Duplication of femoral vein and its significant clinical implications
Punita Sharma1* and Surinder Salwan2
1Department of Anatomy, Sri Guru Ram Das Institute of Medical Sciences and Research, Amritsar, India
2Department of Government Medical College, Amritsar, India
- *Corresponding Author:
- Punita Sharma
242, Medical Enclave Circular Road, Amritsar India
Tel: +91 183 2421508
E-mail: punitasalwan05@gmail.com
Date of Received: August 17th, 2011
Date of Accepted: November 28th, 2011
Published Online: December 12th 2011
© Int J Anat Var (IJAV). 2011; 4: 188–191.
[ft_below_content] =>Keywords
superficial femoral vein, misnomer, duplication, deep vein thrombosis
Introduction
The femoral vein accompanies the femoral artery, beginning at the opening in adductor magnus as the continuation of the popliteal vein, and ending at the level of inguinal ligament, by becoming the external iliac vein. In the lower part of the adductor canal it is posterolateral to the femoral artery; in the upper part of the canal, and in the lower part of the femoral triangle, it is behind the artery. At the base of the femoral triangle it is medial to the artery. The femoral vein has numerous muscular tributaries. The deep femoral vein joins the femoral vein posteriorly 4–12 cm distal to the inguinal ligament, and the great saphenous vein then enters anteriorly. Lateral and medial circumflex femoral veins are usually tributaries of the femoral vein [1].
The complex embryologic development of the vascular system often results in a myriad of clinically relevant variants. It has been stated that the classic anatomic venous pattern in the lower extremity is found in only 16 percent of patients [2].
The femoral region of the thigh is utilized for various clinical procedures, both open and closed, particularly with respect to arterial and venous cannulations. Venous pattern particularly in the lower limbs is of great clinical importance, while ligating the veins to prevent the spread of deep vein thrombosis [3].
Femoral vein catheterization is the easiest and safest method for obtaining temporary vascular access in hemodialysis patients. Therefore, an attempt has been made to report the case of duplication of femoral vein and elaborate its embryological and clinical aspects.
Case Report
While conducting dissection for undergraduate students, we came across the variation of femoral vein in an intact formaldehyde-preserved cadaver of a 42-year-old Indian male, in the department of Anatomy at Sri Guru Ram Das Institute of Medical Sciences and Research, Amritsar, India.
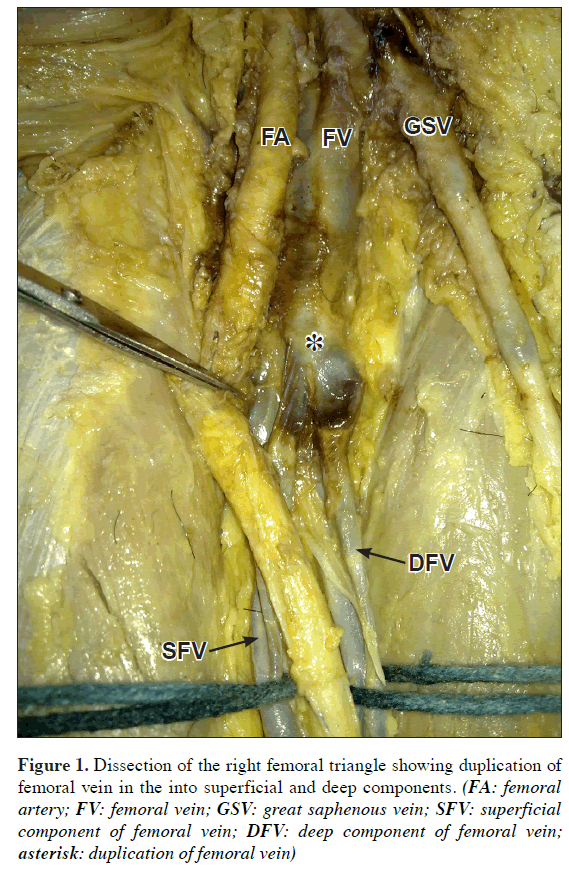
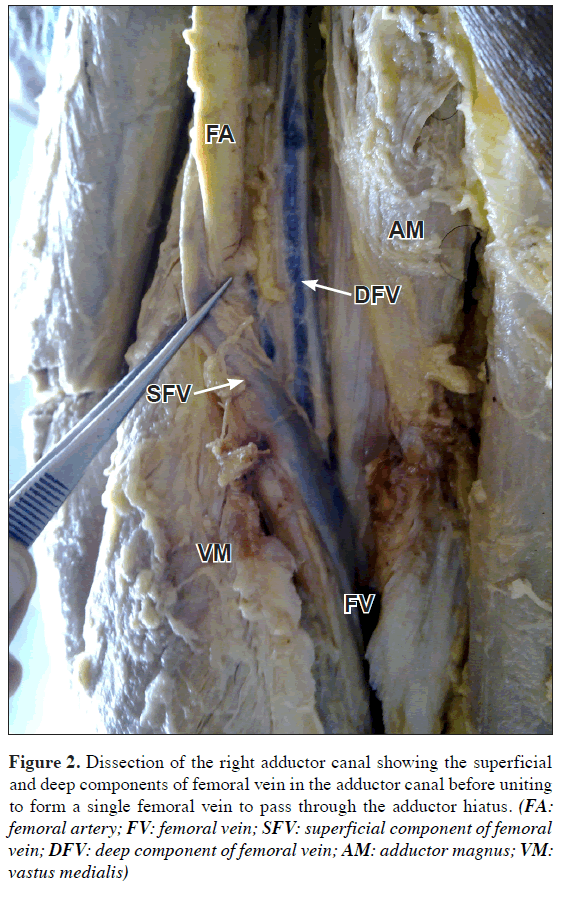
