An accessory muscle of the thoracic wall
Md Hassan Ali and Mohamed Hassan Eweidah*
Department of Anatomy, College of Medicine, Al-Jouf University, Sakaka, Al-Jouf Kingdom of Saudi Arabia.
- *Corresponding Author:
- Mohamed Hassan Eweidah
Associate Professor of Anatomy, College of Medicine, Al-Jouf University, PO Box 2014, Sakaka Al-Jouf,Saudi Arabia.
Tel: +966 555875425
E-mail: eweidah@yahoo.com
Date of Received : December 14th, 2009
Date of Accepted : February 23rd, 2010
Published Online : February 28th, 2010
© IJAV. 2010; 3: 33–35.
[ft_below_content] =>Keywords
sciatic nerve,genicular branch,sural nerve,common peroneal nerve,nerve transplantation
Introduction
Sciatic nerve, the largest branch of the sacral plexus originates from the L4-S3 roots, emerges from the greater sciatic foramen and passes inferior to the piriformis muscle between the ischial tuberosity and the greater trochanter of the femur. The nerve divides most frequently at the level of the upper angle of the popliteal fossa into tibial and common peroneal branches [1]. Both the tibial and the common peroneal nerves give muscular, cutaneous and genicular branches. The medial sural cutaneous nerve from tibial nerve or peroneal communicating nerve from common peroneal nerve may continue as sural nerve which supplies the lateral surface of the leg, gives off the lateral branches to the heel and the lateral dorsal cutaneous nerve [2].
We here present a case of bilateral high division of the sciatic nerves together with a unilateral (left) unusual high genicular branch of the common peroneal nerve and bilateral unusual thick peroneal communicating nerves.
Case Report
Case Report
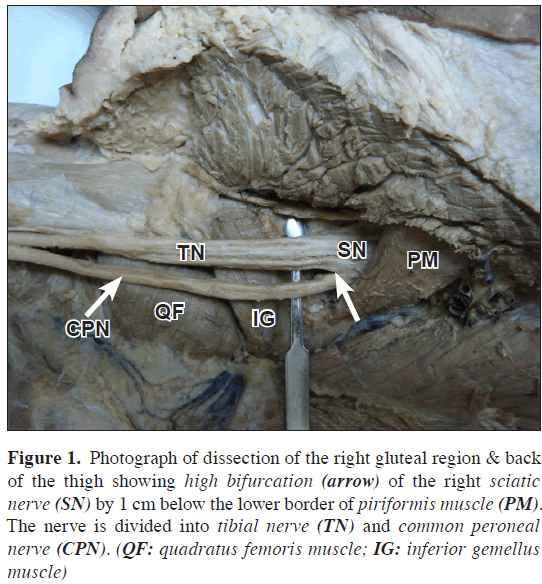
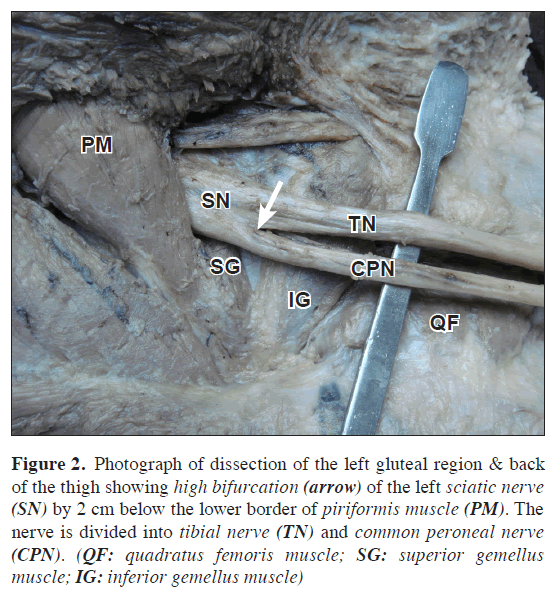
During the routine dissection for medical undergraduates in the College of Medicine, Al-Jouf University, Kingdom of Saudi Arabia, a bilateral high bifurcation of the sciatic nerves in a 50-year-old male Filipino cadaver was noticed. The sciatic nerve terminated 2 cm (on the left side) and 1 cm (on the right side) below the lower border of the piriformis muscle, about 41 cm from the popliteal skin crease. It bifurcated into a larger tibial nerve medially nerveand a smaller common peroneal nerve laterally (Figures 1,2).
