Compliance with recommendations for routine HIV screening during pregnancy in Halifax
- *Corresponding Author:
- Dr Scott A Halperin
IWK Health Centre, 5850 University Avenue, Halifax, Nova Scotia B3J 3G9.
Tel:902-470-8141
Fax:902-470-7232
E-mail:shalperin@iwkgrace.ns.ca
Keywords
Counselling; HIV; Perinatal transmission; Pregnancy; Screening
The majority of paediatric AIDS cases in Canada can be attributed to vertical transmission (mother to fetus) of HIV [1]. Treatment of an HIV-positive pregnant woman with zidovudine (ZDV) before and during birth, as well as treatment of the child after birth, can reduce the rate of vertical transmission by approximately two-thirds [2]. In 1995, 70.2% of AIDS cases among Canadian women of child-bearing age were in women who became infected with HIV through heterosexual contact or who did not have any identifiable risk factors [3]. According to this statistic, if only those women who were classified as being atrisk were counselled about HIV and HIV testing, a large proportion of women who are HIV-positive would not be identified. Furthermore, studies have shown that women with higher levels of education and women who received proper HIV counselling had higher rates of consent for HIV screening and ZDV intervention [4].
The Society of Obstetricians and Gynaecologists of Canada (SOGC) [5], the Canadian Medical Association [6], the College of Family Physicians of Canada [7], the Canadian Paediatric Society [8], the Canadian Paediatric AIDS Research Group [9] and the Reproductive Care Program (RCP) of Nova Scotia [3] recommend that all pregnant women be counselled about HIV and HIV testing, and be offered an HIV blood test during their pregnancy. Both the Departments of Obstetrics/Gynecology and Family Medicine at the IWK Health Centre, Halifax, Nova Scotia follow the SOGC and RCP guidelines.
The primary objective of this study was to determine the proportion of women in Nova Scotia who delivered at the IWK Health Centre who were counselled about HIV and HIV testing during pregnancy. A secondary objective was to determine the proportion of those who had received counselling who subsequently underwent the blood test.
Methods
Setting and study population
The study was conducted at the IWK Health Centre where, in 2000, there were 4625 deliveries (50% of all deliveries in Nova Scotia). All pregnant women who delivered at the IWK Health Centre between March 10 and May 10, 2000 were given a questionnaire to complete. The study was approved by the IWK Health Centre Research Ethics Board.
Procedures
A letter of introduction and a questionnaire were attached to the front of the packages for those with newborns that nurses distributed to mothers after delivery. The nurses were asked to mention the questionnaire to the women. The principal investigator met with the nursing staff before the study began to raise awareness about the importance of HIV screening, and nurses were reminded of their role throughout the two months. Completed questionnaires were placed in a sealed box at the nursing station. The return rate one month into the study averaged less than 20%; therefore, return envelopes were attached to the questionnaires to allow women the option of completing the questionnaire after they left the hospital.
Instrument
The questionnaire asked women for their ages, levels of education and histories of previous deliveries. They were also asked if they received counselling about HIV during their pregnancy and, if yes, who spoke to them and at what point in time. Furthermore, they were asked if they were offered an HIV blood test, whether they had an HIV blood test done and, if so, when it was performed. Finally, those who did not have an HIV blood test were asked for their reasons for not doing so. The demographics of the total population of women who delivered at the IWK Health Centre during the same time period were assessed and compared with the sample population.
Statistical considerations
Sample sizes of 400 and 200 were calculated to provide a point estimate with a 95% CI width of 10% for the primary objective and 15% for the secondary objective. With a predicted compliance rate of 50% for the return of the questionnaire, the survey was scheduled to continue for two months, which would have allowed the distribution of surveys to approximately 800 women.
The frequency distribution of all variables was calculated. Comparison of proportional data were analyzed with χ2 or Fisher’s exact test as appropriate to determine the significance of the association of each predictor variable with the two outcome variables.
