Impact of telehealth in Bangladesh during the COVID-19 pandemic in 2020
2 The Center for Enterprise and Society (CES), University of Liberal Arts Bangladesh (ULAB), Dhaka, Bangladesh
Received: 22-Sep-2021 Accepted Date: Oct 06, 2021; Published: 13-Oct-2021
Citation: Rahman S, Amit S. Impact of telehealth in Bangladesh during the COVID-19 pandemic in 2020. Curr Res Integr Med. 2021;6(3):9-12.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Telehealth is allowing healthcare workers to see patients virtually in locations that were not accessible previously, and this has reduced cost and time as well as saved lives. Bangladesh is a developing country with only 6 doctors for every 10,000 patients. Due to the COVID-19 pandemic, a rising percentage of individuals in Bangladesh are turning to telehealth as it may provide more convenience and access to care for online consultations while minimizing the risks of virus transmission that may result from going to a healthcare provider. Our research question was to see if there was any impact of telehealth utilization on patient satisfaction during the pandemic in 2020. This study will leverage a timely national experiment to evaluate the users of telehealth across the Bangladeshi population. We obtained de-identified data for 200 patients among outpatient telehealth visits from Global Health Data Exchange as it captures telehealth use throughout Bangladesh. The analysis showed that 92% of participants were males in the study population, and had a higher dependency on telehealth than 8% of the females. We found that the youngest age group, had the highest dependence on telehealth, compared to any other age group in Bangladesh. The lowest dependence was among the oldest age group of 45 years and above. There was strong association between patient satisfaction and telehealth use.
Keywords
Telehealth; Healthcare utilization; COVID-19 pandemic
Introduction
Telehealth is the use of electronic information and technologies to support long-distance healthcare services from healthcare workers to patients remotely at any time and place. Bangladesh is a developing country with only 6 doctors per 10,000 patients. The healthcare sector is heavily focused in Dhaka, the capital city of Bangladesh; although, 64% of the population resides in rural areas and patients need to travel long distances to access healthcare services. Telehealth is allowing healthcare workers to see patients virtually in locations that were not accessible previously, and this has reduced cost and time as well as saved lives. With 60.3% of the total market as of 2019, North America is currently the largest telehealth market and is expected to remain so until 2025; however, the Asian market is predicted to grow fast.
Bangladeshi Telehealth practices began in 1999 through the Center for Rehabilitation of Paralyzed (CRP) by Swinfen Charitable Trust of the UK, which used store and forward-based telemedicine with digital cameras for taking images, but no real-time technology was applied. However, lack of marketing, poor logistics, and little connectivity meant that this approach did not succeed. In 2020, the COVID-19 pandemic led both government and non-government bodies to initiate telehealth for delivering patient care all over the country. Through a public project under the Directorate General of Health Services (DGHS), high-quality telehealth services were established at Bangabandhu Sheikh Mujib Medical University and the National Institute of Cardiovascular Diseases with 3 district hospitals (Shatkhira, Nilphamari, and Gopalganj) and 3 sub-district hospitals (Pirgonj, Dakope and Debhata) [1]. Among private projects, Praava Health, Evercare, Maya, and Telenor Health are some of the successful hospitals and organizations leading telehealth services in Bangladesh.
Although few people used telehealth services in the pre-COVID-19 period, the pandemic has led to a significant rise in telehealth services in Bangladesh. COVID-19 testing rate in Bangladesh during the initial outbreak was only 0.34%, the second lowest in South Asia, only after the war torn nation- Afghanistan. This also led people to stay home and seek medical assistance through virtual channels as many wanted to prevent catching the virus. During the pandemic, a rising percentage of individuals in Bangladesh were turning to telehealth as it may provide more convenience and access to care for online consultations while minimizing the risks of virus transmission that may result from going to a healthcare provider. This study will leverage a timely national experiment to evaluate the impact of telehealth across the Bangladeshi population. Despite the overall growth in telehealth in this country, it is unclear whether telehealth utilization has increased for patient populations for all age groups and both genders in 2020. The research question and hypothesis are as follows.
Research question
What impact did telehealth use have on patients’ healthcare satisfaction in Bangladesh during the COVID-19 pandemic in 2020?
Telehealth use is experiencing unprecedented growth. However, telehealth users’ demographics are unclear in Bangladesh. The research question aims to assess the demographics and impacts of telehealth use on healthcare satisfaction compared to in-person appointments with healthcare providers for healthcare utilization.
