Anatomical Variations of the Recurrent Laryngeal Nerve and Implications for Injury Prevention During Surgical Procedures of the Neck
2 Department of Anatomy, Michigan Head & Spine Institute, Southfield, MI, United States, Email: danielfahim@gmail.com
3 Department of Foundational Medical Studies, Oakland University William Beaumont School of Medicine, MI, United States
Received: 17-Mar-2020 Accepted Date: Jul 29, 2020; Published: 05-Aug-2020
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Introduction: Injury of the recurrent laryngeal nerve (RLN) during surgical procedures of the neck may result in vocal cord paralysis which leads to dysphonia and dysphagia. Accurate knowledge of anatomical variations of RLN provides information to prevent inadvertent intraoperative injury, improving patient safety, optimizing clinical outcomes, and ultimately guiding best clinical and surgical practices. The present study aims to assess the potential anatomical variability of RLN pertaining to its course, branching pattern, and relationship to the inferior thyroid artery, which potentially makes it vulnerable to injury, compression, or stretch during surgical procedures of the neck.
Materials and Methods: 55 formalin-fixed cadavers were carefully dissected and examined, with the course of recurrent laryngeal nerve carefully evaluated and documented bilaterally. Cadavers with anatomical variation were photographed and the data was analyzed quantitatively.
Results: Our findings indicate that extra laryngeal branches coming off of the RLN on both the right and left side innervate the esophagus, trachea, and mainly intrinsic laryngeal muscles. On the right side, 89.1% of the cadavers demonstrated 2-5 extra laryngeal branches. On the left side, 74.6% of the cadavers demonstrated 2-3 extra-laryngeal branches. In relation to the inferior thyroid artery (ITA), 67.9% of right RLNs were located anteriorly, while 32.1% were located posteriorly. On the other hand, 32.1% of left RLNs were anterior to the ITA, while 67.9% were related posteriorly. On both sides 3-5% of RLN crossed in between the branches of the ITA.
Concluding remarks: Anatomical consideration of the variations in the course, branching pattern, and relationship of the RLNs is essential to minimize complications associated with surgical procedures of the neck, especially thyroidectomy and anterior cervical discectomy and fusion (ACDF) surgery. The information gained in this study emphasizes the need to preferentially utilize left-sided approaches for ACDF surgery whenever possible
Keywords
Recurrent laryngeal nerve; Inferior thyroid artery, Anatomical variations; ACDF; Thyroidectomy
Materials and Methods
The study was performed on 55 formalin-fixed cadavers at Oakland University William Beaumont School of Medicine from 2017-2019, of which 28 were male, 27 were female, and all were Caucasian in ethnicity. Anterior cervical deep dissection was performed in order to locate the RLN and surrounding landmarks on each cadaver. Cadavers that demonstrated anatomical variations were identified, and after detailed clearing, photographs were taken for data analysis. Cadavers without anatomical variations were also photographed for comparison as controls. The data was documented based on whether the left or right nerve was being observed, and also based on the number of branches that were identified on each RLN. We also took into account the relationship of the RLN with the ITA, whether the nerve was anterior, posterior, or in between the branches of the artery. The data was analyzed quantitatively with the McNemar’s Test and Fisher’s Exact Test, and statistical significance was determined based on a p value less than 0.05.
Results
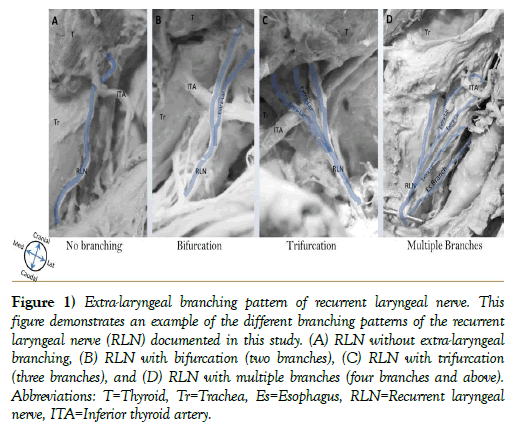
The findings indicated that there are branches coming off of the RLN on both the right and left sides, innervating both the esophagus and trachea in some instances. On the right side, 89.1% demonstrated anywhere between 2-5 extra-laryngeal branches, and 74.6% demonstrated branching on the left side (Table 1) (Figure 1). Using the Fisher’s Exact Test, and following data analysis, it was determined that there is a statistically significant difference in the branching pattern between the two sides. Of note, 16.4% of the cadavers demonstrated concomitant bilateral bifurcations in this study, while16.4% of the cadavers demonstrated concomitant bilateral trifurcations.
