Long-term outcomes of veno-venous bypass operations in postthrombotic syndrome
2 Kazan State Medical University, Kazan, Russia, Email: imignatiev@rambler.ru
3 Vishnevsky Institute of Surgery, Moscow, Russia, Email: info@angiolsurgery.org
4 Russian Medical Academy of Postgraduate Education, Moscow, Russia, Email: info@angiolsurgery.org
Received: 26-Jul-2017 Accepted Date: Jul 26, 2017; Published: 11-Aug-2017
Citation: Ignatyev IM, Pokrovsky AV, Gradusov EG. Long-term outcomes of veno-venous bypass operations in post-thrombotic syndrome. J Phlebol Lymphol. 2017;10(1):5-9.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
BACKGROUND: Surgical reconstructions for venous occlusive disease are rarely performed. Consequently, reliable data on long-term patency, clinical outcome, hemodynamic evaluation and risk factors for graft occlusion are poor. The present study was aimed at assessing long-term results of venovenous bypass operations in postthrombotic syndrome (PTS).
METHODS: We analyzed long-term outcomes of crossover vein bypass procedures in 68 patients with unilateral postthrombotic iliac vein obstructions at periods from two to 28 years and 12 patients who underwent saphenopopliteal bypasses for femoral vein obstructions.
RESULTS: It was validated that the decisive factor of the success of the crossover bypass procedure was a sufficient diameter of venous graft, i.e., not less than 7–8 mm. The advantage of dilated great saphenous vein of affected extremity is shown in this study. It has been determined that in 70.6% of the patients, crossover grafts have a propensity to dilate, furnishing the requisite venous blood outflow from an affected extremity. Venous hemodynamic studies of the affected extremity with occlusion of the external pressed graft revealed that crossover bypass assumes the primary role in the maintenance of venous return. In 15 years, cumulative patency of crossover grafts was 77%. There was cumulative clinical success in 71% of the patients. The patency rate of saphenopopliteal grafting within the period up to 12 years was 91.7%. Long-term outcomes of the procedures proved durable functioning of the grafts and improvement of regional venous hemodynamics. There was significant improvement of reconstructive operations with the usage of distal arteriovenous fistulas.
CONCLUSION: Long-term results demonstrated a high efficacy of venovenous bypass operations in PTS.
Keywords
Post-thrombotic iliac vein obstruction, Femoral vein obstruction, Crossover bypass, Saphenopopliteal bypass, Duplex ultrasound, Venous hemodynamics
One of the most widespread reconstructive operations employed for unilateral post-thrombotic iliac vein occlusion is the cross-femoral saphenous vein bypass, also known as the Palma procedure [1]. In recent years, endovascular stenting operations for iliac vein obstructions have been widely utilized in clinical practice due to their minimally invasive techniques and reliable long-term outcomes. Today, the crossover bypass is perceived as an alternative reconstruction, if endovascular options fail or they are not possible [2,3]. In a few large series have been reported, overall patency of saphenous vein Palma grafts including about 400 operations ranged between 70% and 83% at three-five years [4]. Some authors have reported good results utilizing externally supported polytetrafluoroethylene (PTFE) prosthetic grafts, coupled with proximal arteriovenous fistula (AVF) formation [5]. In order to improve the results of crossover bypasses, Gloviczki and Cho were the first to perform an endophlebectomy from the femoral vein of the affected extremity [6].
The operation that was proposed for surgical correction of femoral vein obstruction is the saphenopopliteal vein bypass also known as the May- Husni procedure [7] which has not been widely used. The worldwide experience includes about 150 performed operations during a period of 60 years. However, in recent years, the interest in this type of intervention has reappeared. Some authors obtained good results of the graft patency rate performing this procedure [8,9].
This case series describes long-term results of veno-venous bypass operations.