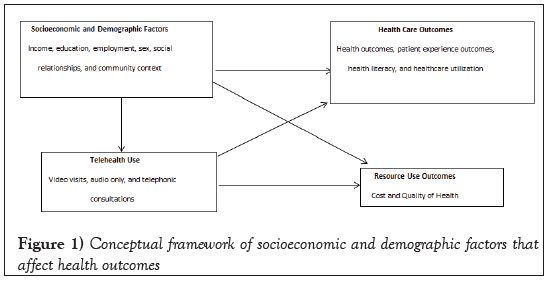
Conceptual framework
The conceptual framework as shown in Figure 1 shows hypothesized associations of socioeconomic and demographic factors that affect health outcomes. In the socioeconomic and demographic factors, the phenomenon indicates a patient’s absolute and relative position in society, including prestige, education, occupation, and wealth. For example, employment provides income, which influences choices of housing (residential and community), relationships among friends and family, food, medical care, and more. However, employment depends on education because the higher the education a person attains, the better employment opportunity he/she will typically receive. Employment sometimes depends on the gender/sex of an individual, considering there is a glass ceiling for women in Bangladeshi society. For example, females often experience discrimination in the job market and often receive less payment compared to men in the same position.
Figure 1: Conceptual framework of socioeconomic and demographic factors that affect health outcomes
Socioeconomic and demographic factors lead to varying health outcomes for patients because the higher the income or education the better health literacy he/she possesses and also the better health care he/she can seek, leading to improved healthcare utilization. Having a good job also leads to employers covering the cost of health insurance. Patient safety and patient experience outcomes are tied with income because patients with higher income can afford expensive treatments in elite hospitals. Many dimensions of social relationships, such as access to social networks and availability to emotional support, can be important to health through healthcare utilization, clinical processes of care, cost, and patient experience. This is usually identified through marital status, social support, and living alone. Residential and community context indicate housing, walkability, broadband coverage, access to transportation, safety, and proximity to services. Patient experience will include communication with nurses and doctors, access to timely appointments and information, the responsiveness of healthcare staff, care coordination, pain management, medication information, and overall experience.
In terms of resource use outcomes, cost and quality of health depend on which part of the region the hospital is located in as well as how expensive the treatment is (better or expensive treatment can be afforded by patients with higher socioeconomic status). For example, patients residing in Gulshan area of Dhaka City, usually turn to United Hospital, which is expensive but has one of the highest rankings in terms of quality, whereas patients in Old Dhaka area might turn to Capital General Hospital, which is cheaper but has one of the lowest rankings in terms of healthcare quality. Also, hospitals using telehealth services will likely see reduced admission rates and mortality in patients, and patients will also incur reduced healthcare- related costs (e.g., transportation costs). However, rural populations might not have sufficient internet access and might not be able to utilize telehealth services in comparison to other populations. Simultaneously, health care outcomes directly affect the resource use outcomes, mainly through high administrative costs, costly new technologies, expensive drugs, and physician fees. However, if the patient seeks telehealth, then the costs are likely to decrease as telehealth leads to improved patient outcomes through advanced monitoring, cognitive affordances, execution of life-saving, and evidence- based critical care protocols. Moreover, telehealth increases the ability to access timely care by reducing potential travel issues or transfers to other health care facilities.
The government of Bangladesh has declared it will fix fees for healthcare services in private hospital, and this will lead to reduced cost of care, while improving quality of health.
Literature Review
Telehealth usage during the COVID-19 pandemic has become one of the vital tools for patients to seek medical assistance. While there are a few studies regarding its utilization in Bangladesh, none of them have incorporated demographic and socioeconomic aspects of the Bangladesh populations. Uscher-Pines et al. analyzed the overall impact of telehealth by Teladoc, where only 7% of the patients had follow-up visits compared to patients who visited physicians’ offices or Emergency Departments (ED) for similar conditions [2]. Another study by Uscher-Pines et al. assessed how telemental health is deployed through semi-structured 60-minute telephone interviews with providers and found that 48% used a range of services [3]. In a comparison study between quality and access to care at Teladoc using claims from 18-64 years old enrollees in a state, it was found that 3,043 patients used telehealth services 4,657 times, but Teladoc is only on-demand telehealth care and has a gap in addressing other types of telehealth [3]. A study between March to April 2020 conducted a semi-structured interview with 20 outpatient psychiatrists with COVID-19 cases and patients who experienced satisfaction using telehealthcare services, but the inability to observe nonverbal cues, limited bandwidth, and incompatible devices were some issues for underserved patients [4]. The Diabetic Association of Bangladesh (BADAS) provided telehealth to children and adolescents with type 1 diabetes through phone calls and text messages, where 235 patients received advice over the phone from March to April 2020, and 52% of them were from the capital city, Dhaka [5]. Most of the patients experienced hyperglycemia and were advised accordingly, and the study recognized telemedicine as a solution for routine care of diabetic children who are unable to travel long distances to clinics.