TABLE 1
Frequency distribution of recurrent laryngeal nerve branching pattern. This table demonstrates the frequency distribution of branching patterns of the recurrent laryngeal nerve (RLN) on the right and left side. The right RLN branching pattern is documented to be anywhere between 2-5 branches (89.1%), while the left RLN documented to be 2-5 branches (74.6%). The values were statistically significant, as determined by P<0.05 (McNemar’s Test and Fisher’s Exact Test, P=0.0348).
| Right Side | Left Side | |||
|---|---|---|---|---|
| Frequency | % | Frequency | % | |
| Branches | 89.09 | 74.55 | ||
| Bifurcation (2) | 22 | 40.00 | 15 | 27.27 |
| Trifurcation (3) | 15 | 27.27 | 19 | 34.55 |
| Multiple (≥ 4) | 12 | 21.82 | 7 | 12.73 |
| No branch | 6 | 10.91 | 14 | 24.45 |
Figure 1: Extra-laryngeal branching pattern of recurrent laryngeal nerve. This figure demonstrates an example of the different branching patterns of the recurrent laryngeal nerve (RLN) documented in this study. (A) RLN without extra-laryngeal branching, (B) RLN with bifurcation (two branches), (C) RLN with trifurcation (three branches), and (D) RLN with multiple branches (four branches and above). Abbreviations: T=Thyroid, Tr=Trachea, Es=Esophagus, RLN=Recurrent laryngeal nerve, ITA=Inferior thyroid artery.
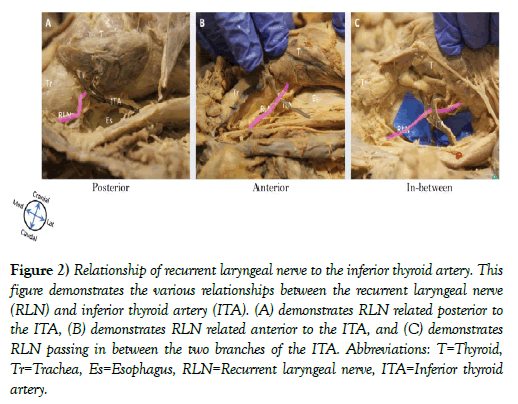
The relationship of the RLN with the ITA was also examined. The ITA is a common landmark that surgeons use to locate the RLN especially during thyroidectomy. The RLN was discovered to have a varying relationship with ITA, and can be seen anterior or posterior to it, and even sometimes in between the branches of ITA. In relation to the ITA, 67.9% of right RLN’s were related anteriorly, while 32.1% were related posteriorly. The opposite values were true for the left side, with 67.9% related posteriorly and 32.1% related anteriorly. On the right side, 3.6% of nerves crossed in between branches of ITA, while 5.4% of left RLN’s were found crossing between branches of ITA (Table 2) (Figure 2).
