Bilateral superficial ulnar arteries with an unusual arterial arch in the forearmthe
Nachiket Shankar* and Raveendranath Veeramani
Department of Anatomy, St. John’s Medical College, Bangalore, Karnataka, India
- *Corresponding Author:
- Nachiket Shankar, MS
Assistant Professor, Department of Anatomy, St. John’s Medical College Sarjapur Road, Bangalore Karnataka, 560034, India
Tel: +91 80 22065061/62
Fax: +91 80 25520777
E-mail: nachiket76@gmail.com
Date of Received: November 4th, 2008
Date of Accepted: January 31st, 2009
Published Online: February 2nd, 2009
© Int J Anat Var (IJAV). 2009; 2: 24–26.
[ft_below_content] =>Keywords
superficial ulnar artery, origin, brachial artery, axillary artery, arterial arch
Introduction
The ulnar artery is the larger terminal branch of the brachial artery and is usually given off in the cubital fossa. Along with the radial artery, it supplies the structures in the forearm and hand, as well as the elbow and wrist joints. The superficial ulnar artery (SUA) is a rare variation of the ulnar artery. It usually arises higher up, either in the axilla or the arm, and runs a superficial course in the forearm before entering the hand [1]. In this case report we describe the bilateral presence of SUA along with an unusual arterial arch in the forearm. It’s embryological basis, incidence, course, branches, associations, and clinical importance are discussed.
Case Report
During routine dissection of an elderly male cadaver, an unusual branch was seen arising from the brachial artery on the left side and from the axillary artery on the right side. These arteries were traced from origin to termination and their course, relations and branches were studied. On tracing these arteries, they were identified as SUA on either side.
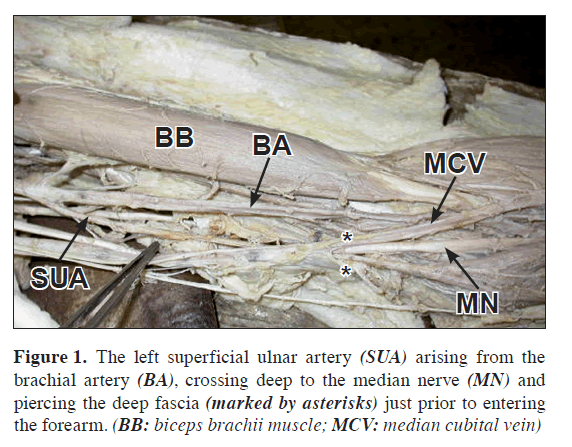
On the left side, the SUA arose from the junction of the upper and middle one third of the brachial artery (Figure 1). It coursed medial to the brachial artery and was crossed superficially by the median nerve from the lateral to the medial side. Just proximal to entering the forearm the SUA pierced the brachial fascia. Subsequently it ran a subcutaneous course along the medial aspect of forearmthe forearm. Before entering the hand it bore a similar relationship as a normal ulnar artery to the flexor carpi ulnaris and the ulnar nerve. It then entered the palm, superficial to the flexor retinaculum and formed the superficial palmar arch. The SUA gave the superior and inferior ulnar collateral arteries (SUCA and IUCA) in the arm. No other significant branches were given off by the SUA. On this side, the brachial artery was terminated in the cubital fossa by giving off the radial and the common interosseous arteries.
