Massive ossification in the parietal lateral lacunae of human superior sagittal sinus
Received: 02-Nov-2022, Manuscript No. ijav-22-5620; Editor assigned: 04-Nov-2022, Pre QC No. ijav-22-5620 (PQ); Accepted Date: Nov 23, 2022; Reviewed: 18-Nov-2022 QC No. ijav-22-5620; Revised: 23-Nov-2022, Manuscript No. ijav-22-5620 (R); Published: 30-Nov-2022, DOI: 10.37532/1308-4038.15(11).225
Citation: Tessema CB. Massive Ossification in the Parietal Lateral Lacunae of Human Superior Sagittal Sinus. Int J Anat Var. 2022;15(11):232-234.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
During the dissection of the cranial cavity of a 93-year-old male cadaver, two hard and irregular masses were incidental palpated in the parietal lateral lacunae of the superior sagittal sinus. Opening of both lacunae revealed two vascularized bony masses, which were firmly attached to the wall of the lacunae by fibrous bands. Each mass was found to have a gross appearance of cancellous bone with trabecular framework and multiple osseous canaliculi traversed by blood vessels. There were no observable pathological changes in the calvaria, other blood vessels and the brain in the vicinity of the lacunae. Such huge ossified masses can have mass effect on adjacent structures causing impaired venous blood flow and CSF absorption in the dural sinus with related complications and can also be important differential diagnoses for other intracranial clacifications or foreign bodies. Therefore, anatomists, pathologist, radiologist and neurosurgeons should be aware of such ossification in the dural sinuses.
Key Words
Ossification; Superior sagittal sinus; Parietal lateral lacunae
INTRODUCTION
Intracranial calcification is a common neuroimaging finding in otherwise asymptomatic, normal individuals as well as in patients with wide range of underlying conditions like neurologic, metabolic or developmental disorders, mitochondrial diseases, infectious diseases, neoplastic or other disorders and in patients with trauma or toxic history [1]. Patients with intracranial calcifications may exhibit movement disorders, seizures, cognitive impairments, and a variety of neurologic and psychiatric symptoms [1]. The advent and introduction of modern advanced and sophisticated imaging techniques like CT scan, cone beam CT, PET scan and MRI have brought magnificent changes in the ability of professionals, particularly radiologist, in the detection of calcifications/ossifications at various locations in the cranial cavity [2-7]. Several CT scan and cone beam CT studies demonstrated that intracranial calcifications can be physiological (age related), pathological or idiopathic. Physiological calcifications, unaccompanied by any evidence of a disease and have no demonstrable pathological cause, are common and occur in both sexes at any age and in any ethnicity. Whereas, pathological calcifications have been described as extremely rare phenomena in patients with infectious diseases (e.g., tuberculosis, toxoplasmosis, cysticercosis), primary or metastatic brain tumors, autoimmune conditions like lupus erythematosus, certain developmental disorders and syndromes, endocrine disorders such as thyroid and parathyroid diseases and neuropsychiatric conditions with seizures or stroke [5, 6, 7]. Pathological calcifications/ ossifications could also be posttraumatic [8], or consequences of intracranial venous congestion [9]. According to a report on calcifications and ossification of the convexity of the falx cerebri and related subdural spaces; isolated dural calcification commonly affects the convexity of the cerebral dura mater, falx cerebri and the superior sagittal sinus [10]. This report, in addition to the above causes, also mentioned that intracranial calcifications/ossifications can be idiopathic, and can also be associated with vitamin-D intoxication or chronic renal failure [10]. It was also revealed that superior sagittal sinus calcifications occur in about 8% of the cases [11]. An earlier report of extensive falx cerebri ossification, incidentally found in patient with minor head injury, considered it as a normal anatomical variant [12].
Even though, most intracranial ossifications/calcifications including those in the dura mater and dural sinuses are considered as benign incidental findings during imaging investigations and dissections, they could have a mass effect of variable extent and they are also important in the differential diagnosis of calcified/ossified masses in the cranial cavity including calcified meningioma and hematoma [12], and foreign bodies in the cranial cavity following crash blast and gunshot injuries.