The right femoral vein was posterolateral to the femoral artery as it entered the adductor canal at the adductor hiatus. In the adductor canal, it divided into two veins at a distance of 5.5 cm above the adductor hiatus. Thus superficial and deep components of the femoral vein were formed. The superficial component wound around the anteromedial aspect of the femoral artery within the adductor canal to lie superficial to the artery; while the deep component ascended as the usual femoral vein, posterior to the femoral artery. In the femoral triangle, 8.5 cm below the inguinal ligament, the superficial ramus skirted around the anterolateral aspect of the femoral artery to unite with the deep component posterior to the femoral artery. Then the single femoral vein received the great saphenous vein 2.5 cm below the inguinal ligament and was placed medial to the femoral artery at the level of the inguinal ligament.
The superficial ramus received the lateral circumflex femoral vein while the single united femoral vein received the deep femoral and the medial circumflex veins.
The caliber of the femoral vein at the inguinal ligament was much larger than the femoral artery. The caliber of femoral vein at the inguinal ligament was 29 mm, while the caliber of the superficial and deep components was 11 and 15 mm, respectively.
The femoral vein and artery on the left side showed no variation.
Discussion
Before we start describing the embryological and clinical basis of femoral vein duplication, we take the liberty of clearing the mist concerning the terminology used for femoral vein because the misnomer attached to the femoral vein has significant clinical implications.
Figure 1: Dissection of the right femoral triangle showing duplication of femoral vein in the into superficial and deep components. (FA: femoral artery; FV: femoral vein; GSV: great saphenous vein; SFV: superficial component of femoral vein; DFV: deep component of femoral vein; asterisk: duplication of femoral vein)
Figure 2: Dissection of the right adductor canal showing the superficial and deep components of femoral vein in the adductor canal before uniting to form a single femoral vein to pass through the adductor hiatus. (FA: femoral artery; FV: femoral vein; SFV: superficial component of femoral vein; DFV: deep component of femoral vein; AM: adductor magnus; VM: vastus medialis)
Some specialist physicians (e.g., radiologists, and orthopedic/vascular surgeons) use the term “superficial femoral vein” (SFV) for the distal part of the “femoral vein” (FV) to differentiate the femoral vein segments before and after the “deep femoral vein” joins it, and differentiate the distal segment of the femoral vein from the “deep femoral vein” (DFV; profunda femoris vein), which is paired with the deep femoral (profunda femoris) artery [4].
