A new type of non-recurrent inferior laryngeal nerve in a cadaver with a right retroesophageal subclavian artery
Newton BW*, Rodgers SA, Rau JN, Hong MY, Terreberry RR
Department of Anatomy, Campbell University Jerry M. Wallace School of Osteopathic Medicine, Lillington, North Carolina, USA.
- *Corresponding Author:
- Bruce W. Newton
Department of Anatomy
Campbell University Jerry M. Wallace School of Osteopathic Medicine
Lillington, North Carolina, 27546, USA
Telephone 1-910-893-7306
E-mail: bnewton@campbell.edu
Published Online: 2 June 2017
Citation : Newton BW, Rodgers SA, Rau JN, et al. A new type of non-recurrent inferior laryngeal nerve in a cadaver with a right retro esophageal subclavian artery. Int J Anat Var. 2017;10(2):018-19.
© This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http:// creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
[ft_below_content] =>Keywords
Larynx, Laryngeal nerve, Superior laryngeal nerve, Recurrent laryngeal nerve injury, Thyroidectomy, Vagus nerve
Introduction
A retroesophageal right subclavian artery (arteria lusoria) is the most common developmental anomaly of the aortic arch [1]. Variant right subclavian arteries are classified as being either: Type I, where right subclavian artery courses posterior to the esophagus (80-84% of cases); Type II, where right subclavian artery courses between the esophagus and trachea (13-15% of cases); and Type III, where right subclavian artery courses anterior to the trachea (4-5% of cases) [2]. The Type I variation described by Shenoy et al. is also termed Type G by Araújo et al. and Donadel et al. [1-3].
Normally, the right recurrent laryngeal nerve branches off the right vagus nerve inferior to the right subclavian artery and loops around the artery before ascending between the trachea and esophagus to enter the inferior aspect of the larynx where the name changes to the right inferior laryngeal nerve. However, due to arteria lusoria the right recurrent laryngeal nerve follows an atypical course and is called a non-recurrent inferior laryngeal nerve (NRILN). Three types of a NRILN have been previously described: Type 1A–the NRILN courses straight to the larynx at the level of the upper thyroid pole; Type 1B–courses transversely at the level of the thyroid isthmus; and Type II–courses inferiorly to the inferior thyroid pole before slightly looping back to enter the larynx [4]. Regardless of its course, the inferior laryngeal nerve, or a NRILN, innervates all of the intrinsic muscles of larynx, except for the cricothyroid muscle, and is, therefore, asymptomatic unless iatrogenically-injured.
Materials and Methods
During the dissection of a 93-year-old female cadaver by students in a medical gross anatomy course, an aberrant right subclavian artery with an associated NRILN was found. Photographs of the artery and NRILN were taken after the head was thoroughly dissected.s
Results
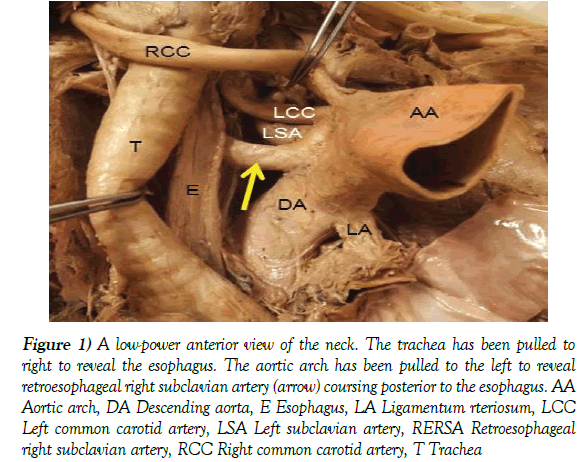
Figure 1 demonstrates the position of the right retroesophageal subclavian artery in this cadaver, and shows it arising from the most distal aspect of the aortic arch immediately distal to the origin of the left subclavian artery. This is a Type I, Type G or Type IV variation as described by Shenoy et al. and Donadel et al. [1,2] Because the right subclavian artery was retroesophageal, the right common carotid artery arose as a separate branch off the aortic arch, and there was no brachiocephalic trunk.