TABLE 2
Frequency of relationship of recurrent laryngeal nerve to the inferior thyroid artery. This table demonstrates the relationship of recurrent laryngeal nerve (RLN) to the inferior thyroid artery (ITA) on the right and left side. RLN is observed as either related anteriorly, posteriorly, or in between the ITA. The right RLN demonstrated 67.9% anterior to the ITA, and 32.1% posterior to it. The left RLN demonstrated the exact opposite results with 32.1% anterior, and 67.9% posterior to the ITA. The08 values were statistically significant, as determined by P<0.05 (McNemar’s Test and Fisher’s Exact Test, P=0.0004).
| Right Side | Left Side | |||
|---|---|---|---|---|
| Frequency | % | Frequency | % | |
| Anterior | 36 | 67.92 | 17 | 32.08 |
| Posterior | 17 | 32.08 | 36 | 67.92 |
| In-between | 2 | 3.57 | 3 | 5.36 |
Figure 2: Relationship of recurrent laryngeal nerve to the inferior thyroid artery. This figure demonstrates the various relationships between the recurrent laryngeal nerve (RLN) and inferior thyroid artery (ITA). (A) demonstrates RLN related posterior to the ITA, (B) demonstrates RLN related anterior to the ITA, and (C) demonstrates RLN passing in between the two branches of the ITA. Abbreviations: T=Thyroid, Tr=Trachea, Es=Esophagus, RLN=Recurrent laryngeal nerve, ITA=Inferior thyroid artery.
Discussion
Injury of the RLN is a well-known and troublesome complication associated with surgical procedures of the neck. Awareness of anatomical variation in the branching patterns of the RLN contributes to the challenge of avoiding this complication. Consideration of these variations is essential to minimize complications associated with surgical procedures of the neck- especially in ACDF and thyroidectomies. Significant post-operative complications, such as airway obstruction and narrowing, can be avoided if surgeons and their assistants in the operating room are aware of these variant structures. Ignorance of the anatomical variations in the branching pattern of the RLN makes it vulnerable to damage by stretching, compression, retraction, or accidental sharp division during the aforementioned surgical procedures.
Although a number of studies debate whether the left or right-sided approach to surgery is safer, there is no generally accepted consensus in the surgical community. To answer this question our study focused on side variations observed and found that the left RLN branches less often than the right RLN, and also takes a more predictable course to the laryngeal structures, rather than an oblique, anterolateral approach. Chen and his colleagues describe that overstretching of the RLN is less likely to occur on the left side due to the fact that it is better protected within the tracheoesophageal groove [11]. The right sided approach is typically taken during an ACDF procedure, due to surgeon handedness [11]. The other reason why neurosurgeons in particular favor right-sided approach is due to awareness of the risk of causing compression of the carotid artery during retraction or the inadvertent dislodging of athreoscloretic plaque during dissection, resulting in stroke. A right-sided stroke is far better tolerated than a left-sided stroke due to language dominance in the overwhelming majority of patients.
In contrast to thyroidectomy, in ACDF the RLN is not routinely monitored or exposed as standard practice, potentially making it more prone to damage from indirect intraoperative injury by retraction or stretch injury while separating fascial layers or during retraction [12]. Of course, the counter argument is that avoiding exposure of the nerve makes it less vulnerable to injury as no dissection is being carried out immediately around it. Direct surgical trauma to the RLN is rare, which is why injury is typically related to overstretching or excessive pressure from the endotracheal tube [13].
Our findings indicate that there is a significant amount of variation in the RLN’s course and branching pattern, indicating that 89% of right RLN and 74.6% of left RLN demonstrated 2-5 extra-laryngeal branches. These findings are in agreement with previous studies that have reported significant variability in RLN branching patterns [14-17]. This data suggests that the risk of iatrogenic injury is greater with right-sided approaches than the left-sided approaches during ACDF procedures. The right RLN has more variability in its branching pattern, relationship with the ITA, and by its anterolateral position in comparison with the left [16,17]. Because of the fact that extra-laryngeal branching patterns are so common, misidentification of these branches can potentially lead to iatrogenic injury [16]. It is argued that branched nerves are even more vulnerable than those without branches because of their smaller caliber and fragility, ultimately making them prone to damage even with normal manipulation [12]. Similar to our study, previous finding reported that 50% to 60% patients often have small branches of the RLN that innervate trachea, esophagus, or inferior constrictor muscles, and misidentification of these branches can cause a myriad of post-operative symptoms that include dysphagia, dyspnea, and dysphonia [16]. The greater number of branches on the right suggests that the risk of iatrogenic injury is greater with right-sided approach than with the left-sided approach during ACDF procedures.