The misleading and incorrect term ‘superficial femoral’ vein should never be used because the femoral vein is a deep vein and is not part of the superficial venous system. The incorrect term does not appear in any definitive anatomic atlas, as it is “not” recognized as a legitimate, yet it has come into common use in vascular laboratory practice. Confusion arising from use of the inappropriate name has been responsible for many cases of clinical mismanagement and death as patients (with deep vein thrombosis of femoral vein) are denied efficacious thrombolytic therapy [4].
Coming to the embryological basis of venous malformations (VM), the ‘truncular’ VM is one of two different types of the VMs, classified based on the stage where the developmental arrest/defect occurred. The truncular VM represents an embryologically defective vein where developmental arrest has occurred during the vascular trunk formation period in the ‘later stage’ of the embryonic development. This lesion no longer possesses the evolutional capacity to proliferate. On the hand, the ‘extratruncular’ VM represents a defective vein where developmental arrest has occurred during an ‘earlier stage’ of embryonic development and therefore maintains the mesenchymal cell properties and its evolutional ability to proliferate when stimulated [5].
Uhl et al. in their dissection study on fresh non-embalmed cadavers reported that venous malformations (truncular forms) occurring during the late development of the embryo produce several anatomical variations in the number and caliber of the main venous femoral trunks at the thigh level [6]. They concluded that the modal anatomy of the femoral vein was found in 308 of 336 limbs (88%). Truncular malformations were found in 28 of 336 limbs (12%); unitruncular configurations in 3% [axo femoral trunk [1%] and deep femoral trunk (2%)]. Bitruncular configurations were found in 9% [bifidity of the femoral vein (2%), femoral vein with axio-femoral trunk (5%), and femoral vein with deep femoral trunk (2%)]. Though truncular venous malformations of the femoral vein are not rare (12%), their knowledge is important for the investigation of the venous network, particularly the venous mapping of patients with cardiovascular disease.
It is also important to recognize a bitruncular configuration to avoid potential errors for the diagnosis of deep venous thrombosis of the femoral vein, in the case of an occluded duplicated trunk. Screaton et al. conducted a retrospective review of 381 venograms obtained after initial ultrasound findings were considered negative for thigh or popliteal thrombosis in patients in whom deep vein thrombosis was suspected [7]. False-negative ultrasound findings occurred in four (2%) of 204 patients with single femoral veins and in 10 (6%) of 177 patients with duplicated femoral veins. They made an important inference that the frequency of missed proximal thrombosis at ultrasound appears to be increased when duplicated superficial femoral veins are present, and imaging studies are insufficient to support the adoption of a totally noninvasive imaging strategy.
Liu et al. conducted ascending positive contrast venography on 337 lower extremities to determine whether there were any anatomic variations that might predispose to (deep vein thrombosis ) DVT and to explain why some many patients with DVT are asymptomatic. They concluded that one of factors responsible for “silent” DVT was multiple femoral veins. In these patients, complete occlusion by the thrombus is less likely because multiplicity may offer internal collaterals, preventing epifascial edema. Multiple FVs were found in 31% of the total limbs. Of the limbs with multiple FVs, 40% had DVT. This was a statistically higher incidence (p<0.001) than that seen in the 19% of those limbs with a single FV. Only 41% of the DVT limbs with multiple FVs were symptomatic; whereas 72% of DVT limbs with a single FV were symptomatic (p<0.001). While no difference was found relative to symptomatology and incidence of DVT between single and multiple popliteal veins [8].