Figure 1: A low-power anterior view of the neck. The trachea has been pulled to right to reveal the esophagus. The aortic arch has been pulled to the left to reveal retroesophageal right subclavian artery (arrow) coursing posterior to the esophagus. AA Aortic arch, DA Descending aorta, E Esophagus, LA Ligamentum rteriosum, LCC Left common carotid artery, LSA Left subclavian artery, RERSA Retroesophageal right subclavian artery, RCC Right common carotid artery, T Trachea
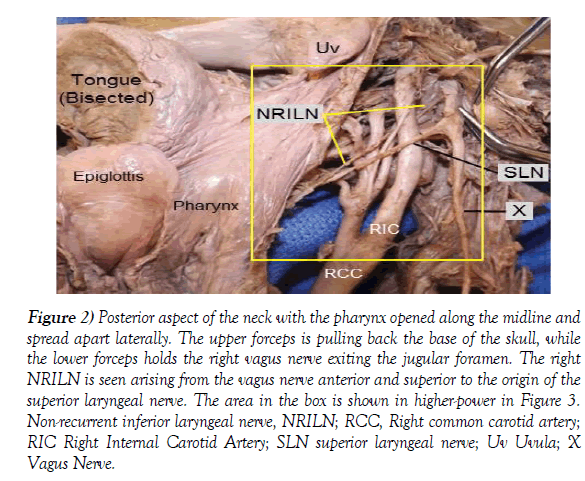
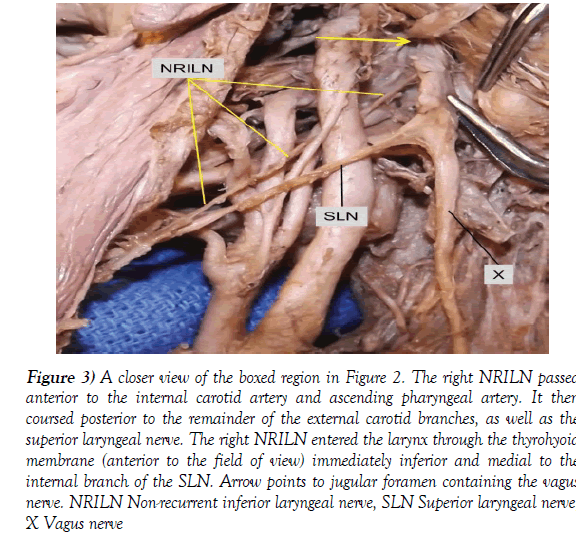
A posterior view of the NRILN course is shown in Figures 2 and 3. The NRILN arose from the right vagus nerve immediately after the vagus had exited the jugular foramen. It descended medially in the neck, crossed lateral to the internal carotid artery and medial to all the branches of the external carotid artery with the exception of the ascending pharyngeal artery. With approximately 0.5 cm of its length remaining, the NRILN crossed medial to the internal branch right superior laryngeal nerve. The NRILN then entered the larynx through the thyrohyoid membrane inferior to the superior laryngeal nerve.
Figure 2: Posterior aspect of the neck with the pharynx opened along the midline and spread apart laterally. The upper forceps is pulling back the base of the skull, while the lower forceps holds the right vagus nerve exiting the jugular foramen. The right NRILN is seen arising from the vagus nerve anterior and superior to the origin of the superior laryngeal nerve. The area in the box is shown in higher-power in Figure 3. Non-recurrent inferior laryngeal nerve, NRILN; RCC, Right common carotid artery; RIC Right Internal Carotid Artery; SLN superior laryngeal nerve; Uv Uvula; X Vagus Nerve.