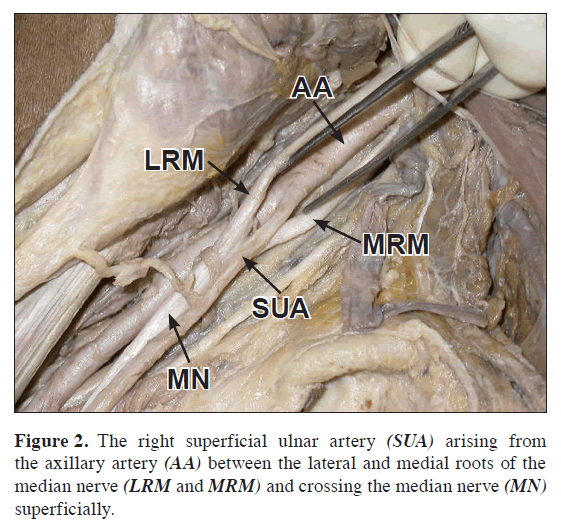
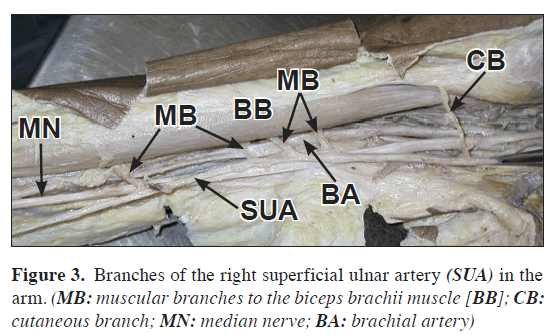
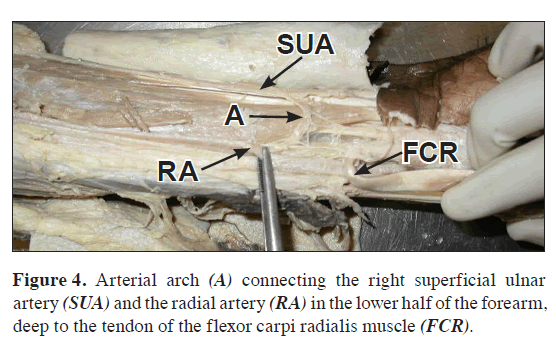
On the right side, the SUA arose from the 3rd part of the axillary artery just proximal to the joining of the medial and lateral roots of the median nerve (Figure 2). The caliber of the SUA was larger on this side. It then coursed superficial to both the median nerve and the brachial artery, but deep to the deep fascia. Its further course in the forearm and hand was similar to that on the left side. However, the branches arising from the SUA on this side were different. Just after the origin, it gave a large cutaneous branch to the skin of the upper medial aspect of the arm. It then gave four large muscular branches to the biceps brachii muscle (Figure 3). In the lower half of the forearm, an arterial arch connecting the SUA and radial artery was observed deep to the tendon of the flexor carpi radialis muscle (Figure 4). The termination of the brachial artery was similar to that on the left side. The palmaris longus was found to be absent on this side.
Discussion
Anomalies of the arterial system of the upper limb are not uncommon, as its development is dependent upon multiple sources as well as a precise sequential pattern of formation and regression. These anomalies may be of various types such as variations in the mode of origin or branching pattern, occupation of unusual tissue planes and unexpected relationships to surrounding structures [2]. The older sprouting theory was initially proposed by Singer in 1933 and was widely accepted till recently [3]. Poteat proposed modifications of this theory in 1986 [4,5]. He stated that there is an axis artery of the upper limb which initially consists of vessels that persist in adult life as the axillary artery, brachial artery, anterior interosseous artery and the deep palmar arch. All other arteries are formed as branches of this axis artery. The final arterial pattern in adults is formed as a result of branching, anastomosis and selective regression [2].
However, recent evidence from human embryos in various stages of development does not support the sprouting theory. Initially a capillary plexus originating from the dorsal aorta develops in the limb bud. Extensive remodeling of this capillary plexus in a proximo-distal direction occurs. The adult pattern of blood vessels occurs due selective maintenance, enlargement and differentiation of certain channels and regression of others. Variations in the arterial pattern of the upper limb occur due to persistence and enlargement of parts of the capillary plexus that would otherwise have regressed [6]. The precise reason for the formation of the SUA is not known; although genetic predisposition, chemical factors, hemodynamic forces, fetal limb movement and unusual musculature may all play a role [1,7].