Dona et al. designed a study to determine the incidence of duplications in individuals presenting for venous incompetence studies, and whether their presence could, in theory, act as a predisposing factor to DVT formation [9]. Duplex ultrasound examinations were performed in which venous duplications were actively searched for and recorded. The diameters of both limbs of any duplicated system and the single vessel immediately distal to it were recorded. Using these measurements, the changes in total cross-sectional area (CSA) associated with these variants was calculated. In addition, with the knowledge that the volume flow rate must remain constant, the velocity changes associated with such systems were calculated. Short-segment FV duplications were used to calculate the percentage change in total CSA and therefore blood flow velocities. Of the 13 (33%) suitable for such calculations, and calculating for each individual duplicated system, a mean increase in the vessel’s total CSA of 42%, which corresponded to a theoretical decrease in blood flow velocity of 36%, was found. The study confirmed the significantly high incidence of duplications of the PV and FV and the increase in the possibility of the potential for DVT formation secondary to changes in flow velocities. Perhaps the high incidence of DVT in multiple FVs can be explained by increased blood volume in the venous pool and conversely a decrease flow rate, which probably predisposes the limb to DVT [10,11].
To conclude, though truncular venous malformations of the femoral vein are not rare 12%, for the investigator, it may be clinically prudent to scan the opposite limb in the presence of venous duplication since femoral vein duplication is frequently bilateral. It should also be noted that a thrombus is more likely to be seen in one canal of a duplicated femoral vein than in the usual anatomy. Thus, a thrombus in that canal could be easily missed on ultrasound. Furthermore, for the surgeon, femoral vein duplication could provide the opportunity to use one of the trunks for deep vein transposition reconstruction surgery of the opposite limb [6].
References
- Standring S, ed. Gray’s Anatomy. 39th Ed., London, Elsevier. 2005; 543–547.
- Kerr TM, Smith JM, McKenna P, Lutter KS, Sampson MG, Helmchen RH, Roedersheimer LR. Venous and arterial anomalies of the lower extremities diagnosed by duplex scanning. Surg Gynecol Obstet. 1992; 175: 309–314.
- Bandyopadhyay M, Biswas S, Roy R. Vessels in femoral triangle in a rare relationship. Singapore Med J. 2010; 51: 3–5.
- Hammond I. The superficial femoral vein. Radiology. 2003; 229: 604–606.
- Lee BB, Laredo J, Neville R. Embryological background of truncular venous malformation in the extracranial venous pathways as the cause of chronic cerebrospinal venous insufficiency. Int Angiol. 2010; 29: 95–108.
- Uhl JF, Gillot C, Chahim M. Anatomical variations of the femoral vein. J Vasc Surg. 2010; 52: 714–719.
- Screaton NJ, Gillard JH, Berman LH, Kemp PM. Duplicated superficial femoral veins: a source of error in the sonographic investigation of deep vein thrombosis. Radiology. 1998; 206: 397–401.
- Liu GC, Ferris EJ, Reifsteck JR, Baker ME. Effect of anatomic variations on deep vein thrombosis of the lower extremity. AJR Am J Roentgenol. 1986; 146: 845–848.
- Dona E, Fletcher JP, Hughes TM, Saker K, Batiste P, Ramanathan I. Duplicated popliteal and superficial femoral veins: incidence and potential significance. Aust N Z J Surg. 2000; 70: 438–440.
- Sigel B, Edelstein AL, Felix WR Jr, Memhardt CR. Compression of the deep venous system of the lower leg during inactive recumbency. Arch Surg. 1973; 106: 38–43.
- Sevitt S. Etiology and pathogenesis of deep vein thrombosis. Lancet 1960; 275: 384–385.
Punita Sharma1* and Surinder Salwan2
1Department of Anatomy, Sri Guru Ram Das Institute of Medical Sciences and Research, Amritsar, India
2Department of Government Medical College, Amritsar, India
- *Corresponding Author:
- Punita Sharma
242, Medical Enclave Circular Road, Amritsar India
Tel: +91 183 2421508
E-mail: punitasalwan05@gmail.com
Date of Received: August 17th, 2011
Date of Accepted: November 28th, 2011
Published Online: December 12th 2011
© Int J Anat Var (IJAV). 2011; 4: 188–191.