Figure 3: A closer view of the boxed region in Figure 2. The right NRILN passed anterior to the internal carotid artery and ascending pharyngeal artery. It then coursed posterior to the remainder of the external carotid branches, as well as the superior laryngeal nerve. The right NRILN entered the larynx through the thyrohyoid membrane (anterior to the field of view) immediately inferior and medial to the internal branch of the SLN. Arrow points to jugular foramen containing the vagus nerve. NRILN Non-recurrent inferior laryngeal nerve, SLN Superior laryngeal nerve, X Vagus nerve
Discussion
The female cadaver in this study had a retroesophageal right subclavian artery. Most right retroesophageal subclavian arteries are found retrospectively during surgery since 90-93% of the people with arteria lusoria are asymptomatic [3]. However, it is important to note that the presence of an aberrant right subclavian artery provides an accurate predictor of the presence of a NRILN [2].
A right NRILN has a population prevalence of 0-3.9% with over 99.5% of NRILNs occurring on the right side [5]. Patients with a NRILN do not present with impaired function, since the NRILN continues to innervate the same laryngeal structures as a normal inferior laryngeal nerve. Therefore, the presence of a NRILN is often found incidentally, e.g., during thyroidectomies [4,5]. Since the authors do not have access to the medical history of the woman described in this case, it is unknown if the aberrant course of the right NRILN caused any difficulties; but was most likely asymptomatic. However, the retroesophageal right subclavian artery may have caused dysphagia, dyspnea and/or retrosternal pain [3].
When not properly identified during neck surgical procedures, injuries to the NRILN may be sustained, resulting in paralysis of the ipsilateral vocal cord with resultant voice hoarseness. In order to reduce the risk of injury, it is imperative head and neck surgeons acknowledge the potential presence of a NRILN prior to performing a procedure. Importantly, whereas the Type I and Type II NRILN have been described, the right NRILN in this cadaver has not, to our knowledge, been previously described in the literature. This new NRILN variant arising from the vagus nerve extremely high in the neck and entering the thyrohyoid membrane cannot be classified as a previously described type; therefore, this new variant is termed a “Type III NRILN”. Moving forward, it is imperative to document the course of this new Type III NRILN variant in order to increase preoperative awareness and further reduce potential surgical complications, e.g., during neck dissection, thyroidectomy, and carotid endarterectomy [2,4].
Acknowledgements
The authors gratefully thank the individuals who donate their bodies to support medical education. This project was made possible by internal support and funding by the Campbell University Jerry M. Wallace School of Osteopathic Medicine.
Conflict of interest
Newton BW, Ph.D., takes responsibility for the integrity of the content of the paper.
References
- Donadel MM, Lontra MB, Cavazzola LT, et al. Retroesophageal right subclavian artery: A case report and review of literature. Eur J Anat. 2006;10(3):57-60.
- Shenoy AM, Nanjundappa A, Halkud R, et al. Retroesophageal right subclavian artery with nonrecurrent laryngeal nerve: Unique variation of surgical importance. World J Endocr Surg. 2013;5(2):33-8.
- Araújo G, Bizzi JWJ, Muller J, et al. “Dysphagia lusoria”–Right subclavian retroesophageal artery causing intermittent esophageal compression and eventual dysphagia–A case report and literature review. Int J Surg Case Rep. 2015;10:32-4.
- Defechereux T, Albert V, Alexandre J, et al. The inferior non recurrent laryngeal nerve: A major surgical risk during thyroidectomy. Acta Chir Belg. 2000;100:62-7.
- Casal D, Peças A, Sousa D, et al. A non-recurrent inferior laryngeal nerve in a man undergoing thyroidectomy: A case report. J Med Case Rep. 2010;4:386.
Newton BW*, Rodgers SA, Rau JN, Hong MY, Terreberry RR
Department of Anatomy, Campbell University Jerry M. Wallace School of Osteopathic Medicine, Lillington, North Carolina, USA.
- *Corresponding Author:
- Bruce W. Newton
Department of Anatomy
Campbell University Jerry M. Wallace School of Osteopathic Medicine
Lillington, North Carolina, 27546, USA
Telephone 1-910-893-7306
E-mail: bnewton@campbell.edu
Published Online: 2 June 2017
Citation : Newton BW, Rodgers SA, Rau JN, et al. A new type of non-recurrent inferior laryngeal nerve in a cadaver with a right retro esophageal subclavian artery. Int J Anat Var. 2017;10(2):018-19.
