-2021 QC No. PULHHR-21-4022; Revised: 27-Dec-2021, Manuscript No. PULHHR-21-4022; Published: 06-Jan-2022, DOI: 10.37532/pulhhr.22.6(1).39-40
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
A 52-year-old woman with Sjögren's syndrome and immunologic thrombocytopenic purpura was found to have a mediastinal tumor. Preoperative examination revealed the patient suffered from a severe thrombocytopenia and even has a rare blood group: O D+ (D+c+c+E+E+). Resection of the mediastinal tumor using Video-Assisted Thoracic Surgery (VATS) after thoroughly prepared including thrombocyte transfusion. Histopathologic examination and immunohistochemistry of the thymus tumor were both consistent with Mucosa-Associated Lymphoid Tissue (MALT) lymphoma. This rare case suggests that thymic MALT lymphoma can develop with an autoimmunue disease such as Sjögren's syndrome, surgical resection of thymic tumor should be performed after careful preoperative prepration.
Keywords
Syndrome; Lymphoid tissue; MALT lymphoma; B-cell
Introduction
Mucosa-Associated Lymphoid Tissue (MALT) lymphoma is an extranodal low-grade B-cell lymphoma that occurs in MALT usually found in salivary glands, thyroid gland, lungs, urinary bladder, gastrointestinal tract, and skin [1]. MALT lymphoma rarely involves the thymus gland. We recently treated a case of simultaneous MALT lymphoma in the thymus gland with Sjögren’s syndrome and immunologic thrombocytopenic purpura. We hereby highlight our experience in this case.
Thymic Mucosa-Associated Lymphoid Tissue (MALT) B-cell lymphoma in patient with Sjögren’s syndrome, immunologic thrombocytopenic purpura and is a rare blood group.
A 52-year-old woman was admitted to our hospital for treatment of thrombocytopenic purpura at the department of rheumatism and immunology. She had suffered from loss of teeth and dryness in the mouth for more than 10 years and also complained of dryness in eyes and arthralgia of proximal digital interosseous joints, wrist and knee joints in the last 5 years. 1 month ago, she had purpuric rashes in the lower extremities and blood test showed platelets counts were only 12/L × 109/L in local hospital.
The results for SS-A/Ro antibody and SS-B/La antibody were positive. Rheumatoid factor was positive (57.5 IU/mL), while serum levels of total protein, IgG, IgM, and IgA were normal. Eye examination revealed a positive Shirmer’s test (right eye:1 mm after 5 min and left eye:2 mm after 5 min).
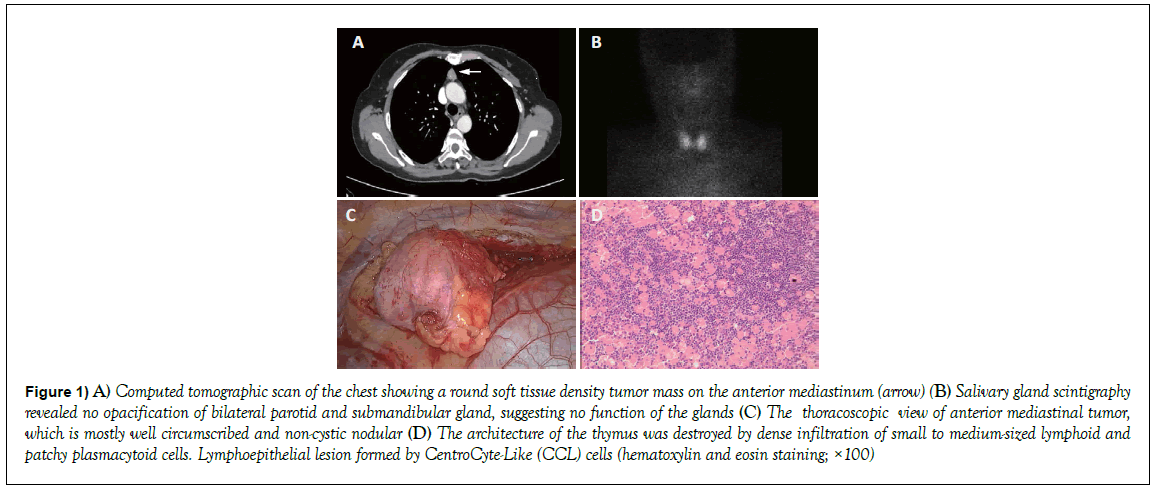
Salivary gland scintigraphy revealed no opacification of bilateral parotid and submandibular gland, suggesting no function of the glands (Figure 1). The patient fulfilled five of the six revised American-European Consensus Group Classification criteria in 2002 with xerostomia, xerophthalmia, positive Shirmer’s test, positive salivary gland scintigraphy, and positivity of SS-A/ Ro antibody and SS-B/La antibodies, and was confirmed as having definite Sjögren’s syndrome [2]. Further work-up included bone marrow puncture and chest CT in our hospital that revealed findings compatible with the diagnosis of immunologic thrombocytopenic purpura and thymic tumor. There is also found a special blood group: O D+ (D+c+c+E+E+ and full 4+ reaction with anti-D), which has a rare prevalence in irregular antibody [3]. So transfusion preparation was carefully done by blood bank. After platelets transfusion, hepatoprotection, corticosteroid therapy and intravenous gamma globulin, the patient was transferred into our department for elective operation to remove an anterior mediastinal tumor measuring 1.7 cm × 1.7 cm in size on the chest CT (Figure 1).