Results
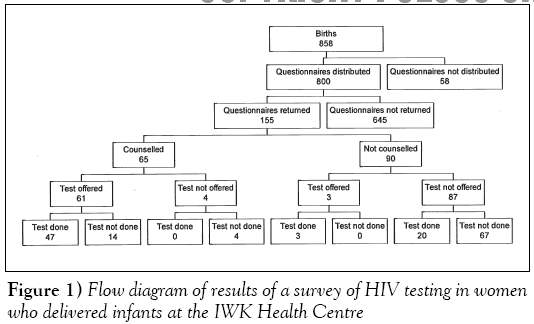
There were 858 births at the IWK Health Centre between March 10 and May 10, 2000. Letters were distributed to 800 new mothers and 155 questionnaires were returned (response rate of 19.4%) (Figure 1). The mean age of respondents was 29.7 years and more than 61% of those had completed postsecondary education or held an advanced degree (Table 1). A total of 65 (41.9%; 95% CI 34.1 to 49.7) women were counselled about HIV during their pregnancy and 47 (72.3%; 95% CI 65.3 to 79.3) of those who were counselled underwent the test.
| Patient characteristics | Mean | Respondents Range |
|---|---|---|
| Age (years) | 29.7 | 17–45 |
| Previous deliveries | 0.7 | 0–5 |
| Education | Total | Proportion (%) |
| Some high school | 7 | 4.5 |
| Completed high school | 18 | 11.6 |
| Some postsecondary | 35 | 22.6 |
| Completed postsecondary | 79 | 51.0 |
| Advanced degree | 16 | 10.3 |
Table 1: Patient characteristics among respondents to a questionnaire distributed between May 10 and March 10, 2000 for women who delivered at the IWK Health Centre
There were significant differences between: the proportion of women counselled and whether the current delivery was their first delivery or if they had previous deliveries (P=0.050); the proportion of women offered a test and their ages (P=0.028); and the proportion of women who underwent a test and their ages (P=0.017) (Table 2). There were no significant differences between: the proportion of women counselled about HIV and their ages and levels of education; the proportion of women offered an HIV blood test and their levels of education and histories of previous deliveries; and the proportion of women who had an HIV blood test and their levels of education and histories of previous deliveries.
| Variables | Younger than 25 | Age (years) 25 or older | P | Level of education | |||||
|---|---|---|---|---|---|---|---|---|---|
| High school or less | Postsecondary | P | Previous deliveries | ||||||
| Yes | No | P | |||||||
| Number counselled (%) | 12 (7.7) | 53 (34.2) | 0.093 | 12 (7.7) | 53 (34.2) | 0.52 | 37 (23.9) | 28 (18.1) | 0.050 |
| Number not counselled (%) | 8 (5.2) | 82 (52.9) | 13 (8.4) | 77 (49.7) | 36 (23.2) | 54 (34.8) | |||
| Test offered (%) | 13 (8.4) | 51 (32.9) | 0.028 | 13 (8.4) | 51 (32.9) | 0.27 | 36 (23.2) | 37 (23.9) | 0.072 |
| Test not offered (%) | 7 (4.5) | 84 (54.2) | 12 (7.7) | 79 (51.0) | 28 (18.1) | 54 (34.8) | |||
| Test done (%) | 14 (9.0) | 55 (35.5) | 0.017 | 13 (8.4) | 56 (36.1) | 0.51 | 38 (24.5) | 31 (20.0) | 0.078 |
| Test not done (%) | 6 (3.9) | 80 (51.6) | 12 (7.7) | 74 (47.7) | 35 (22.6) | 51 (32.9) | |||
Table 2: Hypothesized predictor variables associated with HIV counselling and screening of women who delivered at the IWK Health Centre in Nova Scotia
The proportion of women who were offered an HIV blood test was 64 of 155 (41.3%); 14 of those women chose not to have the test done (Figure 1). An additional 20 women requested and underwent the test without it being offered; therefore, the total number of women who had an HIV test was 70 of 155 (45.2%).