© This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http:// creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
The presence of the retroesophageal right subclavian artery predicts the presence of a right non-recurrent inferior laryngeal nerve (NRILN). Three different right NRILNs have been previously described: Types Ia, Ib and II. This case describes a new variant of right NRILN, termed Type III, which arises from the vagus nerve as it exits the jugular foramen. Unlike previously described NRILNs, which enter the inferior aspect of the larynx, the Type III NRILN enters the larynx through the thyrohyoid membrane. The unusual course of the Type III NRILN makes it vulnerable to injury during neck surgeries.
-Keywords
Larynx, Laryngeal nerve, Superior laryngeal nerve, Recurrent laryngeal nerve injury, Thyroidectomy, Vagus nerve
Introduction
A retroesophageal right subclavian artery (arteria lusoria) is the most common developmental anomaly of the aortic arch [1]. Variant right subclavian arteries are classified as being either: Type I, where right subclavian artery courses posterior to the esophagus (80-84% of cases); Type II, where right subclavian artery courses between the esophagus and trachea (13-15% of cases); and Type III, where right subclavian artery courses anterior to the trachea (4-5% of cases) [2]. The Type I variation described by Shenoy et al. is also termed Type G by Araújo et al. and Donadel et al. [1-3].
Normally, the right recurrent laryngeal nerve branches off the right vagus nerve inferior to the right subclavian artery and loops around the artery before ascending between the trachea and esophagus to enter the inferior aspect of the larynx where the name changes to the right inferior laryngeal nerve. However, due to arteria lusoria the right recurrent laryngeal nerve follows an atypical course and is called a non-recurrent inferior laryngeal nerve (NRILN). Three types of a NRILN have been previously described: Type 1A–the NRILN courses straight to the larynx at the level of the upper thyroid pole; Type 1B–courses transversely at the level of the thyroid isthmus; and Type II–courses inferiorly to the inferior thyroid pole before slightly looping back to enter the larynx [4]. Regardless of its course, the inferior laryngeal nerve, or a NRILN, innervates all of the intrinsic muscles of larynx, except for the cricothyroid muscle, and is, therefore, asymptomatic unless iatrogenically-injured.
Materials and Methods
During the dissection of a 93-year-old female cadaver by students in a medical gross anatomy course, an aberrant right subclavian artery with an associated NRILN was found. Photographs of the artery and NRILN were taken after the head was thoroughly dissected.s
Results
Figure 1 demonstrates the position of the right retroesophageal subclavian artery in this cadaver, and shows it arising from the most distal aspect of the aortic arch immediately distal to the origin of the left subclavian artery. This is a Type I, Type G or Type IV variation as described by Shenoy et al. and Donadel et al. [1,2] Because the right subclavian artery was retroesophageal, the right common carotid artery arose as a separate branch off the aortic arch, and there was no brachiocephalic trunk.
Figure 1: A low-power anterior view of the neck. The trachea has been pulled to right to reveal the esophagus. The aortic arch has been pulled to the left to reveal retroesophageal right subclavian artery (arrow) coursing posterior to the esophagus. AA Aortic arch, DA Descending aorta, E Esophagus, LA Ligamentum rteriosum, LCC Left common carotid artery, LSA Left subclavian artery, RERSA Retroesophageal right subclavian artery, RCC Right common carotid artery, T Trachea
A posterior view of the NRILN course is shown in Figures 2 and 3. The NRILN arose from the right vagus nerve immediately after the vagus had exited the jugular foramen. It descended medially in the neck, crossed lateral to the internal carotid artery and medial to all the branches of the external carotid artery with the exception of the ascending pharyngeal artery. With approximately 0.5 cm of its length remaining, the NRILN crossed medial to the internal branch right superior laryngeal nerve. The NRILN then entered the larynx through the thyrohyoid membrane inferior to the superior laryngeal nerve.