Materials and Methods
From 1985 to 2012, we performed crossover bypass procedures in 96 patients with iliac vein obstructions (out of 236 examined patients with the given obstruction). Saphenopopliteal bypasses were done in 14 patients with femoral vein obstructions. There were 62 men and 48 women among the patients, aged from 17 to 60 years (mean – 41.6 years). According to the CEAP, the patients were classified, as follows: C4a–26 patients, C4b–51, C5–29, C6–4 (some of the patients were retrospectively evaluated with the CEAP classification). The duration of the disease was from six months to 21 years (mean-9.3 years). Recurrent venous ulcers were revealed in 24 patients. The left-sided vein obstructions were determined in 78 patients, and right-sided ones, in 32 [10].
Contrast phlebography, dynamic radionuclide phlebography (gamma-camera MB-9100, Hungary), duplex ultrasound (HDI-5000, Phillips Medical Systems; VIVID-7, General Electric Medical Systems, USA), and strain-gauge plethysmography (Angioflow2, Microlab, Italy) were used to assess the venous image and peripheral hemodynamics.
The indications for the bypass procedures were established for patients with obstructive lesions associated with severe chronic venous insufficiency (CVI) that is resistant to traditional methods of conservative and surgical treatment.
The aim of different techniques of crossover bypass formation was to create a graft with an adequate diameter that is not less than 7-8 mm. The transposition of the great saphenous vein (GSV) of the unaffected extremity was done when the vein exceeded 6 mm in diameter. In 39 cases panel vein graft utilizing contralateral GSV was used (“classic” Palma procedure), and 57 dilated GSV of the affected extremity was used as a graft. In the latter case, we reinforced the graft by carcass spiral in order to prevent its future dilatation. This approach to crossover bypass was advocated by Vedensky [11].
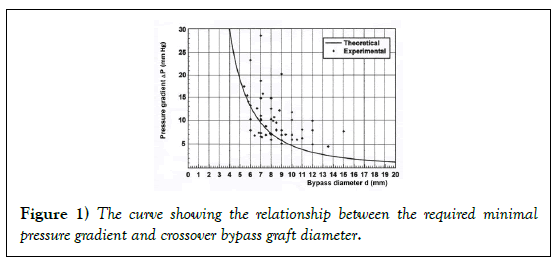
The mathematic model of crossover bypass operation was based on clinical and experimental research. In this model the relationship was established between the bypass diameter and the pressure gradient (between the common femoral vein (CFV) of the affected and normal extremities) necessary for its function maintenance and the graphic curve was plotted, which serves a reference point for determination of the ratio between the parameters indicated (Figure 1) [10].
In 20 patients, the reconstructive operations were combined with formation of distal AVFs between the posterior tibial arteries and veins. In five patients, we performed reconstructions of the aneurysmal transformations of the grafts (graft resections that are placed in external Vedensky spiral correctors). In two cases, we eliminated stenoses of the crossover grafts.
24 patients were identified with isolated femoro-popliteal venous obstruction, 18 of them were symptomatic enough to suggest surgical intervention. Fourteen (58.3%) patients underwent the operations. In four cases, the GSV was inadequate for the bypass procedures due to its small diameter. In two patients, we utilized a reinforced axillary vein segment with a valve into a slightly dilated GSV. In four cases, reconstructive operations were combined with the AVFs creation in the lower third of the calf.
Statistical Analysis
Statistical data processing was performed with licensed statistical software package Statistica 7.0 (StatSoft Inc., USA). The clinical characteristics of patients are presented by methods of descriptive statistics. Data were expressed as mean ± SD values. The variables were analyzed with nonparametric Wilcoxon test. Differences of categorical data were tested using χ2 test. Kaplan–Meier curves were used to calculate cumulative patency rates and cumulative clinical success rates. A P value <0.05 was considered statistically significant.