Rural Bangladesh has good acceptability for telehealth, with a mean age of 32.38, a monthly income of approximately 9000BDT, and a maximum of 17 years of schooling [6]. However, no study has been conducted involving both rural and urban parts of the country to assess telehealth efficacy. Usability issue is one of the barriers in telehealth adoption; 61% of usability problems contributed to slow adoption of mobile health usage [7]. But this paper only examines mobile applications and could be extended to other forms such as web applications.
Systematic reviews showed that telehealth interventions produce positive outcomes when they are used for remote patient monitoring, especially for chronic conditions (e.g. cardiovascular and respiratory disease) and psychotherapy (e.g. behavioral health), with improvement in mortality rate, quality of life, and reduced hospital admissions, reduced patient time in emergency departments, reduced heart attack mortality during emergency services and improved access and clinical outcomes for outpatient consultations [8]. Moreover, research in telehealth should be integrated with new models of payment and care to assess the continuum of care in organizations. A paper studied four years of data from a nationally representative biannual consumer survey of telehealth use trends and the role policies play in its usage [9]. As Bangladesh is a developing country, there are several challenges including digital divides and disparities, and the equipment facilities in e-health services for both patients and healthcare providers should be increased, along with making separate laws and reimbursement policies for physicians and patients [10]. Currently, the physician cost of telehealth and in-person visits is the same in most hospitals and clinics.
Some studies have overestimated the rates of telehealth use as it was conducted online and so excluded people with limited internet access, and there was the possibility of self-reported bias as the data was retrospective. Moreover, policies need to be made to incentivize providers and health systems to use telehealth even after the pandemic, such as offering financial incentives to providers to adopt telehealth. For example, Kaiser Permanents Medical Group gave a complimentary iPhone and data plan to all 9000 physicians to support telehealth use and counts telehealth visits similar to in-person visits. Furthermore, the removal of financial consumer barriers to using telehealth for low-income populations can enhance telehealth visits. This can include implementing waivers or discounts to purchase needed equipment such as smartphones, data plans, or sufficient internet coverage. Misinformation and lack of communication networks made the healthcare system crumble, vulnerable and incompetent. In such chaos, national media outlets failed to efficiently and effectively deliver reliable information to the audience from all walks of life, letting the more personalized and internet-based occupy the communication space [11]. However, there is insufficient broadband coverage in most of the rural areas, posing further challenges to telehealth usage. It must be noted that even if telehealth service is widely available (i.e. during the COVID-19 pandemic), some rural patients might not have complete information on how, when, and where (through which platform) to use it. Therefore, improving education and awareness in underserved communities can increase overall health outcomes. The Ministry of Health in Bangladesh can mobilize investments to improve telehealth infrastructure and provide enough access to such populations and underserved communities.
Data and Methods
Study sample
We obtained de-identified data for outpatient telehealth visits from Global Health Data Exchange as it captures telehealth use throughout Bangladesh. It contains standard data elements such as demographics, diagnosis, age, income, gender, race/ethnicity, education, and more. Our sample is from age 16 to 45 and over, gender is only males and females and the study period is 2020 only. This cross-sectional data, consisting of 200 Bangladeshi patients was part of the COVID-19 health services disruption survey 2020, which was developed to assess the level of disruption to a wide range of health services resulting from the pandemic and government mandates that lead to changes in behavior to mitigate the spread of the virus. It was funded by Bill and Melinda Gates Foundation (BMGF) and there were several contributors including the Institute for Health Metrics and Evaluation (IHME), BMGF, Premise Data Corporation, Ipsos, and ORB International. There were a total of 36 questions in the survey including the questions relating to health conditions, time spent with a healthcare provider, frequency of visits, medication, average income per month, and more.
Study outcomes
The primary outcome of interest was whether patients had any satisfaction after telehealth use which was assessed through pre and post-telehealth use. Multiple regression analysis was done in association with telehealth use, gender, and change in income (pre and post). For the secondary outcome of interest, we were able to capture and see if there was any causality between gender and telehealth use as well.