Women were counselled by their family doctor (n=50, 76.9%), an obstetrician (n=16, 24.6%), a nurse (n=8, 12.3%), an obstetrical resident (n=3, 4.6%) or another health care worker (n=1, 1.5%). Counselling was done predominantly during the first trimester of their pregnancies (n=60, 92.3%), followed by the second trimester (n=8, 12.3%) and the third trimester (n=2, 3.1%). No women were counselled at the time of or after delivery. The women who underwent an HIV blood test during their pregnancy did so during the first trimester (n=54, 77.1%), followed by the second trimester (n=14, 20.0%) and the third trimester (n=2, 2.9%). No women were tested at the time of or after delivery.
Women who did not have an HIV blood test were asked for their reasons for not doing so. Reasons given included: not at risk (n=20), not offered (n=23), not sure if test was done (n=7), in a monogamous relationship (n=13), not a concern (n=10), tested recently (n=13), uncomfortable asking for one myself (n=1), no time to do it (n=1), automatically done in another province (n=2) and do not know (n=4).
The age and the number of previous deliveries of the women who completed the questionnaire (age – mean 29.7±5.1 years, range 17 to 45 years; previous deliveries – mean 0.8±0.9, range 0 to 5) were similar to those of all women who delivered at the IWK Health Centre during the same time period (age – mean 29.7±5.2 years, range 15 to 49 years; previous deliveries – mean 0.8±0.9, range 0 to 5).
Discussion
This study demonstrates that a substantial number of pregnant women were neither counselled about HIV during their pregnancy nor offered an HIV blood test. However, of those women who were counselled about HIV, most had an HIV blood test done. These results confirm previous studies that found that when women are counselled and offered an HIV blood test, they are more likely to have a blood test done [4]. The results also indicate that in Nova Scotia, family doctors, obstetricians and nurses may be involved in the counselling process and that those who are involved are following the guidelines outlined by the Reproductive Care Program of Nova Scotia. These guidelines state that:
women should be counseled about HIV and offered an HIV blood test during the first trimester of their pregnancy. However, if not completed by the second and third trimesters, counseling and testing should be done at these times. [3]
Although many women did not receive testing because they did not perceive themselves to be at risk, some women indicated that they were not offered a blood test. It is possible that if they had been offered an HIV test, they may have considered having it done. A history of previous births was a predictor that the proportion of women counselled and an age below 25 years was associated with higher rates of counselling and higher rates of women who had the HIV test done. Also of concern is that many women did not know whether they were tested for HIV during the series of routine prenatal tests. If they had been counselled about HIV, they would have known that HIV is not included in the routine prenatal tests, but can be done at the same time if requested.
The major limitation of this study was the smaller than anticipated response rate, which may have introduced bias. Different response rates may be related to level of education, culture, duration of stay in hospital, parity and inconsistent reminders by nursing staff. There are no demographic data on the nonresponders except that the age and previous deliveries of the women who completed the questionnaire were similar to those of all women who delivered at the IWK Health Centre during the same time period. We hypothesize that the reason for the poor return rate was that the questionnaire was distributed to the women at a very busy and exciting time, when they had a lot of other paperwork to complete. However, a sensitivity analysis indicated that if all 645 women who did not respond actually had been counselled, the proportion of women counselled would have been 710 of 800 (88.8%). In contrast, if all 645 women who did not respond had not been counselled , the proportion of women counselled would have been only 65 of 800 (8.1%). Some medical authorities suggest that HIV counselling programs during pregnancy should target a minimum standard of 90% to 95% of women. Therefore, both the survey’s results (41.9%) and the hypothetical extremes (8.1% to 88.8%) are unacceptably low.
These results indicate that all health care professionals involved in the care of pregnant women need to be reminded of the importance of HIV counselling and testing during pregnancy. If education cannot improve the proportion of women who are counselled and offered an HIV blood test during their pregnancy, then policies may need to be changed. New policies could include mandating HIV counselling by all professionals involved in obstetrics, or mandating HIV testing of all pregnant women in Nova Scotia. However, these types of options are not commonly seen in clinical medicine. The most favourable options may be additional education of both health care providers (rounds, in-services) and the public (prenatal classes, educational brochures in hospital and physician waiting rooms), and systems modifications such as check-off boxes on prenatal and labour and delivery forms. Whatever interventions are implemented, follow-up audits are necessary to evaluate whether the current standards are being met.
Acknowledgements
We thank the nurses of the Maternal and Newborn Health Program of the IWK Health Centre for their assistance with the study survey.
References
- Health Canada. HIV/AIDS Epi Update: Perinatal Transmission of HIV. May 2001. <www.hc-sc.gc.ca/hpb/lcdc/bah/epi/peri_e.html>. (Version current at August 1, 2001)
- Connor EM, Sperling RS, Gleber R, et al. Reduction of maternal-infant transmission of human immunodeficiency virus type 1 with zidovudine treatment. N Engl J Med 1994;331:1173-80.
- Reproductive Care Program of Nova Scotia. Guidelines for antenatal laboratory screening and testing and HIV counseling guidelines. Halifax: Reproductive Care Program of Nova Scotia, 1998.
- Oldenettel D, Dye T, Artal R. Prenatal HIV screening in pregnant women; a medical-legal review. Birth 1997;24:165-72.
- Society of Obstetricians and Gynaecologists of Canada (SOGC) Clinical Practice Guidelines. HIV Testing in Pregnancy. June 1997;62.
- Canadian Medical Association. Counselling Guidelines for HIV testing. Ottawa: Canadian Medical Association; 1995.
- Tessier D, Dion H, Grossman DW, Rachlis A. HIV Care: A Primer &
- Canadian Paediatric Society. Statement: Perinatal human immunodeficiency virus (HIV) testing. Can J Paediatr 1994;1:ID94-01.
- Samson L, King S. Evidence-based guidelines for universal counselling and offering of HIV testing in pregnancy in Canada. CMAJ 1998;158:1449-57.
- *Corresponding Author:
- Dr Scott A Halperin
IWK Health Centre, 5850 University Avenue, Halifax, Nova Scotia B3J 3G9.
Tel:902-470-8141
Fax:902-470-7232
E-mail:shalperin@iwkgrace.ns.ca
Abstract
BACKGROUND: The routine offering of testing for HIV during each pregnancy is recommended by various advisory bodies, including the Canadian Paediatric Society. OBJECTIVES: To determine the proportion of women in Nova Scotia who were counselled about HIV and HIV testing during their pregnancies and to determine the proportion of those who underwent the blood test after counselling. METHODS: A Self-administered survey at the IWK Health Centre, Halifax, Nova Scotia was performed. Questionnaires were distributed to 800 new mothers who delivered a child between March 10 and May 10, 2000. The questionnaire asked women for their ages, levels of education, history of previous deliveries, whether they had received counselling about HIV during their pregnancy, whether they were offered an HIV blood test and whether they underwent an HIV blood test. RESULTS: A total of 155 questionnaires were returned (response rate of 19.4%). The proportion of women who were counselled about HIV during their pregnancy was 65 of 155 (41.9%) (95% CI 34.1 to 49.7) and the proportion of those who were counselled who underwent the test was 47 of 65 (72.3%) (95% CI 65.3 to 79.3). There was a significant difference between the proportion counselled and history of previous deliveries (P=0.050), the proportion offered a test and their ages (P=0.028), and the proportion who had a test done and their ages (P=0.017). CONCLUSIONS: There is inadequate compliance with the recommendation that all women be offered HIV testing during each pregnancy at the IWK Health Centre. Health care professionals involved in obstetrics need to be reminded of the importance of HIV counselling and testing during pregnancy. Further evaluation throughout Canada of the effect of HIV screening recommendations during pregnancy is advisable.
-Keywords
Counselling; HIV; Perinatal transmission; Pregnancy; Screening
The majority of paediatric AIDS cases in Canada can be attributed to vertical transmission (mother to fetus) of HIV [1]. Treatment of an HIV-positive pregnant woman with zidovudine (ZDV) before and during birth, as well as treatment of the child after birth, can reduce the rate of vertical transmission by approximately two-thirds [2]. In 1995, 70.2% of AIDS cases among Canadian women of child-bearing age were in women who became infected with HIV through heterosexual contact or who did not have any identifiable risk factors [3]. According to this statistic, if only those women who were classified as being atrisk were counselled about HIV and HIV testing, a large proportion of women who are HIV-positive would not be identified. Furthermore, studies have shown that women with higher levels of education and women who received proper HIV counselling had higher rates of consent for HIV screening and ZDV intervention [4].