Figure 1: Photograph of dissection of the right gluteal region & back of the thigh showing high bifurcation (arrow) of the right sciatic nerve (SN) by 1 cm below the lower border of piriformis muscle (PM). The nerve is divided into tibial nerve (TN) and common peroneal nerve (CPN). (QF: quadratus femoris muscle; IG: inferior gemellus muscle)
Figure 2: Photograph of dissection of the left gluteal region & back of the thigh showing high bifurcation (arrow) of the left sciatic nerve (SN) by 2 cm below the lower border of piriformis muscle (PM). The nerve is divided into tibial nerve (TN) and common peroneal nerve (CPN). (QF: quadratus femoris muscle; SG: superior gemellus muscle; IG: inferior gemellus muscle)
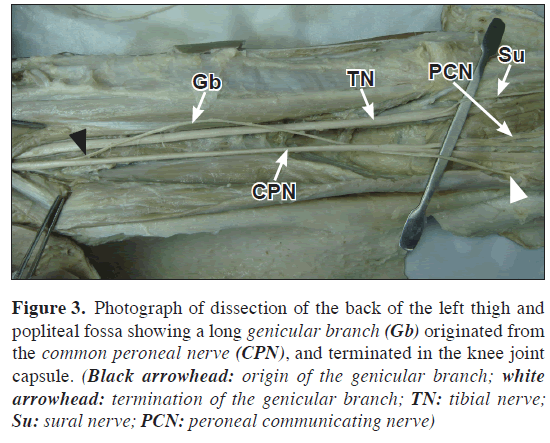
In the same case on the left side, an interesting finding was observed in the common peroneal nerve. A long slender branch emerged from the medial aspect of the nerve in the middle part of the thigh (20 cm from the site of bifurcation of sciatic nerve). This variant branch ran downwards and laterally along the common peroneal nerve. It ended into the capsule of the knee joint, so it could be considered as one of the genicular branches of the common peroneal nerve (Figure 3).
Figure 3: Photograph of dissection of the back of the left thigh and popliteal fossa showing a long genicular branch (Gb) originated from the common peroneal nerve (CPN), and terminated in the knee joint capsule. (Black arrowhead: origin of the genicular branch; white arrowhead: termination of the genicular branch; TN: tibial nerve; Su: sural nerve; PCN: peroneal communicating nerve)
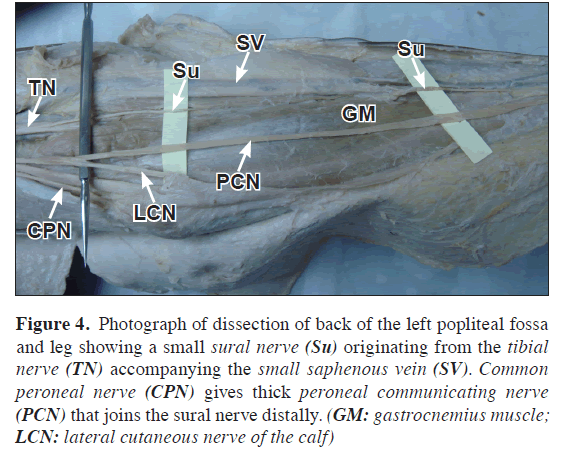
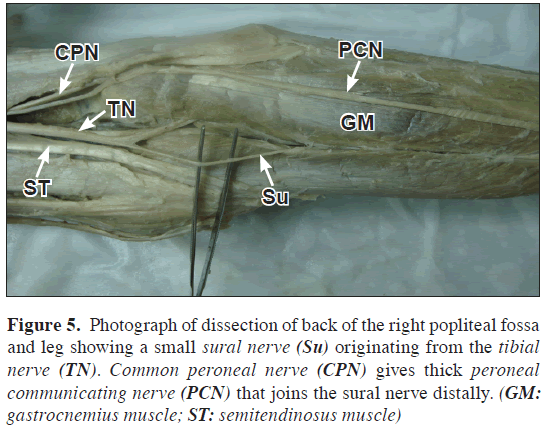
The sural nerves had a normal course bilaterally but of very small size. The peroneal communicating nerve, which is a branch of the common peroneal nerve, was bilaterally thick and carried most of the nerve fibers distributed to the areas supplied normally by the sural nerve. The peroneal communicating nerve coursed down the lateral side of the leg and joined the small sural nerve above the lateral malleolus (Figures 4,5).