The overall incidence of the SUA varies between 0.67 and 9.38%, as reported in various studies conducted throughout the world [1]. It more commonly arises from the brachial artery as compared to the axillary artery [8]. The reported incidence of the SUA arising from the axillary artery varies between 0.17% and 2% [1]. The bilateral presence of the SUA with a different origin on each side is even more rare [9]. When the SUA is present, the brachial artery commonly terminates as the radial and common interosseous artery as seen in the present case [8]. In the present case, the SUA arose from the junction of the upper and middle third of the brachial artery on the left side. The SUA arises most frequently from the lower third of the brachial artery, less frequently from the upper third and rarely from the middle third [8]. The termination of the SUA on either side by forming the superficial palmar arch as observed by us is the usual mode of termination [1,7,8,9].
The relations of the SUA to the median nerve differed on either side in the present case. On the left side the SUA passed deep to the median nerve and on the right side it was superficial. The SUA most often crosses superficial to the median nerve [1,8,9]. To our knowledge, passage of the SUA deep to the median nerve is extremely uncommon. In this case, the SUA ran in the subcutaneous plane in the forearm on both sides. The plane of the SUA in the forearm has been variably described as being subfascial or subcutaneous. The subfascial course appears to be more common [8].
In the present case, the SUA on the left side gave off the SUCA and the IUCA. On the right side, it gave a large cutaneous branch to the skin of the arm and four substantial branches to the biceps brachii muscle. In the lower half of the forearm an arterial arch connecting the SUA and the radial artery was observed on the right side. When present, the SUA often gives branches to the biceps brachii [1,9-11]. To our knowledge, the other described branches rarely arise from the SUA. A survey of the literature showed that an arterial arch connecting the SUA and the radial artery in the forearm has not been reported previously.
The SUA is sometimes associated with the absence of the palmaris longus muscle, as we observed on the right side [5]. Other associated arterial anomalies, like a persistent median artery may be present along with a SUA [1,8,12]. These were not observed in our case. The presence of a SUA has important clinical implications. The superficial course of the SUA places it at risk during trauma and intravenous cannulation. Inadvertent intra-arterial passage of drugs during intravenous injections may occur, with grave consequences. Reconstructive surgeries using flaps are becoming increasingly common. Free forearm flaps based on the radial artery may damage the SUA causing ischemia of the hand. Also the presence of a SUA may cause difficulties in the interpretation of angiograms. Thus, it is important to look for a possible SUA before performing the procedures mentioned above. This can be accomplished by careful palpation of the cubital fossa and ulnar aspect of the forearm, or by Doppler ultrasound examination. The SUA, if recognized preoperatively, can be used to advantage in raising a skin flap for reconstructive surgeries [1,5,7,13,14].
Acknowledgements
The authors would like to thank Dr. Roopa Ravindranath, Professor, Department of Anatomy, as well as all the other staff of the Anatomy Department at St. John’s Medical College for their support and encouragement.
References
- Natsis K, Papadopoulou AL, Paraskevas G, Totlis T, Tsikaras P. High origin of a superficial ulnar artery arising from the axillary artery: anatomy, embryology, clinical significance and a review of the literature. Folia Morphol. 2006; 65: 400–405.
- Standring S, ed. Gray’s Anatomy. 39th Ed., Elsevier Churchill Livingstone Publishers. 2006; 941.
- Singer E. Embryological pattern persisting in the arteries of the arm. Anat Rec. 1933; 55: 403–409.
- Poteat WL. Report of a rare human variation: absence of the radial artery. Anat Rec. 1986; 214: 89–95.
- Nakatani T, Tanaka S, Mizukami S. Superficial ulnar artery originating from the brachial artery and its clinical importance. Surg Radiol Anat. 1998; 20: 383–385.
- Rodriguez-Niedenfuhr M, Vazquez T, Parkin IG, Sanudo JR. Arterial patterns of the human upper limb: update of anatomical variations and and embryological development. Eur J Anat. 2003; 7 Suppl. 1: 21–28.
- Krishnamurthy A, Kumar M, Nayak SR, Prabhu LV. High origin and superficial course of ulnar artery: a case report. Firat Tip Dergisi. 2006; 11: 66–67.