The Society of Obstetricians and Gynaecologists of Canada (SOGC) [5], the Canadian Medical Association [6], the College of Family Physicians of Canada [7], the Canadian Paediatric Society [8], the Canadian Paediatric AIDS Research Group [9] and the Reproductive Care Program (RCP) of Nova Scotia [3] recommend that all pregnant women be counselled about HIV and HIV testing, and be offered an HIV blood test during their pregnancy. Both the Departments of Obstetrics/Gynecology and Family Medicine at the IWK Health Centre, Halifax, Nova Scotia follow the SOGC and RCP guidelines.
The primary objective of this study was to determine the proportion of women in Nova Scotia who delivered at the IWK Health Centre who were counselled about HIV and HIV testing during pregnancy. A secondary objective was to determine the proportion of those who had received counselling who subsequently underwent the blood test.
Methods
Setting and study population
The study was conducted at the IWK Health Centre where, in 2000, there were 4625 deliveries (50% of all deliveries in Nova Scotia). All pregnant women who delivered at the IWK Health Centre between March 10 and May 10, 2000 were given a questionnaire to complete. The study was approved by the IWK Health Centre Research Ethics Board.
Procedures
A letter of introduction and a questionnaire were attached to the front of the packages for those with newborns that nurses distributed to mothers after delivery. The nurses were asked to mention the questionnaire to the women. The principal investigator met with the nursing staff before the study began to raise awareness about the importance of HIV screening, and nurses were reminded of their role throughout the two months. Completed questionnaires were placed in a sealed box at the nursing station. The return rate one month into the study averaged less than 20%; therefore, return envelopes were attached to the questionnaires to allow women the option of completing the questionnaire after they left the hospital.
Instrument
The questionnaire asked women for their ages, levels of education and histories of previous deliveries. They were also asked if they received counselling about HIV during their pregnancy and, if yes, who spoke to them and at what point in time. Furthermore, they were asked if they were offered an HIV blood test, whether they had an HIV blood test done and, if so, when it was performed. Finally, those who did not have an HIV blood test were asked for their reasons for not doing so. The demographics of the total population of women who delivered at the IWK Health Centre during the same time period were assessed and compared with the sample population.
Statistical considerations
Sample sizes of 400 and 200 were calculated to provide a point estimate with a 95% CI width of 10% for the primary objective and 15% for the secondary objective. With a predicted compliance rate of 50% for the return of the questionnaire, the survey was scheduled to continue for two months, which would have allowed the distribution of surveys to approximately 800 women.
The frequency distribution of all variables was calculated. Comparison of proportional data were analyzed with χ2 or Fisher’s exact test as appropriate to determine the significance of the association of each predictor variable with the two outcome variables.
Results
There were 858 births at the IWK Health Centre between March 10 and May 10, 2000. Letters were distributed to 800 new mothers and 155 questionnaires were returned (response rate of 19.4%) (Figure 1). The mean age of respondents was 29.7 years and more than 61% of those had completed postsecondary education or held an advanced degree (Table 1). A total of 65 (41.9%; 95% CI 34.1 to 49.7) women were counselled about HIV during their pregnancy and 47 (72.3%; 95% CI 65.3 to 79.3) of those who were counselled underwent the test.
| Patient characteristics | Mean | Respondents Range |
|---|---|---|
| Age (years) | 29.7 | 17–45 |
| Previous deliveries | 0.7 | 0–5 |
| Education | Total | Proportion (%) |
| Some high school | 7 | 4.5 |
| Completed high school | 18 | 11.6 |
| Some postsecondary | 35 | 22.6 |
| Completed postsecondary | 79 | 51.0 |
| Advanced degree | 16 | 10.3 |
Table 1: Patient characteristics among respondents to a questionnaire distributed between May 10 and March 10, 2000 for women who delivered at the IWK Health Centre
There were significant differences between: the proportion of women counselled and whether the current delivery was their first delivery or if they had previous deliveries (P=0.050); the proportion of women offered a test and their ages (P=0.028); and the proportion of women who underwent a test and their ages (P=0.017) (Table 2). There were no significant differences between: the proportion of women counselled about HIV and their ages and levels of education; the proportion of women offered an HIV blood test and their levels of education and histories of previous deliveries; and the proportion of women who had an HIV blood test and their levels of education and histories of previous deliveries.