Figure 4: Photograph of dissection of back of the left popliteal fossa and leg showing a small sural nerve (Su) originating from the tibial nerve (TN) accompanying the small saphenous vein (SV). Common peroneal nerve (CPN) gives thick peroneal communicating nerve (PCN) that joins the sural nerve distally. (GM: gastrocnemius muscle; LCN: lateral cutaneous nerve of the calf)
Figure 5: Photograph of dissection of back of the right popliteal fossa and leg showing a small sural nerve (Su) originating from the tibial nerve (TN). Common peroneal nerve (CPN) gives thick peroneal communicating nerve (PCN) that joins the sural nerve distally. (GM: gastrocnemius muscle; ST: semitendinosus muscle)
Discussion
A number of variations in the course and distribution of the sciatic nerve (SN) have been reported [2]. Higher level of the SN division is a relatively frequent phenomenon. Bifurcation into its two major divisions (common peroneal and tibial nerves) may occur anywhere between the sacral plexus and the lower part of the thigh [3]. In the present case, the right SN was divided 1 cm below the lower border of the piriformis muscle, while the left was divided 2 cm below lower border of the piriformis muscle on both sides above the gemellus superior. The high bifurcation of this nerve is of clinical importance. The piriformis syndrome occurs secondary to the compression of the SN as it exits the greater sciatic foramen in the gluteal region [4]. The anatomical variations in the level at which the sciatic nerve divides into the tibial nerve and common peroneal nerve have been suspected as a possible cause for incomplete block of the sciatic nerve in the popliteal fossa [1].
The common peroneal nerve (CPN), usually gives off three genicular (articular) branches. In our present case, a long variant genicular branch on the medial aspect of CPN in the middle of the left thigh was noticed during routine dissection. Its clinical significance in knee surgery may be very much appreciated.
The peroneal nerve is the most common site of intraneural ganglia and the communication proved to extend through the articular branch of the CPN. It arises from the superior tibiofibular joint and are connected to it by the articular branch [5]. The CPN is most frequently damaged as a result of complete or partial division during varicose vein operations and in cases of complication of small saphenous vein surgery [6,7].
Classically, the sural nerve (Su) is formed by the joining of the medial sural cutaneous nerve (MSCN) and the peroneal communicating nerve (PCN) or by the MSCN or PCN alone [8]. There had been some debate on the contribution of the Su. In a significant study, it is reported that the contribution of the PCN (or LSCN) was greater than that of the MSCN [9]. The bilateral thick peroneal communicating nerves in our present case were directly continuing from the common peroneal nerves. They were supplying those areas normally covered by sural nerve. In addition to this, it is also noted that the sural nerves here were quite thin and joining with the above-mentioned thick peroneal communicating nerves distally in the legs on both sides. In the case of nerve grafts and tissue biopsies, the proper selection of the size and the site is critical. The Su is the most frequent site of the nerve graft and peripheral nerve biopsy [8]. However, sacrificing the Su causes clinical problems. In order to reduce such problems, it is reported that the PCN (or LSCN) can be a good substitute for the Su [10].