- Rodriguez-Niedenfuhr M, Vazquez T, Nearn L, Ferreira B, Parkin I, Sanudo JR. Variations of the arterial pattern in the upper limb revisited: a morphological and statistical study, with a review of the literature. J Anat. 2001; 199: 547–566.
- Yazar F, Kirici Y, Ozan H, Aldur MM. An unusual variation of the superficial ulnar artery. Surg Radiol Anat. 1999; 21: 155–157.
- Jacquemin G, Lemaire V, Medot M, Fissette J. Bilateral case of superficial ulnar artery originating from axillary artery. Surg Radiol Anat. 2001; 23: 139–143.
- Aharinejad S, Nourani F, Hollensteiner H. Rare case of high origin of the ulnar artery from the brachial artery. Clin Anat. 1997; 10: 253–258.
- Rodriguez-Baeza A, Nebot J, Ferreira B, Reina F, Perez J, Sanudo JR, Roig M. An anatomical study and ontogenic explanation of 23 cases with variations in the main pattern of the human brachio-antebrachial arteries. J Anat. 1995; 187: 473–479.
- Hazlett JW. The superficial ulnar artery with reference to accidental intra-arterial injection. Can Med Assoc J. 1949; 61: 289–293.
- Devansh. Superficial ulnar artery flap. Plast Reconstr Surg. 1996; 97: 420–426.
Nachiket Shankar* and Raveendranath Veeramani
Department of Anatomy, St. John’s Medical College, Bangalore, Karnataka, India
- *Corresponding Author:
- Nachiket Shankar, MS
Assistant Professor, Department of Anatomy, St. John’s Medical College Sarjapur Road, Bangalore Karnataka, 560034, India
Tel: +91 80 22065061/62
Fax: +91 80 25520777
E-mail: nachiket76@gmail.com
Date of Received: November 4th, 2008
Date of Accepted: January 31st, 2009
Published Online: February 2nd, 2009
© Int J Anat Var (IJAV). 2009; 2: 24–26.
Abstract
The superficial ulnar artery is a rare variant of the ulnar artery. It usually arises higher up, either in the axilla or the arm, and runs a superficial course in the forearm before entering the hand. During routine dissection of an elderly male cadaver, superficial ulnar arteries were seen bilaterally. On the left side, the artery arose from the junction of the upper and middle one third of the brachial artery. It arose from the 3rd part of the axillary artery on the right side. On this side, an arterial arch connecting the superficial ulnar artery and radial artery was observed in the forearm. Bilaterally, the brachial artery terminated in the cubital fossa by giving off the radial and the common interosseous arteries. An arterial arch connecting the superficial ulnar artery and the radial artery in the forearm has not been reported previously. The presence of a superficial ulnar artery has important clinical implications.
-Keywords
superficial ulnar artery, origin, brachial artery, axillary artery, arterial arch
Introduction
The ulnar artery is the larger terminal branch of the brachial artery and is usually given off in the cubital fossa. Along with the radial artery, it supplies the structures in the forearm and hand, as well as the elbow and wrist joints. The superficial ulnar artery (SUA) is a rare variation of the ulnar artery. It usually arises higher up, either in the axilla or the arm, and runs a superficial course in the forearm before entering the hand [1]. In this case report we describe the bilateral presence of SUA along with an unusual arterial arch in the forearm. It’s embryological basis, incidence, course, branches, associations, and clinical importance are discussed.
Case Report
During routine dissection of an elderly male cadaver, an unusual branch was seen arising from the brachial artery on the left side and from the axillary artery on the right side. These arteries were traced from origin to termination and their course, relations and branches were studied. On tracing these arteries, they were identified as SUA on either side.
On the left side, the SUA arose from the junction of the upper and middle one third of the brachial artery (Figure 1). It coursed medial to the brachial artery and was crossed superficially by the median nerve from the lateral to the medial side. Just proximal to entering the forearm the SUA pierced the brachial fascia. Subsequently it ran a subcutaneous course along the medial aspect of forearmthe forearm. Before entering the hand it bore a similar relationship as a normal ulnar artery to the flexor carpi ulnaris and the ulnar nerve. It then entered the palm, superficial to the flexor retinaculum and formed the superficial palmar arch. The SUA gave the superior and inferior ulnar collateral arteries (SUCA and IUCA) in the arm. No other significant branches were given off by the SUA. On this side, the brachial artery was terminated in the cubital fossa by giving off the radial and the common interosseous arteries.