Figure 2: Posterior aspect of the neck with the pharynx opened along the midline and spread apart laterally. The upper forceps is pulling back the base of the skull, while the lower forceps holds the right vagus nerve exiting the jugular foramen. The right NRILN is seen arising from the vagus nerve anterior and superior to the origin of the superior laryngeal nerve. The area in the box is shown in higher-power in Figure 3. Non-recurrent inferior laryngeal nerve, NRILN; RCC, Right common carotid artery; RIC Right Internal Carotid Artery; SLN superior laryngeal nerve; Uv Uvula; X Vagus Nerve.
Figure 3: A closer view of the boxed region in Figure 2. The right NRILN passed anterior to the internal carotid artery and ascending pharyngeal artery. It then coursed posterior to the remainder of the external carotid branches, as well as the superior laryngeal nerve. The right NRILN entered the larynx through the thyrohyoid membrane (anterior to the field of view) immediately inferior and medial to the internal branch of the SLN. Arrow points to jugular foramen containing the vagus nerve. NRILN Non-recurrent inferior laryngeal nerve, SLN Superior laryngeal nerve, X Vagus nerve
Discussion
The female cadaver in this study had a retroesophageal right subclavian artery. Most right retroesophageal subclavian arteries are found retrospectively during surgery since 90-93% of the people with arteria lusoria are asymptomatic [3]. However, it is important to note that the presence of an aberrant right subclavian artery provides an accurate predictor of the presence of a NRILN [2].
A right NRILN has a population prevalence of 0-3.9% with over 99.5% of NRILNs occurring on the right side [5]. Patients with a NRILN do not present with impaired function, since the NRILN continues to innervate the same laryngeal structures as a normal inferior laryngeal nerve. Therefore, the presence of a NRILN is often found incidentally, e.g., during thyroidectomies [4,5]. Since the authors do not have access to the medical history of the woman described in this case, it is unknown if the aberrant course of the right NRILN caused any difficulties; but was most likely asymptomatic. However, the retroesophageal right subclavian artery may have caused dysphagia, dyspnea and/or retrosternal pain [3].
When not properly identified during neck surgical procedures, injuries to the NRILN may be sustained, resulting in paralysis of the ipsilateral vocal cord with resultant voice hoarseness. In order to reduce the risk of injury, it is imperative head and neck surgeons acknowledge the potential presence of a NRILN prior to performing a procedure. Importantly, whereas the Type I and Type II NRILN have been described, the right NRILN in this cadaver has not, to our knowledge, been previously described in the literature. This new NRILN variant arising from the vagus nerve extremely high in the neck and entering the thyrohyoid membrane cannot be classified as a previously described type; therefore, this new variant is termed a “Type III NRILN”. Moving forward, it is imperative to document the course of this new Type III NRILN variant in order to increase preoperative awareness and further reduce potential surgical complications, e.g., during neck dissection, thyroidectomy, and carotid endarterectomy [2,4].
Acknowledgements
The authors gratefully thank the individuals who donate their bodies to support medical education. This project was made possible by internal support and funding by the Campbell University Jerry M. Wallace School of Osteopathic Medicine.
Conflict of interest
Newton BW, Ph.D., takes responsibility for the integrity of the content of the paper.
References
- Donadel MM, Lontra MB, Cavazzola LT, et al. Retroesophageal right subclavian artery: A case report and review of literature. Eur J Anat. 2006;10(3):57-60.
- Shenoy AM, Nanjundappa A, Halkud R, et al. Retroesophageal right subclavian artery with nonrecurrent laryngeal nerve: Unique variation of surgical importance. World J Endocr Surg. 2013;5(2):33-8.
- Araújo G, Bizzi JWJ, Muller J, et al. “Dysphagia lusoria”–Right subclavian retroesophageal artery causing intermittent esophageal compression and eventual dysphagia–A case report and literature review. Int J Surg Case Rep. 2015;10:32-4.
- Defechereux T, Albert V, Alexandre J, et al. The inferior non recurrent laryngeal nerve: A major surgical risk during thyroidectomy. Acta Chir Belg. 2000;100:62-7.
- Casal D, Peças A, Sousa D, et al. A non-recurrent inferior laryngeal nerve in a man undergoing thyroidectomy: A case report. J Med Case Rep. 2010;4:386.