Acknowledgements
The authors greatly acknowledge the contribution of Mr. Shaik Rahiman, Lecturer of Biochemistry, College of Medicine, Al-Jouf University for his help in overall outcome of the manuscript.
References
- Nayak S. An unusual case of trifurcation of the sciatic nerve. Neuroanatomy. 2006; 5: 6–7.
- Huelke DF. The origin of the peroneal communicating nerve in adult man. Anat Rec. 1958; 132: 81–92.
- Mas N, Ozeksi P, Ozdemir B, Kapakin S, Mustafa F, Sargon H, Celik H, Yener N. A case of bilateral high division of the sciatic nerves, together with a unilateral unusual course of the tibial nerve. Neuroanatomy. 2003; 2: 13–15.
- Porta M. A comparative trial of botulinum toxin type A and methylprednisolone for the treatment of myofascial pain syndrome and pain from chronic muscle spasm. Pain. 2000; 85: 101–105.
- Spinner RJ, Atkinson JL, Tiel RL. Peroneal intraneural ganglia: the importance of the articular branch. A unifying theory. J Neurosurg. 2003; 99: 330–343.
- Giannas J, Bayat A, Watson SJ. Common peroneal nerve injury during varicose vein operation. Eur J Vasc Endovasc Surg. 2006 ; 31: 443–445.
- Atkin GK, Round T, Vattipally VR, Das SK. Common peroneal nerve injury as a complication of short saphenous vein surgery. Phlebology. 2007; 22: 3–7.
- Strauch B, Goldberg N, Herman CK. Sural nerve harvest: anatomy and technique. J Reconstr Microsurg. 2005; 21: 133–136.
- Kim CH, Jung HY, Kim MO, Lee CJ. The relative contributions of the medial sural and peroneal communicating nerves to the sural nerve. Yonsei Med J. 2006; 47: 415–422.
- Ortiguela ME, Wood MB, Cahill DR. Anatomy of the sural nerve complex. J Hand Surg Am. 1987; 12: 1119–1123.
Md Hassan Ali and Mohamed Hassan Eweidah*
Department of Anatomy, College of Medicine, Al-Jouf University, Sakaka, Al-Jouf Kingdom of Saudi Arabia.
- *Corresponding Author:
- Mohamed Hassan Eweidah
Associate Professor of Anatomy, College of Medicine, Al-Jouf University, PO Box 2014, Sakaka Al-Jouf,Saudi Arabia.
Tel: +966 555875425
E-mail: eweidah@yahoo.com
Date of Received : December 14th, 2009
Date of Accepted : February 23rd, 2010
Published Online : February 28th, 2010
© IJAV. 2010; 3: 33–35.
Abstract
In addition to identifying a pectoralis quartus muscle variation, an additional variation of the anterior thoracic wall that has not been reported in the literature was found in a 60-year-old male cadaver. The accessory muscle originated from the aponeurosis of the external abdominal oblique and inserted on the fascia overlying the coracobrachialis muscle. Additionally, the co-existence of an accessory muscle and pectoralis quartus has not been previously described. The current findings and the clinical significance are discussed as a single muscle variation and as two muscle variations in combination.
-Keywords
sciatic nerve,genicular branch,sural nerve,common peroneal nerve,nerve transplantation
Introduction
Sciatic nerve, the largest branch of the sacral plexus originates from the L4-S3 roots, emerges from the greater sciatic foramen and passes inferior to the piriformis muscle between the ischial tuberosity and the greater trochanter of the femur. The nerve divides most frequently at the level of the upper angle of the popliteal fossa into tibial and common peroneal branches [1]. Both the tibial and the common peroneal nerves give muscular, cutaneous and genicular branches. The medial sural cutaneous nerve from tibial nerve or peroneal communicating nerve from common peroneal nerve may continue as sural nerve which supplies the lateral surface of the leg, gives off the lateral branches to the heel and the lateral dorsal cutaneous nerve [2].