MATERIALS AND METHODS
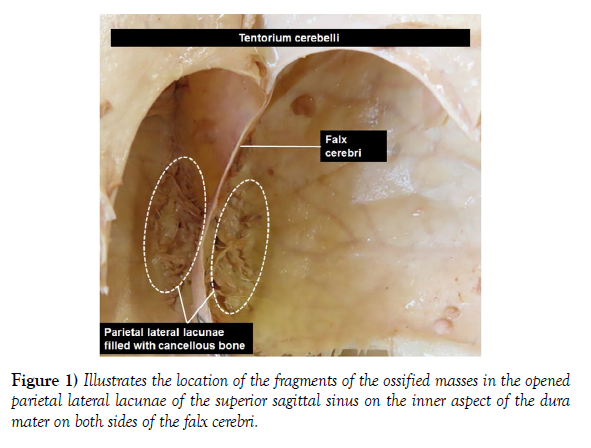
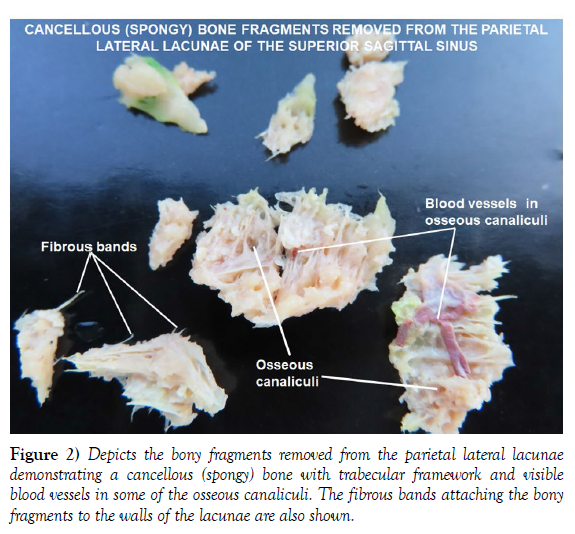
During opening of the head for the removal of the brain and meninges in a 93-year-old male cadaver, two hard irregular masses were incidentally palpated in the parietal lateral lacunae on both sides of the superior sagittal sinus. The dura mater was carefully removed and the lacunae were opened on the inside and fragments of the two masses were removed piece by piece. Photographs of the parietal lacunae and the fragments removed from the lacunae were taken for illustrations.
CASE REPORT
The opening of the parietal lateral lacunae on both sides of the superior sagittal sinus revealed two masses of vascularized bone, which were firmly and inseparably attached to the walls of the parietal lateral lacunae by fibrous bands (Figure 1). The observation of the fragmented pieces of the bony masses separated from the walls of the lacunae revealed a gross cancellous (spongy) bone appearance with a trabecular framework and multiple irregular osseous canaliculi traversed by blood vessels. In contrary to ordinary spongy bone, the osseous canaliculi in the fragments appeared clean and white with no red marrow or fat in them. There were no grossly observable pathological changes in the adjacent calvaria, brain, superior sagittal sinus or other blood vessels in the vicinity (Figure 2).
DISCUSSION
Frequent encounters of intracranial calcifications/ossifications involving the dura mater are well documented in many previous studies and report. These calcifications/ossifications can be physiological (age related), pathological or idiopathic. According to Deng H et al, when specific cause is not evident (idiopathic), a genetic etiology should be considered [1]. A study done on CT and MRI scans of 40 patients showed areas of ossification of variable shape in the falx cerebri consistent with a fatty marrow surrounded by a rim of cortical bone, the most common area of ossification being the frontal region of the falx cerebri. Such ossification is least frequently seen in the posterior part of the falx cerebri [2]. Falx cerebri ossification alone is usually not clinically significant, although sometimes it must be differentiated from calcified meningioma and interhemispheric vascular anomalies. Sometimes falx ossification is the site of metastases, leukemic infiltrations, myeloid metaplasia, osteosarcoma, chondroma, chondrosarcoma and giant cell tumors [2]. A CT scan study done on 365 cases also stated that falx cerebri calcification/ossification accounted for 34% of the cases and was slightly more frequent in older males [3]. Many other studies described that age related intracranial physiological calcifications/ossification occur in many parts of the brain and its meninges including the sagittal sinus and other blood vessels [4-7]. Pathological dural calcifications/ossifications can be caused by different diseases and trauma. This was supported by a case report that illustrated wide spread islets of eggshell-shaped bony tissue in the pericranium and dural mater detected during decompressive posttraumatic craniectomy that occurred in 6-year-old boy with a previous history of trauma to the head [8]. Intracranial ossification due to intracranial venous congestion associated with vascular malformations was also documented [9]. The report of Al-Motabagani M et al on two cadavers (one male and one female), demonstrated a calcified parietal emissary vein with ossification of the convex border of the falx cerebri and degenerated underlying brain tissue in the female cadaver, and a calcified upper convex border of the falx cerebri and superior sagittal sinus with no gross changes on the underlying brain tissue in the male cadaver [10]. Another retrospective study conducted on 107 CT scanned brains also noted superior sagittal sinus calcification with a slight preponderance of males over females (8% of females and 8.4% of males) [11]. The review and case report article on extensive falx cerebri ossification with no intracranial pathology considered it as normal anatomical variant and concluded that the proper nomenclature for such changes to be ossification not calcification [12]. Farther more, these authors also clearly noted that the terms like calcification and ossification are interchangeably used in most literature, though the distinction between the two can only be made on the basis of the presence or absence of bone tissue during histopathological examination [12]. The author of this current report could also observe that the term calcification is more frequently used than ossification. However, based on the gross appearance in the finding of this report that showed a trabecular bony framework pattern and its deposition in the lumen of the lacunae rather than in the wall, it seems to be more of ossification than calcification which is consistent with the previous report by Siedlecki Z et al 2020 [12].