Results
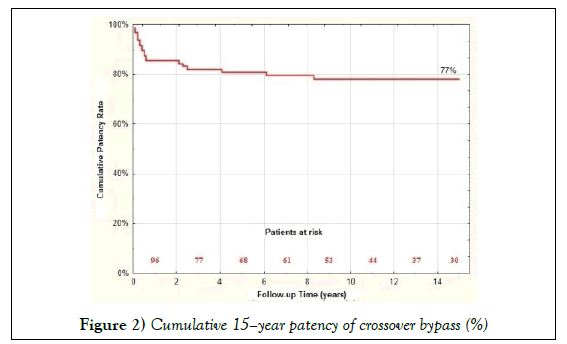
Long-term outcomes of the crossover bypass graft were followed in 68 patients during the period from two to 28 years (mean – 9.8 years), in 12 patients – of saphenopopliteal grafting from one to 12 years (mean – 5.1 years). In 15 years, cumulative patency of crossover grafts was 77% (Figure 2).
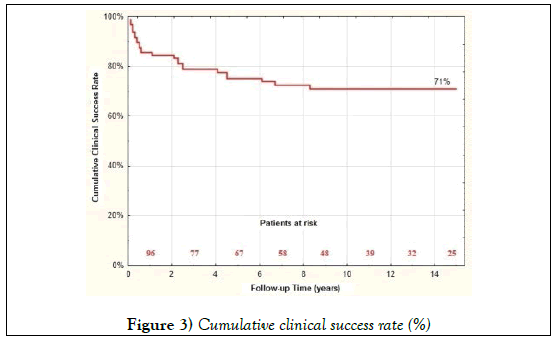
Cumulative clinical success (defined as alleviation of symptoms and/or healing of ulcers) was in 71% of patients (Figure 3).
Recurrent venous ulcers occurred in two cases. The remainder of the patients showed neither any significant improvement, nor recurrent venous ulcers. In some cases, the absence of prolonged clinical effects was explained by pathological aneurysmatic transformations or stenoses of the crossover grafts. Patency of dilated GSV graft is 84.5% vs. 69.2% of GSV of unaffected extremity (χ2 = 3.9, P<0.05).
The hemodynamic role of the bypass in the outflow from the extremity was assessed by strain-gauge plethysmography with occlusion of the graft by applying external pressure. The results demonstrated that the graft served as the main conduit for the blood outflow from the involved extremity (Table 1).
| Condition of the crossover graft | Number of patients (n=68) |
|---|---|
| Uniform dilatation | 48 (70.6%) |
| Pathological dilation (local or diffuse) | 14 (20.7%) |
| Stenoses | 2 (2.9%) |
| Recanalization after thrombosis | 2 (2.9%) |
| No alterations | 2 (2.9%) |
Table 1: Condition of crossover graft in the long-term period.
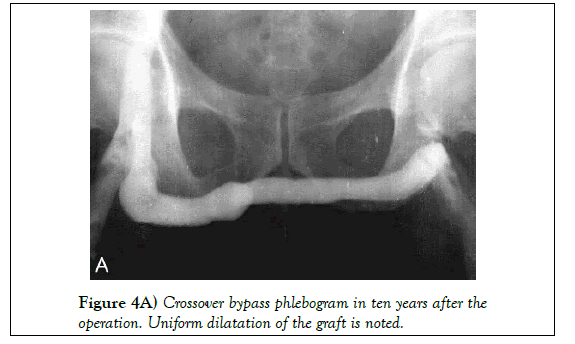
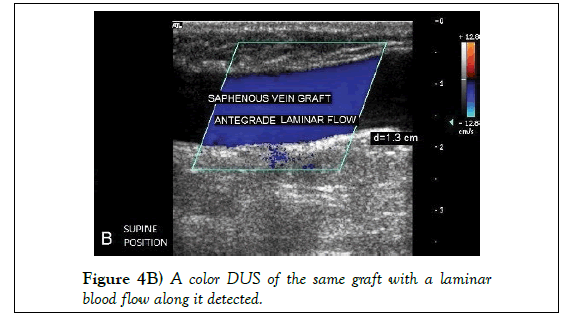
Phlebographic and duplex ultrasound (DUS) follow up demonstrated that the majority of bypasses, regardless of the techniques of their formation, undergo dilation with time. The bypass expands most intensively during the first two-three years. Uniform dilatations of the grafts in the long-term period were noted in 48 (70.6%) patients (Figures 4A and 4B).
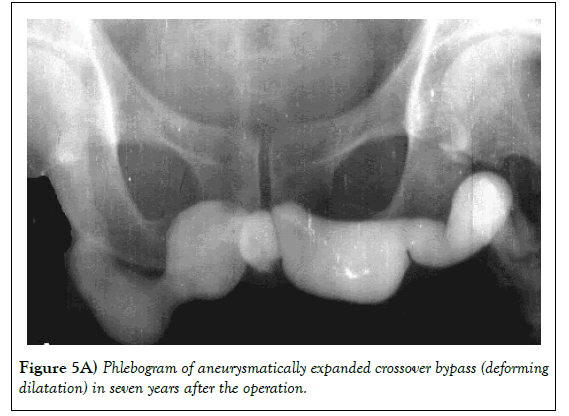
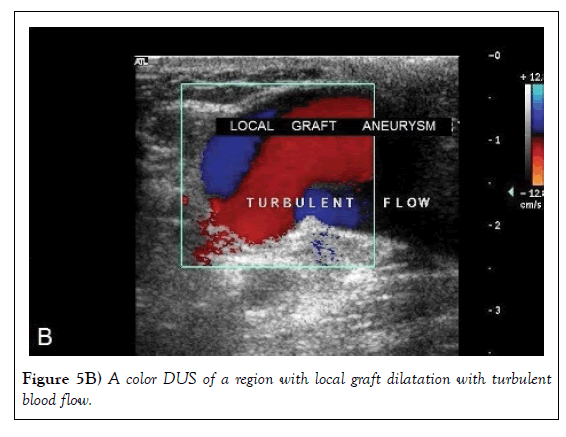
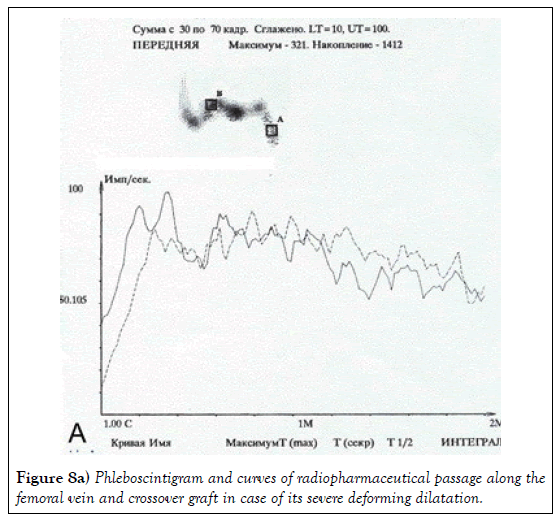
Pathological dilation (local and diffuse) of the graft (˃20 mm) was observed in 14 (20.7%) patients (Figures 5A and 5B).
Stenoses of the grafts were revealed in two (2.9%) patients. There were no alterations in two (2.9%) patients. Venous graft recanalization after thrombosis occurred in two (2.9%) patients (Table 2). Sixteen patients with well-functioning distal AVFs had patent crossover bypasses [12-15].
| VC (ml/100 ml) | MVO (ml/100 ml/min) | EV (ml/100 ml) | EF (%) |
|---|---|---|---|
| 3.58 ± 0.47 (2.91 ± 0.4) 0.10>P>0.05 |
59.76 ± 10.74 (38.11 ± 5.42) P<0.01 |
4.2 ± 0.56 (2.7 ± 0.71) P<0.01 |
68 ± 4.5 (36 ± 7.4) P<0.001 |
Table 2: Results of plethysmography at open and external pressed crossover graft (n=36).
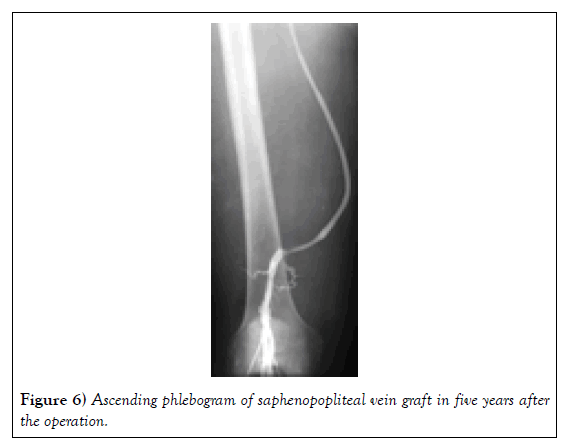
Long-term results after saphenopopliteal bypasses in ten (out of 12) patients showed symptomatic improvements. Graft thrombosis occurred in only one patient. In eleven (91.7%) out of 12 patients, the grafts were patent (Figure 6).
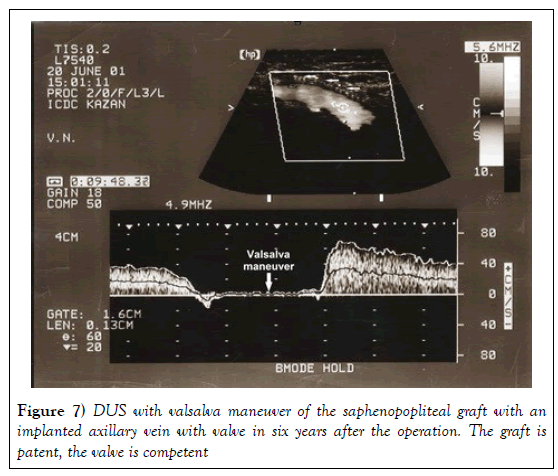
In six years after the operations, according to dynamic radionuclide phlebography, nine examined patients showed significant blood flow acceleration: initial mean of radiopharmaceutical transporting time was 30.83 ± 10.83s, and, after grafting, it decreased to 15.9 ± 3.93s (P<0.05). DUS data demonstrated a good graft function (Figure 7).
The mean diameter of the saphenopopliteal venous graft was 0.68 ± 0.11 cm. The quantitative parameters of the blood flow at rest and during exercises are shown in Table 3.
| at rest | at exercise test | P value | |
|---|---|---|---|
| Vmean, cm/с | 7,95 ± 1,09 | 10,07 ± 1,84 | < 0.05 |
| Vvol, ml/min | 133,92 ± 51,02 | 202,92 ± 62,68 | < 0.05 |
| Vmean, cm/с: mean linear velocity; Vvol, ml/min: volumetric velocity; n: the number of patients. | |||
Table 3 : Quantitative data of blood flow along saphenopopliteal graft at rest and exercise test(n=9).
Discussion
Surgical reconstructions for venous occlusive disease are rarely performed. Consequently, reliable data on long-term patency, clinical outcome, hemodynamic evaluation and risk factors for graft occlusion are poor. With increasing number of endovascular treatments of obstructions of both iliofemoral and femoro-popliteal segments, both open surgical procedures remain to be viable option for cases of failed primary procedure.
The principal target of this study is evaluation of long-term results of veno-venous bypass operation (crossover and saphenopopliteal bypasses), definition of durable graft function and hemodynamic evaluation.
It follows from the analysis of the above presented curve (Figure 1) that the crucial factor of a favorable outcome of crossover bypass operation lies in the graft diameter. The larger the diameter the higher the probability of successful bypasses functioning within the limits of the pressure gradient, approximating the real magnitudes, in patients with unilateral obstructions of the iliac vein (8 mmHg and less). These requirements are fulfilled by grafts no less than 7-8 mm in diameter. These conditions meet dilated GSV of affected extremity as it has a suitable diameter for graft and it lost its ability for a long spasm in comparison with GSV of unaffected extremity. This approach notes the advantage of our policy in choice of crossover bypass. So, in the study of Garg et al. [5] shows that cumulative 10-year primary patency of 25 Palma vein grafts is 49%, while in our study we demonstrate that cumulative 15–year patency of 30 crossover vein grafts is 77%.
Many authors note a considerable amelioration in the outcomes of crossover grafting under conditions of accelerated blood flow. [14,15] At the same time, some researchers are against the use of AVFs at reconstructions. We do not share the opinion that AVFs should be widely used for the crossover bypass procedures. However, we do consider AVFs to be used in the following cases: a “critical” 6–7 mm diameter of saphenous vein graft, incomplete recanalization of the femoral vein causing insufficient blood flow to the graft, or the necessity of creating an optimal pressure gradient between the CFV of the affected and normal extremities. In this group of patients, there were no cases of bypass thrombosis.
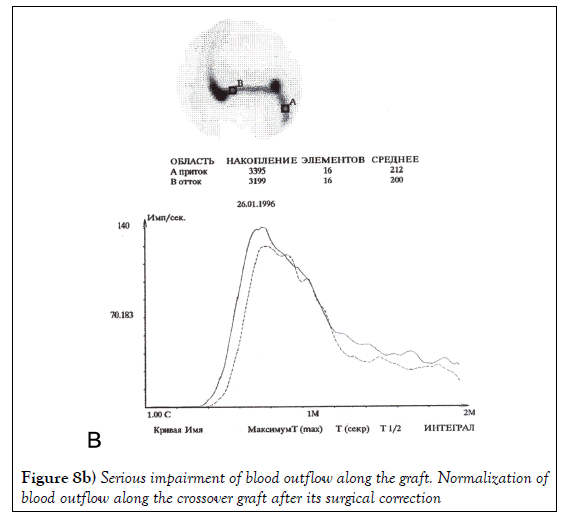
Crossover vein grafts expand over time and maintain an adequate blood outflow from the diseased extremity. This was cogently demonstrated by the results of noninvasive studies of venous hemodynamics in the involved extremity under conditions of open and external pressed graft. It has been shown that in the long-term periods, the main function in venous return is taken upon the crossover bypass. Some of the bypasses undergo pathological transformations in the form of local and diffuse dilatations and stenoses which, in some cases, deteriorate the conditions of blood outflow whereby minimizing the efficacy of reconstruction. Similar modifications of the grafts were also mentioned by Vedensky, Halliday et al., Lalka, Malone [11,16,17]. These authors restrain from repeated surgical bypass corrections in view of the great difficulties of their performance. On the contrary, we consider the given intervention justified despite definite technical difficulties, for it leads to the normalization of blood outflow in the bypass (Figures 8A and 8B).
Repeated reconstructions accomplished in seven patients over the period 7–16 years after crossover bypass were auspicious.
Isolated obstructions of the femoral veins rarely occur in clinical practice and generally do not result in severe disturbances of the blood flow due to specific features of collateral hemodynamics. A completely distinct case is observed when inadequate collateral blood flow is present along the deep femoral vein (DFV). This occurs with compromise of the DFV itself, as well as in case of blockage of the linked branches to the proximal part of the popliteal vein. The saphenopopliteal bypass procedure of the obstructed femoral vein is indicated in cases of insufficient collateral blood flow and severe venous hypertension in the distal part of the extremity. The improvement of the inflow (popliteal vein endovenectomy, AVF) or the outflow of the bypass (common femoral vein endovenectomy, iliac vein stenting, femoro-femoral crossover venous bypass) has the potential to enhance the patency of the May-Husni procedure [8]. The evaluation of the long-term outcomes of the procedure showed that saphenopopliteal bypasses are capable of well-functioning for a prolonged time (in comparison with crossover grafts) without their incompetency.
Conclusion
Long-term outcomes of the crossover vein bypass in unilateral iliac vein obstructions reveal the high efficacy proven by diagnostic evaluations of the venous hemodynamics. The main factor of the success is an optimal diameter of the venous graft.
Saphenopopliteal bypass in femoral vein obstruction is indicated in cases of collateral blood flow insufficiency of the DFV. Long-term outcomes showed a reliable function of the graft and improvement in regional venous hemodynamics. The grafts are capable of long-term well-functioning without pathological dilatation. The combination of bypass operations with distal AVFs formation increases patency of the grafts. Duplex ultrasound is considered to be a reliable noninvasive method of assessment for the function of veno-venous grafts.