We here present a case of bilateral high division of the sciatic nerves together with a unilateral (left) unusual high genicular branch of the common peroneal nerve and bilateral unusual thick peroneal communicating nerves.
Case Report
Case Report
During the routine dissection for medical undergraduates in the College of Medicine, Al-Jouf University, Kingdom of Saudi Arabia, a bilateral high bifurcation of the sciatic nerves in a 50-year-old male Filipino cadaver was noticed. The sciatic nerve terminated 2 cm (on the left side) and 1 cm (on the right side) below the lower border of the piriformis muscle, about 41 cm from the popliteal skin crease. It bifurcated into a larger tibial nerve medially nerveand a smaller common peroneal nerve laterally (Figures 1,2).
Figure 1: Photograph of dissection of the right gluteal region & back of the thigh showing high bifurcation (arrow) of the right sciatic nerve (SN) by 1 cm below the lower border of piriformis muscle (PM). The nerve is divided into tibial nerve (TN) and common peroneal nerve (CPN). (QF: quadratus femoris muscle; IG: inferior gemellus muscle)
Figure 2: Photograph of dissection of the left gluteal region & back of the thigh showing high bifurcation (arrow) of the left sciatic nerve (SN) by 2 cm below the lower border of piriformis muscle (PM). The nerve is divided into tibial nerve (TN) and common peroneal nerve (CPN). (QF: quadratus femoris muscle; SG: superior gemellus muscle; IG: inferior gemellus muscle)
In the same case on the left side, an interesting finding was observed in the common peroneal nerve. A long slender branch emerged from the medial aspect of the nerve in the middle part of the thigh (20 cm from the site of bifurcation of sciatic nerve). This variant branch ran downwards and laterally along the common peroneal nerve. It ended into the capsule of the knee joint, so it could be considered as one of the genicular branches of the common peroneal nerve (Figure 3).
Figure 3: Photograph of dissection of the back of the left thigh and popliteal fossa showing a long genicular branch (Gb) originated from the common peroneal nerve (CPN), and terminated in the knee joint capsule. (Black arrowhead: origin of the genicular branch; white arrowhead: termination of the genicular branch; TN: tibial nerve; Su: sural nerve; PCN: peroneal communicating nerve)
The sural nerves had a normal course bilaterally but of very small size. The peroneal communicating nerve, which is a branch of the common peroneal nerve, was bilaterally thick and carried most of the nerve fibers distributed to the areas supplied normally by the sural nerve. The peroneal communicating nerve coursed down the lateral side of the leg and joined the small sural nerve above the lateral malleolus (Figures 4,5).
Figure 4: Photograph of dissection of back of the left popliteal fossa and leg showing a small sural nerve (Su) originating from the tibial nerve (TN) accompanying the small saphenous vein (SV). Common peroneal nerve (CPN) gives thick peroneal communicating nerve (PCN) that joins the sural nerve distally. (GM: gastrocnemius muscle; LCN: lateral cutaneous nerve of the calf)
Figure 5: Photograph of dissection of back of the right popliteal fossa and leg showing a small sural nerve (Su) originating from the tibial nerve (TN). Common peroneal nerve (CPN) gives thick peroneal communicating nerve (PCN) that joins the sural nerve distally. (GM: gastrocnemius muscle; ST: semitendinosus muscle)
Discussion
A number of variations in the course and distribution of the sciatic nerve (SN) have been reported [2]. Higher level of the SN division is a relatively frequent phenomenon. Bifurcation into its two major divisions (common peroneal and tibial nerves) may occur anywhere between the sacral plexus and the lower part of the thigh [3]. In the present case, the right SN was divided 1 cm below the lower border of the piriformis muscle, while the left was divided 2 cm below lower border of the piriformis muscle on both sides above the gemellus superior. The high bifurcation of this nerve is of clinical importance. The piriformis syndrome occurs secondary to the compression of the SN as it exits the greater sciatic foramen in the gluteal region [4]. The anatomical variations in the level at which the sciatic nerve divides into the tibial nerve and common peroneal nerve have been suspected as a possible cause for incomplete block of the sciatic nerve in the popliteal fossa [1].