In addition to the greater number of branches, the relationship of the right RLN to the ITA may potentially make it more vulnerable to injury as well [16,17] Campos and Henriques described a typical relationship between the RLN and ITA, where the RLN passes posterior to the nerve [17]. Our findings discredit the idea that the RLN consistently passes posterior to the ITA. Therefore, this idea of the RLN consistently passing posterior to the ITA might not be always true because it can give surgeons a false sense of security when dissecting anterior to ITA, ultimately leading to an increased risk of damage [13]. Our study supported with other studies provide evidence demonstrating that the right RLN more often passes anterior to the ITA approximately two-thirds of the time, while the inverse is true on the left [18]. Therefore, left sided approaches to ACDF procedures may be safer as the ITA can more often be identified before the branches of RLN are encountered.
In meta-anaylsis study regarding anatomic variations of the RLN, a significant difference was noted in the prevalence of extra-laryngeal branch patterns between cadaveric studies, and intraoperative studies, 73.3% and 39.2% respectively [17]. The authors suggested that observing branching of the RLN is underestimated in the operating room, and this is attributed to the difficulty of viewing branches intraoperatively due to localized inflammation and edema that can be encountered in anterior neck dissections [19]. True prevalence of extra-laryngeal branching was determined to be better reflected in cadaveric studies, prompting surgeons to attempt to expose the RLN and any branches in their entirety, unless it puts the patient at risk for a more invasive procedure [17].
Vocal cord paralysis is one of the most significant morbidities after ACDF procedures, with incidence up to 24.2% immediately post-operatively [20]. Identification and localization of RLN and intraoperative neuromonitoring of clinically relevant anatomical variations has to be encouraged. Henry and others described that pre-operative ultrasound was used to identify structures and anatomical variations successfully [17]. decrease the risk of iatrogenic injury to the RLN [18]. Of course, this practice would be timeconsuming and potentially cost prohibitive if undertaken for each patient prior to ACDF surgery. We recommend the use of ultrasound evaluation or intraoperative monitoring if a patient has had previous neck surgery. Alternatively, the patient may be direct laryngoscopy pre-operatively to evaluate for unilateral silent vocal cord paralysis. This population of patients may have clinically silent unilateral RLN injuries and are at higher risk for a potentially devastating injury if the opposite side is injured in a subsequent procedure of the neck.
In general, the information gained from our study emphasizes the need of special considerations during ACDF and thyroidectomies, including side preferences, in order to preserve the extra-laryngeal branches of the RLN. Parameters that could potentially affect the incidence of branching patterns that must be looked into further include variations in surgical exposure techniques, retraction practices, the use of surgical loops or magnification, and the use of intraoperative neuromonitoring [18]. The majority of previous studies performed assessing the RLN’s anatomical variations and landmark structures described only one aspect of the nerve and considered smaller sample sizes. Our study tried to address this drawback by considering a comprehensive anatomical approach to show the larger perspective of RLN and its relationship with the surrounding structures using a large sample size of cadavers. One of the limitations of this study is all the cadavers assessed were Caucasian in ethnicity and this might affect the generalizability of our findings.
Conclusion
In conclusion, this study may have implications for surgical technique and consideration of the side of approach for preserving the extra-laryngeal branches of the RLN during surgical procedures of the neck such as ACDF and thyroidectomy procedures. In general, we would recommend preferentially utilizing the left sided approach for ACDF and being mindful of the proximity of the RLN branches to the ITA. Of course, the side of the surgical approach is multifactorial and the individualized decision must be made by the surgeon.
Acknowledgement
The Authors would like to acknowledge Mary Bee from University of Detroit Mercy Lab and the OUWB Embark program staff for their unreserved support.