Covariates
We were able to examine the covariates such as gender and age group from the sample of 200 patients. We were able to do multiple linear regressions to examine the causality of income and telehealth visits.
Analysis
A statistical multiple regression model is:
Yi=a+b1Xi1+b2Xi2+…+bkXik+ei, were the estimated multiple regression model is:
ei~N(0,Ϭ2) i=1,2,…n.
“Fitted” Yi:Yi (An important tool).
Yi would have been the Y values if the regression model were perfect.
Yi=a+b1Xi1+b2Xi2+…+bkXik+ei
That is, if ei were exactly zero.
The null and alternate hypotheses in this study are:
H0: Telehealth usage led to no change in labor market productivity for patients=0 vs. H1: Telehealth usage led to higher labor market productivity for patients>0.
After obtaining the data from Global Health Data Exchange, the file contained data from many countries and we extracted only the data for Bangladesh and excluded other countries, which had 200 de-identified Bangladeshi participants. Initial cleaning was performed to identify missing variables. The dependent variable was the provider, where we wanted to see the impact on telehealth. The independent variables were gender (male or female), 5 age groups, and pre-and post-income to assess labor market productivity, which was in monthly salary in BDT. We labeled ‘1’ to male and ‘0’ to female. Participants in this study were more commonly male (92%) with the common age group of 16-25 years old (65%). Among the providers, we labeled home as ‘1’, which means the patients took virtual consultation with the physician from home and considered in-person consultation with a physician as a health facility and labeled it ‘0’. There were 5 age groups of 16 to 25 (65%), 26 to 35 (25%), 36 to 45 (7%) 45 above (2%) and under 16 (1%). The analysis was done through STATA version 16.
Results and Discussion
The analyses showed that among 92% of participants were males in the study population, and had higher dependency on telehealth than 8% of the females. However, dependency on in-person consultation (health facility) was also higher for males too. It was also interesting to see that females had a very low ratio of medical assistance rates compared with males with a 14:166 ratio in Table 1.
| Total No. | ||||
|---|---|---|---|---|
| Gender | Frequency | Percent | ||
| Female (0) | 16 | 8 | ||
| Male (1) | 184 | 92 | ||
| Total | 200 | 100 | ||
| Users | Health facility (0) | Home (1) | Total | |
| Female (0) | 10 | 4 | 14 | |
| Male (1) | 120 | 46 | 166 | |
| Total | 130 | 50 | 180 | |
| Age | Health facility (0) | Home (1) | Total | Mean (SD) |
| 16 to 25 | 84 | 33 | 117 | 0.93 (0.24) |
| 26 to 35 | 33 | 12 | 45 | 0.88 (0.32) |
| 36 to 45 | 10 | 4 | 14 | 0.85 (0.36) |
| Over 45 | 3 | 1 | 4 | 1 (0) |
| Under 16 | 0 | 0 | 0 | 0 |
| Total | 130 | 50 | 180 | 0.92 (0.27) |
Table 1: Characteristics of patients in the sample
To see if there was any causality with the provider (telehealth or inperson visits), we ran simple linear regression and found no relationship (p-value=0.945>0.05) with a 95% confidence interval. The dependent variable was provider and gender was the independent variable. The number of observations was 180 with a mean of gender 0.922 and a standard deviation of 0.2686. The mean of the provider was 0.2777 and the standard deviation was 0.4491.
33 of the participants between the ages 16 to 25 opted for home consultations, which were the highest, followed by the 26 to 35 years of age group. The least dependency was for the age group over 45 years. Participants less than 16 years of age were excluded as none of them visited any type of provider.
To see if there was any relationship between telehealth and patient satisfaction, the analysis showed that there was a strong relationship between patient satisfaction and telehealth use (p-values<0.05), with a 95% confidence interval as showed in Table 2.
| Coefficient (Std. err.) | P-value | t | |
|---|---|---|---|
| Gender | -0.0166 (0.12) | 0.03 | -0.13 |
| Patient satisfaction | 0.48 (1.54) | 0.02 | 0.01 |
| Constant | 0.2857 (0.1206) | 0.019 | 2.37 |
| No. of observations | 180 |
Table 2: Regression analysis to see association between gender, patient satisfaction and telehealth use
We performed a multiple regression analysis with the use of telehealth use as the dependent variable, with gender, patient satisfaction as independent variables.