Author’s Contribution
Conseption and design: Igor M. Ignatyev, Anatoly V. Pokrovsky, Evgeny G. Gradusov. Analysis and interpretation: Igor M. Ignatyev, Anatoly V. Pokrovsky. Data collection: Igor M. Ignatyev. Writing the article: All authors. Critical revision: All authors. Final approval of the article: All authors. Overall responsibility: Igor M. Ignatyev
Conflict of Interest
The authors certify that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript.
REFERENCES
- Palma ES, Esperon R. Vein transplants and grafts in the surgical treatment of the post-phlebitic syndrome. J Cardiovasc Surg 1960;1:94–107.
- Khanna AK, Singh S. Post-thrombotic syndrome: surgical possibilities. Thrombosis 2012:1–7.
- Gloviczki P, Kalra M, Duncan AA, et al. Open and hybrid deep vein reconstruction: to do or not to do? Phlebology 2012;27 Suppl 1:103-6.
- Gloviczki P, Oderich GS. Open surgical reconstructions for non-malignant occlusion of the inferior vena cava and iliofemoral veins. In: Gloviczki P, editor. Handbook of Venous Disorders. 3rd edn. London: Hodder Arnold; 2009:514-22.
- Garg N, Gloviczki P, Karimi KM, et al. Factors affecting outcome of open and hybrid reconstructions for nonmalignant obstruction of iliofemoral veins and inferior vena cava. J Vasc Surg 2011;53:383–93.
- Gloviczki P, Cho JS. Surgical treatment of chronic deep venous obstruction, In: Rutherford RB, ed. Vascular Surgery. 5th edn. New York: Elsevier; 2001:2099–165.
- Husni EA. In situ saphenopopliteal bypass graft for incompetence of the femoral and popliteal veins. Surg Gynecolol Obstet 1970;130:279–84.
- Coleman DM, Rectenwald JE, Vandy FC, et al. Contemporary results after sapheno-popliteal bypass for chronic femoral vein occlusion. J Vasc Surg: Venous Lym Dis 2013;1:45–51.
- Ryer JR, Misra S, Mc Bane RD, et al. Great saphenous vein transposition to the popliteal vein (the May–Husni procedure). J Vasc Surg: Venous Lym Dis 2013;1:82–3.
- Ignatyev IM. Hemodynamic aspects of crossover vein bypass graft in unilateral occlusions of the iliac veins. Angiol Vasc Surgery [Angiol i Sosud Chirurgia] 2002;8:37–49 (in Russian).
- Vedensky AN. Post-tromboticheskaya bolezn’ [Postthrombotic disease]. Leningrad: Meditsina; 1986:117–162 (in Russian).
- Neglen P. Endovascular reconstruction for chronic iliofemoral vein obstruction. In: Gloviczki P, editor. Handbook of Venous Disorders. 3rd edn. London: Hodder Arnold; 2009:491–502.
- Browse NL, Burnand KJ, Irvine AT, et al. Chronic deep vein obstruction. In: Diseases of the Veins. 2nd edn. London-Sudney-Auckland: Arnold; 1999:409–427.
- Vollmar J, Hutchenreiter S. Der quere Beckenvenen bypass (der “hohe Palma”). Vasa 1980;9:62–6.
- Simkin R, Esteban JS, Bulloj R. Surgical treatment of post-thrombotic syndrome [Article in French]. Phlebologie 1990;4:733–41.
- Halliday P, Harris J, May J. Femoro-femoral crossover grafts (Palma operation): A long-term follow-up study. In: Bergan JJ, Yao JST, eds. Surgery of the veins. New York: Grune & Stratton; 1985:241–5.
- Lalka SG, Malone JM. Surgical management of chronic obstructive venous disease of the lower extremity. In: Rutherford RB, editor. Vascular Surgery. Philadelphia: WB Saunders Co; 1989:1627–47.