Abbreviations
RLN – recurrent laryngeal nerve; ITA – Inferior thyroid artery; ACDF – Anterior cervical discectomy and fusion; CN X – Vagus Nerve
Disclosure
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
REFERENCES
- Shao T, Qiu W, Yang W. Anatomical variations of the recurrent laryngeal nerve in Chinese patients: A prospective study of 2,404 patients. Sci Rep. 2016;6:25475.
- Kulekci M, Batıoglu-Karaaltın A, Saatci O, et al. Relationship between the Branches of the Recurrent Laryngeal Nerve and the Inferior Thyroid Artery. Ann Otol Rhinol Laryngol. 2012;121:650-6.
- Haller JM, Iwanik M, Shen FH. Clinically relevant anatomy of recurrent laryngeal nerve. Spine. 2012;37:97-100.
- Dankbaar JW, Pameijer FA. Vocal cord paralysis: anatomy, imaging and pathology. Insights Imaging. 2014;5:743-51.
- Miscusi M, Bellitti A, Peschillo S, et al. Does recurrent laryngeal nerve anatomy condition the choice of the side for approaching the anterior cervical spine?. Eura Medicophys. 2007:80-5.
- Kilburg C, Sullivan HG, Mathiason MA. Effect of approach side during anterior cervical discectomy and fusion on the incidence of recurrent laryngeal nerve injury. J Neurosurg Spine. 2006;4:273-7.
- Cernea CR, Hojaij FVC, De Carlucci D, et al. Recurrent laryngeal nerve: A plexus rather than a nerve? Arch Otolaryngol - Head Neck Surg. 2009;135:1098-1102.
- Jung A, Schramm J. How to reduce recurrent laryngeal nerve palsy in anterior cervical spine surgery: A prospective observational study. Neurosurg. 2010;67:10-15.
- Liu SC, Chou YF, Su WF. A rapid and Accurate Technique for the Identification of the Recurrent Laryngeal Nerve. Ann Otol Rhinol Laryngol. 2014;123.
- Melamed H, Harris MB, Awasthi D. Anatomic Considerations of Superior Laryngeal Nerve During Anterior Cervical Spine Procedures. Spine (Phila Pa 1976). 2003;27:E83-6.
- Jung A, Schramm J. How to reduce recurrent laryngeal nerve palsy in anterior cervical spine surgery: A prospective observational study. Neurosurg. 2010;67:10-15.
- Rihn JA, Kane J, Albert TJ, et al. What is the incidence and severity of dysphagia after anterior cervical surgery?. Clin Orthop Relat Res. 2011;469:658-65.
- Henry BM, Vikse J, Graves MJ, et al. Extralaryngeal branching of the recurrent laryngeal nerve: a meta-analysis of 28,387 nerves. Langenbeck’s Arch Surg. 2016;401:913-23.
- Gurleyik E. Surgical anatomy of bilateral extralaryngeal bifurcation of the recurrent laryngeal nerve: Similarities and differences between both sides. N Am J Med Sci. 2014;6:445-49.
- Casella C, Pata G, Nascimbeni R, et al. Does extralaryngeal branching have an impact on the rate of postoperative transient or permanent recurrent laryngeal nerve palsy?. World J Surg. 2009;33:261.
- Uludag M, Yazici P, Aygun N, et al. A Closer Look at the Recurrent Laryngeal Nerve Focusing on Branches & Diameters: A Prospective Cohort Study. J Investig Surg. 2016;29:1-6.
- Campos BA, Henriques PRF. Relationship between the recurrent laryngeal nerve and the inferior thyroid artery: a study in corpses. Rev Hosp Clin Fac Med Sao Paulo. 2005;55:195-200.
- Asgharpour E, Maranillo E, Sañudo J, et al. Recurrent laryngeal nerve landmarks revisited. Head Neck. 2012;34:1240-6.
- Chen CC, Huang YC, Lee ST, et al. Long-term result of vocal cord paralysis after anterior cervical disectomy. Eur Spine J. 2014;23:622-26.
- Tan TP, Govindarajulu AP, Massicotte EM, et al. Vocal cord palsy after anterior cervical spine surgery: A qualitative systematic review. Spine J. 2014;14:124.