We also performed a simple linear regression to see if there was any causality between healthcare provider and gender and found no causality as p-values>0.05 at 95% confidence level as showed in Table 3.
| Coefficient (and standard error) | P-value | |
|---|---|---|
| Constant | 0.2857 (0.1203) | 0.019 |
| Gender | -0.0086 (0.1253) | 0.945 |
| R-squared | 0 | |
| Adjusted R-squared | -0.0056 | |
| No. of observations | 180 |
Table 3: Causality between the provider (telehealth or in-person visit) and gender
Conclusion
For the age groups, we found that the youngest age group, 16-25, had a higher dependence on telehealth, compared to any other age group in Bangladesh. It can be because this age group is highly acquainted with technology and very aware of where to seek help when it comes to online platforms. The lowest dependence was among the oldest age group of 45 years and above. This might be because this generation is least acquainted with technology and least aware of online platforms. Technical literacy is also a reason here because older generations have difficulty using mobile phones and computers. We wanted to see which gender used telehealth more often, and found that males more commonly used telehealth platforms for medical assistance. However, it was interesting to note that men also had higher usage with in-person consultations too. This can be because our sample had 92% males, which lead to a higher number of male telehealth users. For research question, we wanted to see if there was any causality between telehealth use and patient satisfaction. Overall, users of telehealth have increased dramatically in Bangladesh due to the COVID-19 pandemic, but disparities exist among genders and age groups. Although telehealth aims to provide patient care remotely and improve access to healthcare among rural patients, it is mainly used among urban populations, due to technical literacy and awareness within urban patient populations. For telehealth to more successfully reach out to rural patients, the Bangladeshi government should increase funding and help startups to lead the way. Currently, venture capital investments are not allowed tax rebates, and only the 2% stamp duty is waived. As rural patients are the most deprived population, investing in rural-based health startups can help improve their access. The higher income class has been the first adopters of telehealth and lower-income groups will be the last, but this disparity needs to be addressed.
Limitations
One of the limitations in assessing this can be since this data was based on a self-reported survey and participants might not have mentioned their incomes honestly. Another limitation is that the survey included only 200 participants with 92% males, and the majority was in the 16-25 years old age group, which does not represent the entire population. Not all sections and questions within sections are relevant to all populations, and this could introduce a “selection bias”. Like any other survey design, this survey additionally suffers from potential “recall bias” requiring patients to remember past events regarding their doctor visits. Additionally, with a sample size of only 200, it is difficult to generalize our conclusion to over 163 million Bangladeshis, hence our study might lack generalizability.
REFERENCES
- Light Castle Partners. Telemedicine for Bangladesh: Bridging the doctor-patient gap. Light Castle Analytics Wing. 2020.
- Uscher-Pines L, Mehrotra A. Analysis of teladoc use seems to indicate expanded access to care for patients without prior connection to a provider. Health Affairs. 2021; 33(2): 258-264.
- Uscher-Pines L, Raja P, Qureshi N, et al. Use of tele-mental health in conjunction with in-person care: A qualitative exploration of implementation models. Psychiatric Services. 2020; 71(5): 419-25.
- Uscher-Pines L, Sousa J, Raja P, et al. Suddenly becoming a “Virtual doctor”: Experiences of psychiatrists transitioning to telemedicine during the COVID-19 pandemic. Psychiatric Services. 2020; 71(11): 1143: 1150.
- Zabeen B, Bhowmik B, Huda K, et al. Use of telemedicine for the management of type 1 diabetes in children and adolescents in Bangladesh during the COVID-19 pandemic. J Diabetol 2020;12:18-21
- Iqbal MH. Telemedicine: An innovative twist to primary health care in rural Bangladesh. J Primary Care Community Health. 2020.
- Agency for Healthcare Research and Quality, AHRQ. Telehealth-mapping the evidence for patient outcomes from systemic reviews. Mtelehealth. 2019.
- Jeongyoung P, Clese E, Preeti I. Are state telehealth policies associate with the use of telehealth services among underserved populations? Health Affairs. 2018; 37(12).
- Chowdhury SR, Sunna TC, Ahmed S. Telemedicine is an important aspect of healthcare services amid COVID-19 outbreak: Its barriers in Bangladesh and strategies to overcome. Int J Health Planning Management. 2020;1-9.
- Al-Zaman MS. Healthcare crisis in Bangladesh during the COVID-19 Pandemic. The American J Tropical Med Hygiene. 2020; 103(4): 1357-1359.
- Taufique J, Chaudhury T, Mannan I. Universal health coverage in Bangladesh: Activities, challenges and suggestions. Advances in Public Health. 2019;209(12).