On the right side, the SUA arose from the 3rd part of the axillary artery just proximal to the joining of the medial and lateral roots of the median nerve (Figure 2). The caliber of the SUA was larger on this side. It then coursed superficial to both the median nerve and the brachial artery, but deep to the deep fascia. Its further course in the forearm and hand was similar to that on the left side. However, the branches arising from the SUA on this side were different. Just after the origin, it gave a large cutaneous branch to the skin of the upper medial aspect of the arm. It then gave four large muscular branches to the biceps brachii muscle (Figure 3). In the lower half of the forearm, an arterial arch connecting the SUA and radial artery was observed deep to the tendon of the flexor carpi radialis muscle (Figure 4). The termination of the brachial artery was similar to that on the left side. The palmaris longus was found to be absent on this side.
Discussion
Anomalies of the arterial system of the upper limb are not uncommon, as its development is dependent upon multiple sources as well as a precise sequential pattern of formation and regression. These anomalies may be of various types such as variations in the mode of origin or branching pattern, occupation of unusual tissue planes and unexpected relationships to surrounding structures [2]. The older sprouting theory was initially proposed by Singer in 1933 and was widely accepted till recently [3]. Poteat proposed modifications of this theory in 1986 [4,5]. He stated that there is an axis artery of the upper limb which initially consists of vessels that persist in adult life as the axillary artery, brachial artery, anterior interosseous artery and the deep palmar arch. All other arteries are formed as branches of this axis artery. The final arterial pattern in adults is formed as a result of branching, anastomosis and selective regression [2].
However, recent evidence from human embryos in various stages of development does not support the sprouting theory. Initially a capillary plexus originating from the dorsal aorta develops in the limb bud. Extensive remodeling of this capillary plexus in a proximo-distal direction occurs. The adult pattern of blood vessels occurs due selective maintenance, enlargement and differentiation of certain channels and regression of others. Variations in the arterial pattern of the upper limb occur due to persistence and enlargement of parts of the capillary plexus that would otherwise have regressed [6]. The precise reason for the formation of the SUA is not known; although genetic predisposition, chemical factors, hemodynamic forces, fetal limb movement and unusual musculature may all play a role [1,7].
The overall incidence of the SUA varies between 0.67 and 9.38%, as reported in various studies conducted throughout the world [1]. It more commonly arises from the brachial artery as compared to the axillary artery [8]. The reported incidence of the SUA arising from the axillary artery varies between 0.17% and 2% [1]. The bilateral presence of the SUA with a different origin on each side is even more rare [9]. When the SUA is present, the brachial artery commonly terminates as the radial and common interosseous artery as seen in the present case [8]. In the present case, the SUA arose from the junction of the upper and middle third of the brachial artery on the left side. The SUA arises most frequently from the lower third of the brachial artery, less frequently from the upper third and rarely from the middle third [8]. The termination of the SUA on either side by forming the superficial palmar arch as observed by us is the usual mode of termination [1,7,8,9].
The relations of the SUA to the median nerve differed on either side in the present case. On the left side the SUA passed deep to the median nerve and on the right side it was superficial. The SUA most often crosses superficial to the median nerve [1,8,9]. To our knowledge, passage of the SUA deep to the median nerve is extremely uncommon. In this case, the SUA ran in the subcutaneous plane in the forearm on both sides. The plane of the SUA in the forearm has been variably described as being subfascial or subcutaneous. The subfascial course appears to be more common [8].
In the present case, the SUA on the left side gave off the SUCA and the IUCA. On the right side, it gave a large cutaneous branch to the skin of the arm and four substantial branches to the biceps brachii muscle. In the lower half of the forearm an arterial arch connecting the SUA and the radial artery was observed on the right side. When present, the SUA often gives branches to the biceps brachii [1,9-11]. To our knowledge, the other described branches rarely arise from the SUA. A survey of the literature showed that an arterial arch connecting the SUA and the radial artery in the forearm has not been reported previously.