Abstract
The complex embryologic development of the vascular system often results in a myriad of clinically relevant variants. The classic anatomic venous pattern in the lower extremity is found in only 16 percent of subjects with 2% occurrence of duplication of superficial femoral vein. A good clinical review of retrospective and prospective studies with various investigation modalities reveals an unprecedented relation between duplicated femoral veins and deep vein thrombosis. So the basic purpose or aim of reporting the case of duplication of femoral vein was to highlight the misnomer attached to the femoral vein and to emphasize through clinical review that more cases of proximal thrombosis have false-negative findings with duplication than with single femoral vein. Also, an attempt has been made to elaborate its embryological and clinical aspects in detail.
-Keywords
superficial femoral vein, misnomer, duplication, deep vein thrombosis
Introduction
The femoral vein accompanies the femoral artery, beginning at the opening in adductor magnus as the continuation of the popliteal vein, and ending at the level of inguinal ligament, by becoming the external iliac vein. In the lower part of the adductor canal it is posterolateral to the femoral artery; in the upper part of the canal, and in the lower part of the femoral triangle, it is behind the artery. At the base of the femoral triangle it is medial to the artery. The femoral vein has numerous muscular tributaries. The deep femoral vein joins the femoral vein posteriorly 4–12 cm distal to the inguinal ligament, and the great saphenous vein then enters anteriorly. Lateral and medial circumflex femoral veins are usually tributaries of the femoral vein [1].
The complex embryologic development of the vascular system often results in a myriad of clinically relevant variants. It has been stated that the classic anatomic venous pattern in the lower extremity is found in only 16 percent of patients [2].
The femoral region of the thigh is utilized for various clinical procedures, both open and closed, particularly with respect to arterial and venous cannulations. Venous pattern particularly in the lower limbs is of great clinical importance, while ligating the veins to prevent the spread of deep vein thrombosis [3].
Femoral vein catheterization is the easiest and safest method for obtaining temporary vascular access in hemodialysis patients. Therefore, an attempt has been made to report the case of duplication of femoral vein and elaborate its embryological and clinical aspects.
Case Report
While conducting dissection for undergraduate students, we came across the variation of femoral vein in an intact formaldehyde-preserved cadaver of a 42-year-old Indian male, in the department of Anatomy at Sri Guru Ram Das Institute of Medical Sciences and Research, Amritsar, India.
The right femoral vein was posterolateral to the femoral artery as it entered the adductor canal at the adductor hiatus. In the adductor canal, it divided into two veins at a distance of 5.5 cm above the adductor hiatus. Thus superficial and deep components of the femoral vein were formed. The superficial component wound around the anteromedial aspect of the femoral artery within the adductor canal to lie superficial to the artery; while the deep component ascended as the usual femoral vein, posterior to the femoral artery. In the femoral triangle, 8.5 cm below the inguinal ligament, the superficial ramus skirted around the anterolateral aspect of the femoral artery to unite with the deep component posterior to the femoral artery. Then the single femoral vein received the great saphenous vein 2.5 cm below the inguinal ligament and was placed medial to the femoral artery at the level of the inguinal ligament.
The superficial ramus received the lateral circumflex femoral vein while the single united femoral vein received the deep femoral and the medial circumflex veins.
The caliber of the femoral vein at the inguinal ligament was much larger than the femoral artery. The caliber of femoral vein at the inguinal ligament was 29 mm, while the caliber of the superficial and deep components was 11 and 15 mm, respectively.
The femoral vein and artery on the left side showed no variation.
Discussion
Before we start describing the embryological and clinical basis of femoral vein duplication, we take the liberty of clearing the mist concerning the terminology used for femoral vein because the misnomer attached to the femoral vein has significant clinical implications.
