Brief introduction to corneal stromal cell
Received: 10-Dec-2021 Accepted Date: Dec 27, 2021; Published: 03-Jan-2022
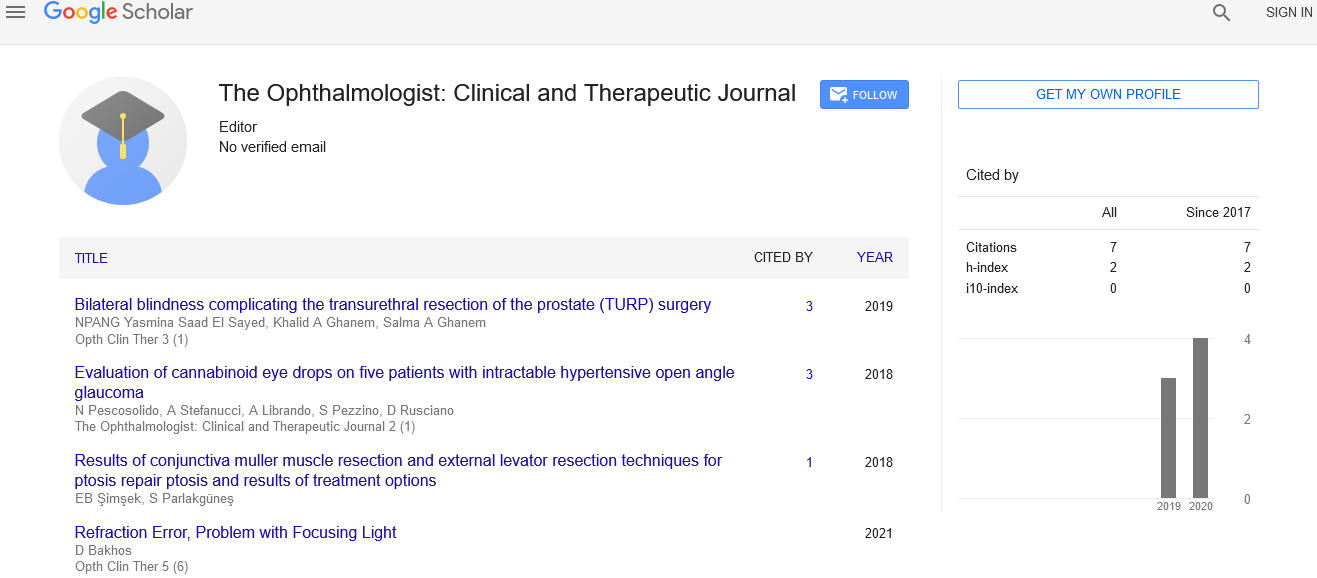
Citation: Connon J. Brief introduction to corneal stromal cell. Opth Clin Ther. 2022;5(6):5
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Editorial Note
Corneal keratocytes (corneal fibroblasts) are specialised fibroblasts residing within the stroma. The corneal layer, representing concerning 85-90% of tissue thickness, is constructed up from extremely regular collagenous lamellae and extracellular matrix elements. Keratocytes, also called as fibroblasts, are mesenchyme-derived cells of the corneal stroma. These cells are commonly quiescent; however they are fast in responding and transition into repair phenotypes following injury. Cytokines and different growth factors that offer autocrine signals for stimulating wound responses in resident cells are generally conferred by platelets at the positioning of an injury. Corneal scarring is related to activate keratocytes responding to a pathological atmosphere, and their conversion to myofibroblasts that deposit non-transparent fibrotic tissue. HiPSCderived NCCs adopt corneal keratocyte-like when cultured in three dimensions or seeded onto cadaveric corneal tissue. Keratocytes play the most important role keep it clear, healing its wounds, and synthesizing its elements. In the unperturbed tissue keratocytes stay dormant, coming into action when any serious injury or inflammation occurs. Some keratocytes underlying the positioning of injury, even a lightweight one, endure programmed cell death instantly after the injury. One in all the primary noticeable changes within the tissue layer stroma following injury and death of a population of keratocytes. This primary keratocyte cell death could be a benign response, thought to own evolved so as to shield the cornea from additional inflammation, and subsequent loss of transparency. Laser in situ keratomileusis (LASIK) could be a newer corrective procedure, within which a flap of the epithelium and basement membrane is initially peeled back by a microkeratome and laser ablation is later on performed on the underlying stroma. In LASIK, keratocyte death is found to occur deeper within the stroma and is typically restricted to the anterior and posterior lamellar face created by the microkeratome. Any fault within the exactly orchestrated process of healing could blur the tissue layer, whereas excessive keratocyte apoptosis could also be a section of the pathological process within the corneal layer disorders like astigmia, and these concerns prompt the continuing analysis into the operation of those cells. Upon injury to the hepatocytes will transition into divergent phenotypes that are enthusiastic about specific environmental signals. Since keratocytes originate from a population of cranial neural crest cells, it is been postulated that a number of the regenerative properties exhibited by these cells following wounding could also be attributed to their stem cellular properties, that were preserved from their cell of origin. Keratocan and Lumican are vital keratan sulphate-containing proteoglycans that are extremely expressed in corneal layer keratocytes. Keratocytes are developmentally derived from the bone population of neural crest cells, from where from they migrate to settle within the mesenchyme. In some species the migration from neural crest comes in two waves, with the primary organic process to create the corneal layer endothelium and also the second invading the epithelium-secreted stromal organ innocent of cells; in different species each populations return from one wave of migration. Once settled within the stroma, keratocytes begin synthesizing albuminoid molecules of various varieties (I, V, VI) and keratan sulphate. These keratocytes are derived from neural crest cells (NCCs). Throughout embryogenesis, NCCs occupy the presumptive tissue layer at around E10.5 in mice and later on differentiate into keratocytes, inflicting thickening of the stroma. By the instant of eye opening when birth, the proliferation of keratocytes is just about finished and most of them are within the quiescent state. By the end of eye development an interconnected keratocyte network is established within the cornea, with dendrites of neighbour cells contacting one another. Quiescent keratocytes synthesize the crystalline, known primarily for his or her role within the lens. Corneal crystallins, just like the lens type, are thought to assist maintaining the transparency and best refraction. These are additionally a part of corneal antioxidant defense. Protein extracts of keratocytes isolated from clear rabbit corneas showed marked reductions in the expression of these proteins. Keratocytes are quiescent, mesenchymal-like cells that extend out keratopodia that contact neighbor keratocytes, forming a incessantly joined cell population at intervals the stroma. Apoptosis of keratocytes, either in quiescent or active state, could be a method that draws special attention. One hypothesis explains such fast reaction by the requirement to stem the doable infection from spreading into the tissue layer, as a result the restrictions of ocular system is the done by immune cells that take up too many hours to hit the position of injury. In an exceedingly traditional course of events, the dearth of keratocytes is bit by bit replenished by the mitosis of the adjacent cells. Programmed cell death is determined when keratotomy, as well as surgery, and many will play a job within the development of post-surgery complications. Keratocytes could play a job in numerous tissue layer disorders. According to comparative research, their functions drastically diverge from the norm in keratoconus, the foremost sort of corneal dystrophy. In keratoconic corneas they need been shown to commit programmed cell death isolated from any epithelial injury; a hypothesis exists that presents excessive keratocyte programmed cell death as a serious pathological event in keratoconus.