The common peroneal nerve (CPN), usually gives off three genicular (articular) branches. In our present case, a long variant genicular branch on the medial aspect of CPN in the middle of the left thigh was noticed during routine dissection. Its clinical significance in knee surgery may be very much appreciated.
The peroneal nerve is the most common site of intraneural ganglia and the communication proved to extend through the articular branch of the CPN. It arises from the superior tibiofibular joint and are connected to it by the articular branch [5]. The CPN is most frequently damaged as a result of complete or partial division during varicose vein operations and in cases of complication of small saphenous vein surgery [6,7].
Classically, the sural nerve (Su) is formed by the joining of the medial sural cutaneous nerve (MSCN) and the peroneal communicating nerve (PCN) or by the MSCN or PCN alone [8]. There had been some debate on the contribution of the Su. In a significant study, it is reported that the contribution of the PCN (or LSCN) was greater than that of the MSCN [9]. The bilateral thick peroneal communicating nerves in our present case were directly continuing from the common peroneal nerves. They were supplying those areas normally covered by sural nerve. In addition to this, it is also noted that the sural nerves here were quite thin and joining with the above-mentioned thick peroneal communicating nerves distally in the legs on both sides. In the case of nerve grafts and tissue biopsies, the proper selection of the size and the site is critical. The Su is the most frequent site of the nerve graft and peripheral nerve biopsy [8]. However, sacrificing the Su causes clinical problems. In order to reduce such problems, it is reported that the PCN (or LSCN) can be a good substitute for the Su [10].
Acknowledgements
The authors greatly acknowledge the contribution of Mr. Shaik Rahiman, Lecturer of Biochemistry, College of Medicine, Al-Jouf University for his help in overall outcome of the manuscript.
References
- Nayak S. An unusual case of trifurcation of the sciatic nerve. Neuroanatomy. 2006; 5: 6–7.
- Huelke DF. The origin of the peroneal communicating nerve in adult man. Anat Rec. 1958; 132: 81–92.
- Mas N, Ozeksi P, Ozdemir B, Kapakin S, Mustafa F, Sargon H, Celik H, Yener N. A case of bilateral high division of the sciatic nerves, together with a unilateral unusual course of the tibial nerve. Neuroanatomy. 2003; 2: 13–15.
- Porta M. A comparative trial of botulinum toxin type A and methylprednisolone for the treatment of myofascial pain syndrome and pain from chronic muscle spasm. Pain. 2000; 85: 101–105.
- Spinner RJ, Atkinson JL, Tiel RL. Peroneal intraneural ganglia: the importance of the articular branch. A unifying theory. J Neurosurg. 2003; 99: 330–343.
- Giannas J, Bayat A, Watson SJ. Common peroneal nerve injury during varicose vein operation. Eur J Vasc Endovasc Surg. 2006 ; 31: 443–445.
- Atkin GK, Round T, Vattipally VR, Das SK. Common peroneal nerve injury as a complication of short saphenous vein surgery. Phlebology. 2007; 22: 3–7.
- Strauch B, Goldberg N, Herman CK. Sural nerve harvest: anatomy and technique. J Reconstr Microsurg. 2005; 21: 133–136.
- Kim CH, Jung HY, Kim MO, Lee CJ. The relative contributions of the medial sural and peroneal communicating nerves to the sural nerve. Yonsei Med J. 2006; 47: 415–422.
- Ortiguela ME, Wood MB, Cahill DR. Anatomy of the sural nerve complex. J Hand Surg Am. 1987; 12: 1119–1123.