Figure 1: Dissection of the right femoral triangle showing duplication of femoral vein in the into superficial and deep components. (FA: femoral artery; FV: femoral vein; GSV: great saphenous vein; SFV: superficial component of femoral vein; DFV: deep component of femoral vein; asterisk: duplication of femoral vein)
Figure 2: Dissection of the right adductor canal showing the superficial and deep components of femoral vein in the adductor canal before uniting to form a single femoral vein to pass through the adductor hiatus. (FA: femoral artery; FV: femoral vein; SFV: superficial component of femoral vein; DFV: deep component of femoral vein; AM: adductor magnus; VM: vastus medialis)
Some specialist physicians (e.g., radiologists, and orthopedic/vascular surgeons) use the term “superficial femoral vein” (SFV) for the distal part of the “femoral vein” (FV) to differentiate the femoral vein segments before and after the “deep femoral vein” joins it, and differentiate the distal segment of the femoral vein from the “deep femoral vein” (DFV; profunda femoris vein), which is paired with the deep femoral (profunda femoris) artery [4].
The misleading and incorrect term ‘superficial femoral’ vein should never be used because the femoral vein is a deep vein and is not part of the superficial venous system. The incorrect term does not appear in any definitive anatomic atlas, as it is “not” recognized as a legitimate, yet it has come into common use in vascular laboratory practice. Confusion arising from use of the inappropriate name has been responsible for many cases of clinical mismanagement and death as patients (with deep vein thrombosis of femoral vein) are denied efficacious thrombolytic therapy [4].
Coming to the embryological basis of venous malformations (VM), the ‘truncular’ VM is one of two different types of the VMs, classified based on the stage where the developmental arrest/defect occurred. The truncular VM represents an embryologically defective vein where developmental arrest has occurred during the vascular trunk formation period in the ‘later stage’ of the embryonic development. This lesion no longer possesses the evolutional capacity to proliferate. On the hand, the ‘extratruncular’ VM represents a defective vein where developmental arrest has occurred during an ‘earlier stage’ of embryonic development and therefore maintains the mesenchymal cell properties and its evolutional ability to proliferate when stimulated [5].
Uhl et al. in their dissection study on fresh non-embalmed cadavers reported that venous malformations (truncular forms) occurring during the late development of the embryo produce several anatomical variations in the number and caliber of the main venous femoral trunks at the thigh level [6]. They concluded that the modal anatomy of the femoral vein was found in 308 of 336 limbs (88%). Truncular malformations were found in 28 of 336 limbs (12%); unitruncular configurations in 3% [axo femoral trunk [1%] and deep femoral trunk (2%)]. Bitruncular configurations were found in 9% [bifidity of the femoral vein (2%), femoral vein with axio-femoral trunk (5%), and femoral vein with deep femoral trunk (2%)]. Though truncular venous malformations of the femoral vein are not rare (12%), their knowledge is important for the investigation of the venous network, particularly the venous mapping of patients with cardiovascular disease.
It is also important to recognize a bitruncular configuration to avoid potential errors for the diagnosis of deep venous thrombosis of the femoral vein, in the case of an occluded duplicated trunk. Screaton et al. conducted a retrospective review of 381 venograms obtained after initial ultrasound findings were considered negative for thigh or popliteal thrombosis in patients in whom deep vein thrombosis was suspected [7]. False-negative ultrasound findings occurred in four (2%) of 204 patients with single femoral veins and in 10 (6%) of 177 patients with duplicated femoral veins. They made an important inference that the frequency of missed proximal thrombosis at ultrasound appears to be increased when duplicated superficial femoral veins are present, and imaging studies are insufficient to support the adoption of a totally noninvasive imaging strategy.
Liu et al. conducted ascending positive contrast venography on 337 lower extremities to determine whether there were any anatomic variations that might predispose to (deep vein thrombosis ) DVT and to explain why some many patients with DVT are asymptomatic. They concluded that one of factors responsible for “silent” DVT was multiple femoral veins. In these patients, complete occlusion by the thrombus is less likely because multiplicity may offer internal collaterals, preventing epifascial edema. Multiple FVs were found in 31% of the total limbs. Of the limbs with multiple FVs, 40% had DVT. This was a statistically higher incidence (p<0.001) than that seen in the 19% of those limbs with a single FV. Only 41% of the DVT limbs with multiple FVs were symptomatic; whereas 72% of DVT limbs with a single FV were symptomatic (p<0.001). While no difference was found relative to symptomatology and incidence of DVT between single and multiple popliteal veins [8].