The SUA is sometimes associated with the absence of the palmaris longus muscle, as we observed on the right side [5]. Other associated arterial anomalies, like a persistent median artery may be present along with a SUA [1,8,12]. These were not observed in our case. The presence of a SUA has important clinical implications. The superficial course of the SUA places it at risk during trauma and intravenous cannulation. Inadvertent intra-arterial passage of drugs during intravenous injections may occur, with grave consequences. Reconstructive surgeries using flaps are becoming increasingly common. Free forearm flaps based on the radial artery may damage the SUA causing ischemia of the hand. Also the presence of a SUA may cause difficulties in the interpretation of angiograms. Thus, it is important to look for a possible SUA before performing the procedures mentioned above. This can be accomplished by careful palpation of the cubital fossa and ulnar aspect of the forearm, or by Doppler ultrasound examination. The SUA, if recognized preoperatively, can be used to advantage in raising a skin flap for reconstructive surgeries [1,5,7,13,14].
Acknowledgements
The authors would like to thank Dr. Roopa Ravindranath, Professor, Department of Anatomy, as well as all the other staff of the Anatomy Department at St. John’s Medical College for their support and encouragement.
References
- Natsis K, Papadopoulou AL, Paraskevas G, Totlis T, Tsikaras P. High origin of a superficial ulnar artery arising from the axillary artery: anatomy, embryology, clinical significance and a review of the literature. Folia Morphol. 2006; 65: 400–405.
- Standring S, ed. Gray’s Anatomy. 39th Ed., Elsevier Churchill Livingstone Publishers. 2006; 941.
- Singer E. Embryological pattern persisting in the arteries of the arm. Anat Rec. 1933; 55: 403–409.
- Poteat WL. Report of a rare human variation: absence of the radial artery. Anat Rec. 1986; 214: 89–95.
- Nakatani T, Tanaka S, Mizukami S. Superficial ulnar artery originating from the brachial artery and its clinical importance. Surg Radiol Anat. 1998; 20: 383–385.
- Rodriguez-Niedenfuhr M, Vazquez T, Parkin IG, Sanudo JR. Arterial patterns of the human upper limb: update of anatomical variations and and embryological development. Eur J Anat. 2003; 7 Suppl. 1: 21–28.
- Krishnamurthy A, Kumar M, Nayak SR, Prabhu LV. High origin and superficial course of ulnar artery: a case report. Firat Tip Dergisi. 2006; 11: 66–67.
- Rodriguez-Niedenfuhr M, Vazquez T, Nearn L, Ferreira B, Parkin I, Sanudo JR. Variations of the arterial pattern in the upper limb revisited: a morphological and statistical study, with a review of the literature. J Anat. 2001; 199: 547–566.
- Yazar F, Kirici Y, Ozan H, Aldur MM. An unusual variation of the superficial ulnar artery. Surg Radiol Anat. 1999; 21: 155–157.
- Jacquemin G, Lemaire V, Medot M, Fissette J. Bilateral case of superficial ulnar artery originating from axillary artery. Surg Radiol Anat. 2001; 23: 139–143.
- Aharinejad S, Nourani F, Hollensteiner H. Rare case of high origin of the ulnar artery from the brachial artery. Clin Anat. 1997; 10: 253–258.
- Rodriguez-Baeza A, Nebot J, Ferreira B, Reina F, Perez J, Sanudo JR, Roig M. An anatomical study and ontogenic explanation of 23 cases with variations in the main pattern of the human brachio-antebrachial arteries. J Anat. 1995; 187: 473–479.
- Hazlett JW. The superficial ulnar artery with reference to accidental intra-arterial injection. Can Med Assoc J. 1949; 61: 289–293.
- Devansh. Superficial ulnar artery flap. Plast Reconstr Surg. 1996; 97: 420–426.