| Variables | Younger than 25 | Age (years) 25 or older | P | Level of education | |||||
|---|---|---|---|---|---|---|---|---|---|
| High school or less | Postsecondary | P | Previous deliveries | ||||||
| Yes | No | P | |||||||
| Number counselled (%) | 12 (7.7) | 53 (34.2) | 0.093 | 12 (7.7) | 53 (34.2) | 0.52 | 37 (23.9) | 28 (18.1) | 0.050 |
| Number not counselled (%) | 8 (5.2) | 82 (52.9) | 13 (8.4) | 77 (49.7) | 36 (23.2) | 54 (34.8) | |||
| Test offered (%) | 13 (8.4) | 51 (32.9) | 0.028 | 13 (8.4) | 51 (32.9) | 0.27 | 36 (23.2) | 37 (23.9) | 0.072 |
| Test not offered (%) | 7 (4.5) | 84 (54.2) | 12 (7.7) | 79 (51.0) | 28 (18.1) | 54 (34.8) | |||
| Test done (%) | 14 (9.0) | 55 (35.5) | 0.017 | 13 (8.4) | 56 (36.1) | 0.51 | 38 (24.5) | 31 (20.0) | 0.078 |
| Test not done (%) | 6 (3.9) | 80 (51.6) | 12 (7.7) | 74 (47.7) | 35 (22.6) | 51 (32.9) | |||
Table 2: Hypothesized predictor variables associated with HIV counselling and screening of women who delivered at the IWK Health Centre in Nova Scotia
The proportion of women who were offered an HIV blood test was 64 of 155 (41.3%); 14 of those women chose not to have the test done (Figure 1). An additional 20 women requested and underwent the test without it being offered; therefore, the total number of women who had an HIV test was 70 of 155 (45.2%).
Women were counselled by their family doctor (n=50, 76.9%), an obstetrician (n=16, 24.6%), a nurse (n=8, 12.3%), an obstetrical resident (n=3, 4.6%) or another health care worker (n=1, 1.5%). Counselling was done predominantly during the first trimester of their pregnancies (n=60, 92.3%), followed by the second trimester (n=8, 12.3%) and the third trimester (n=2, 3.1%). No women were counselled at the time of or after delivery. The women who underwent an HIV blood test during their pregnancy did so during the first trimester (n=54, 77.1%), followed by the second trimester (n=14, 20.0%) and the third trimester (n=2, 2.9%). No women were tested at the time of or after delivery.
Women who did not have an HIV blood test were asked for their reasons for not doing so. Reasons given included: not at risk (n=20), not offered (n=23), not sure if test was done (n=7), in a monogamous relationship (n=13), not a concern (n=10), tested recently (n=13), uncomfortable asking for one myself (n=1), no time to do it (n=1), automatically done in another province (n=2) and do not know (n=4).
The age and the number of previous deliveries of the women who completed the questionnaire (age – mean 29.7±5.1 years, range 17 to 45 years; previous deliveries – mean 0.8±0.9, range 0 to 5) were similar to those of all women who delivered at the IWK Health Centre during the same time period (age – mean 29.7±5.2 years, range 15 to 49 years; previous deliveries – mean 0.8±0.9, range 0 to 5).