Figure 1: A) Computed tomographic scan of the chest showing a round soft tissue density tumor mass on the anterior mediastinum (arrow) (B) Salivary gland scintigraphy revealed no opacification of bilateral parotid and submandibular gland, suggesting no function of the glands (C) The thoracoscopic view of anterior mediastinal tumor, which is mostly well circumscribed and non-cystic nodular (D) The architecture of the thymus was destroyed by dense infiltration of small to medium-sized lymphoid and patchy plasmacytoid cells. Lymphoepithelial lesion formed by CentroCyte-Like (CCL) cells (hematoxylin and eosin staining; ×100)
The Video-Assisted Thoracic Surgery (VATS) thymectomy was performed without red blood cell transfusion in January 18, 2019, following a MDT discussion by thoracic surgeons, transfusion doctor, and anesthesiologist, hematologic and immunologic physician. Hence the diagnosis of the secondary thymic MALT associated with Sjögren’s syndrome was also made. At the 3-month follow-up after the operation, the symptom of dry eyes and mouth improved slightly, blood test shows platelets counts is 114/L × 109/L and there is no evidence of tumor recurrence.
Sjögren’s syndrome is a chronic autoimmune disease characterized by lymphocytic infiltration of the exocrine glands, specifically in the salivary glands, lacrimal glands and musculoskeletal system, resulting in xerostomia, xerophthalmia and arthralgia. Other systems or organs, such as respiratory, digestive, hematology system, and kidney, are also involves in this syndrome, leading to interstitial pneumonia, hepatic damage, thrombocytopenia, and renal dysfunction [4]. Immunologic thrombocytopenic purpura is a common acquired autoimmune disease. Both antibody-mediated platelet destruction and impaired platelet production are involved in its pathogenesis. About 5% of patients with Sjögren’s syndrome eventually develop lymphomas, while patients with Sjögren’s syndrome having a 44-fold increased risk of developing non-Hodgkin’s lymphoma. MALT lymphoma arising in the thymus is extremely rare, only 37 cases have been reported before [1, 5]. Chronic B-cell stimulation by these antibodies may contribute to the development of MALT lymphoma. Immunologic disorders are strongly associated with thymic MALT lymphoma tumorigenesis and that thymic MALT lymphoma did not cause these disorders [6]. The symptoms and antibody abnormalities can remains unimproved after thymectomy. Irregular antibodies screening is a routine preoperative test, because these harmful antibodies, e.g. anti-D, can result in severe hemolytic disease. In a retrospective review of 28303 Chinese (21327 Chinese) antenatal attendances from 1997 to 2001, it is found that the prevalence of clinically significant antibodies amongst Chinese pregnant women is 0.27% and there is only one case which has anti-c+anti-E irregular antibodies among the 58 Chinese women [3]. In another Indian study, it is found that the incidence of irregular antibody varies across different clinical disciplines. Cardiology and cardio-thoracic surgery, hepatology, oncology are the most common clinical disciplines [7]. According to our knowledge, however, the association between irregular antibody and thymic MALT lymphoma is unclear.
As for the surgical treatment of the patient, there are many critical points to achieve a well performance. Firstly, perioperative examination and preparation for clinical diagnosis and operative conditions, such as transfusion preparation, it is important to choose the appropriate patient to perform surgery and make the patient be able to tolerate the operation. Then, for complicated disease, especially in old people with much comorbidity, MDT should be taken into consideration by enough specialized doctor, such as surgeons, physicians, radiologists and anesthesiologists (Figure 1). Finally, postoperative management should focus on surgical complications, for instance, bleeding after operation due to wound errhysis and stress to decrease the platelets counts. To monitor postoperative condition, patient was warned to routine assessment in the outpatient clinic (Figure 1).
We here report one case, to our knowledge that is the first case of thymic MALT lymphoma associated with two rare parathymic syndromes: Sjögren’s syndrome, immunologic thrombocytopenic purpura and accompanying a rare blood group
Conflict of Interest
No potential conflict of interest relevant to this article could be reported. There is no financial support during this study.