Dona et al. designed a study to determine the incidence of duplications in individuals presenting for venous incompetence studies, and whether their presence could, in theory, act as a predisposing factor to DVT formation [9]. Duplex ultrasound examinations were performed in which venous duplications were actively searched for and recorded. The diameters of both limbs of any duplicated system and the single vessel immediately distal to it were recorded. Using these measurements, the changes in total cross-sectional area (CSA) associated with these variants was calculated. In addition, with the knowledge that the volume flow rate must remain constant, the velocity changes associated with such systems were calculated. Short-segment FV duplications were used to calculate the percentage change in total CSA and therefore blood flow velocities. Of the 13 (33%) suitable for such calculations, and calculating for each individual duplicated system, a mean increase in the vessel’s total CSA of 42%, which corresponded to a theoretical decrease in blood flow velocity of 36%, was found. The study confirmed the significantly high incidence of duplications of the PV and FV and the increase in the possibility of the potential for DVT formation secondary to changes in flow velocities. Perhaps the high incidence of DVT in multiple FVs can be explained by increased blood volume in the venous pool and conversely a decrease flow rate, which probably predisposes the limb to DVT [10,11].
To conclude, though truncular venous malformations of the femoral vein are not rare 12%, for the investigator, it may be clinically prudent to scan the opposite limb in the presence of venous duplication since femoral vein duplication is frequently bilateral. It should also be noted that a thrombus is more likely to be seen in one canal of a duplicated femoral vein than in the usual anatomy. Thus, a thrombus in that canal could be easily missed on ultrasound. Furthermore, for the surgeon, femoral vein duplication could provide the opportunity to use one of the trunks for deep vein transposition reconstruction surgery of the opposite limb [6].
References
- Standring S, ed. Gray’s Anatomy. 39th Ed., London, Elsevier. 2005; 543–547.
- Kerr TM, Smith JM, McKenna P, Lutter KS, Sampson MG, Helmchen RH, Roedersheimer LR. Venous and arterial anomalies of the lower extremities diagnosed by duplex scanning. Surg Gynecol Obstet. 1992; 175: 309–314.
- Bandyopadhyay M, Biswas S, Roy R. Vessels in femoral triangle in a rare relationship. Singapore Med J. 2010; 51: 3–5.
- Hammond I. The superficial femoral vein. Radiology. 2003; 229: 604–606.
- Lee BB, Laredo J, Neville R. Embryological background of truncular venous malformation in the extracranial venous pathways as the cause of chronic cerebrospinal venous insufficiency. Int Angiol. 2010; 29: 95–108.
- Uhl JF, Gillot C, Chahim M. Anatomical variations of the femoral vein. J Vasc Surg. 2010; 52: 714–719.
- Screaton NJ, Gillard JH, Berman LH, Kemp PM. Duplicated superficial femoral veins: a source of error in the sonographic investigation of deep vein thrombosis. Radiology. 1998; 206: 397–401.
- Liu GC, Ferris EJ, Reifsteck JR, Baker ME. Effect of anatomic variations on deep vein thrombosis of the lower extremity. AJR Am J Roentgenol. 1986; 146: 845–848.
- Dona E, Fletcher JP, Hughes TM, Saker K, Batiste P, Ramanathan I. Duplicated popliteal and superficial femoral veins: incidence and potential significance. Aust N Z J Surg. 2000; 70: 438–440.
- Sigel B, Edelstein AL, Felix WR Jr, Memhardt CR. Compression of the deep venous system of the lower leg during inactive recumbency. Arch Surg. 1973; 106: 38–43.
- Sevitt S. Etiology and pathogenesis of deep vein thrombosis. Lancet 1960; 275: 384–385.