Discussion
This study demonstrates that a substantial number of pregnant women were neither counselled about HIV during their pregnancy nor offered an HIV blood test. However, of those women who were counselled about HIV, most had an HIV blood test done. These results confirm previous studies that found that when women are counselled and offered an HIV blood test, they are more likely to have a blood test done [4]. The results also indicate that in Nova Scotia, family doctors, obstetricians and nurses may be involved in the counselling process and that those who are involved are following the guidelines outlined by the Reproductive Care Program of Nova Scotia. These guidelines state that:
women should be counseled about HIV and offered an HIV blood test during the first trimester of their pregnancy. However, if not completed by the second and third trimesters, counseling and testing should be done at these times. [3]
Although many women did not receive testing because they did not perceive themselves to be at risk, some women indicated that they were not offered a blood test. It is possible that if they had been offered an HIV test, they may have considered having it done. A history of previous births was a predictor that the proportion of women counselled and an age below 25 years was associated with higher rates of counselling and higher rates of women who had the HIV test done. Also of concern is that many women did not know whether they were tested for HIV during the series of routine prenatal tests. If they had been counselled about HIV, they would have known that HIV is not included in the routine prenatal tests, but can be done at the same time if requested.
The major limitation of this study was the smaller than anticipated response rate, which may have introduced bias. Different response rates may be related to level of education, culture, duration of stay in hospital, parity and inconsistent reminders by nursing staff. There are no demographic data on the nonresponders except that the age and previous deliveries of the women who completed the questionnaire were similar to those of all women who delivered at the IWK Health Centre during the same time period. We hypothesize that the reason for the poor return rate was that the questionnaire was distributed to the women at a very busy and exciting time, when they had a lot of other paperwork to complete. However, a sensitivity analysis indicated that if all 645 women who did not respond actually had been counselled, the proportion of women counselled would have been 710 of 800 (88.8%). In contrast, if all 645 women who did not respond had not been counselled , the proportion of women counselled would have been only 65 of 800 (8.1%). Some medical authorities suggest that HIV counselling programs during pregnancy should target a minimum standard of 90% to 95% of women. Therefore, both the survey’s results (41.9%) and the hypothetical extremes (8.1% to 88.8%) are unacceptably low.
These results indicate that all health care professionals involved in the care of pregnant women need to be reminded of the importance of HIV counselling and testing during pregnancy. If education cannot improve the proportion of women who are counselled and offered an HIV blood test during their pregnancy, then policies may need to be changed. New policies could include mandating HIV counselling by all professionals involved in obstetrics, or mandating HIV testing of all pregnant women in Nova Scotia. However, these types of options are not commonly seen in clinical medicine. The most favourable options may be additional education of both health care providers (rounds, in-services) and the public (prenatal classes, educational brochures in hospital and physician waiting rooms), and systems modifications such as check-off boxes on prenatal and labour and delivery forms. Whatever interventions are implemented, follow-up audits are necessary to evaluate whether the current standards are being met.
Acknowledgements
We thank the nurses of the Maternal and Newborn Health Program of the IWK Health Centre for their assistance with the study survey.
References
- Health Canada. HIV/AIDS Epi Update: Perinatal Transmission of HIV. May 2001. <www.hc-sc.gc.ca/hpb/lcdc/bah/epi/peri_e.html>. (Version current at August 1, 2001)
- Connor EM, Sperling RS, Gleber R, et al. Reduction of maternal-infant transmission of human immunodeficiency virus type 1 with zidovudine treatment. N Engl J Med 1994;331:1173-80.
- Reproductive Care Program of Nova Scotia. Guidelines for antenatal laboratory screening and testing and HIV counseling guidelines. Halifax: Reproductive Care Program of Nova Scotia, 1998.
- Oldenettel D, Dye T, Artal R. Prenatal HIV screening in pregnant women; a medical-legal review. Birth 1997;24:165-72.
- Society of Obstetricians and Gynaecologists of Canada (SOGC) Clinical Practice Guidelines. HIV Testing in Pregnancy. June 1997;62.
- Canadian Medical Association. Counselling Guidelines for HIV testing. Ottawa: Canadian Medical Association; 1995.
- Tessier D, Dion H, Grossman DW, Rachlis A. HIV Care: A Primer &
- Canadian Paediatric Society. Statement: Perinatal human immunodeficiency virus (HIV) testing. Can J Paediatr 1994;1:ID94-01.
- Samson L, King S. Evidence-based guidelines for universal counselling and offering of HIV testing in pregnancy in Canada. CMAJ 1998;158:1449-57.