Though intracranial calcifications/ossifications are frequently reported and considered as benign incidental findings during imaging investigations and dissections, with no pathological manifestation like in the present case, theoretically, I believe that they may have a mass effect of variable extent that can have pathological manifestations depending on size, location and how much wide spread they are. The presence of such ossification may also lead to occlusion of the lumina of the sinuses and associated lacunae impairing venous blood flow and CSF absorption; both of which could potentially cause increased intracranial pressure with brain congestion and edema. Such physiologic ossifications filling the lumina of the parietal lateral lacunae, that receive diploic and meningeal veins and the arachnoid granulation for CSF absorption can turn pathological and are, therefore, important in the differential diagnosis of calcified masses in the cranial cavity including but not limited to calcified meningioma and hematoma, and foreign bodies in the cranial cavity following crash, blast or gunshot injuries to the head.
No resource describing ossification similar to this, filling the lumen of parietal lateral lacunae associated with the superior sagittal sinus, could be found in search of literature. Therefore, I believe that this report is the first of its kind and since it is not associated with any grossly observable structural abnormality, it can be classified under the physiological (age related) ossifications.
CONCLUSION
Though most intracranial calcifications/ossification can be considered benign physiological conditions, such rare massive ossifications can likely cause compressive and degenerative changes leading to different neurological manifestations. Therefore, anatomists, pathologist, radiologist and neurosurgeons should be cognizant of such ossification in the parietal lateral lacunae of the superior sagittal sinus.
ACKNOWLEDGEMENT
I am thankful to the donor and his families for their invaluable donation and consent for education, research and publication. My most sincere and heartfelt thank goes to the department of biomedical sciences for the encouragement and uninterrupted support. I would also like to express my gratitude to Denelle Kees and John Opland for their immense assistance in the preparation of this cadaver for dissection in our gross anatomy lab.
REFERENCES
- Deng H, Zheng W, Jankovic J. Genetic and molecular biology of brain calcification. Ageing Res Rev. 2015; 22:20-38.
- Tsitouridis I, Natsis K, Goutsaridou F, Tsitouridis K, Tarazi L, et al. Falx cerebri ossification: CT and MRI evaluation. Neuroradiol. 2006; 19:621-628.
- Kiroglu Y, Calli C, Karabulut N, Oncel C. Intracranial calcifications on CT. Diagn Interv Radiol. 2010; 16:263-269.
- Schedler A, Deutschmann H. Falx cerebri calcifications and ossifications in CT scans- a data collection on frequency, position and size. 2019; 1(1):1-7.
- Bayrak S, Bulut DG, Cakmak ESK, Orhan K. Cone Beam computed tomographic evaluation of intracranial physiologic calcifications. J Craniofac surg. 2019; 30:510-513.
- Sedghizadeh PP, Nguyen M, Enciso R. Intracrenial physiological calcifications evaluated with cone beam CT. Dentomaxillofac Radiol. 2012; 41:675-678.
- Dos Santos Guedes M, Queiroz IC, de Castro CC. Classification and clinical significance of intracranial calcifications: a pictorial assay. Radiol Bras. 2020; 53(4):273-278.
- Guida L, Mazzoleni F, Bozzetti A, Sganzeria E, Giussani C, et al. Extensive dural ossification after decompressive posttraumatic craniectomy: Aa case report and review of literature. World Neurosurg. 2018; 120:59-62.
- Sankala HA, Hashim H. Intracranial calcification in venous congestion. Egypt J Radiol Nucl med. 2021; 52:181.
- Al-Motabagani M, Haroun H, Meguid EA. Calcification and ossification of the convexity of the falx cerebri and related subdural space in human cadavers. Neuroscience. 2004; 9(4):261-264.
- Krishna Kiran S, Braggs AV. Physiological intracranial calcifications- a study in coastal Karnataka. IJCMSR. 2020; 5(1):A95-A98.
- Siedlecki Z, Gromadzki B, Wozniak J, Jagodzinska K, Hadzik K, et al. Extensive ossification of falx cerebri- literature review based on own experience and case report. J Educ Health Sport. 2020; 10(8):365-371.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, CrossRef
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref