Mucormycosis in COVID-19 patients: A case series
Received: 15-Mar-2022, Manuscript No. PULJCMID-22-4488; Editor assigned: 18-Mar-2022, Pre QC No. PULJCMID-22-4488; Reviewed: 29-Mar-2022 QC No. PULJCMID-22-4488; Revised: 16-May-2022, Manuscript No. PULJCMID-22-4488; Published: 23-May-2022
Citation: Singhal A. Mucormycosis in COVID-19 patients: A case series. J Clin Microbiol Infect Dis 2022;5(4):30-32.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Mucormycosis is an opportunistic, potentially lethal, angioinvasive infection caused by many ribbon-like, broad, non-septate fungal elements of order Mucorales. Its predilection to blood vessels favors rapid and extensive spread to tissues and organs. Diabetes mellitus is the most common underlying risk factor followed up by group of patients with hematopoietic stem cells and solid organ transplant recipients on immunosuppressive therapy, Human Immunodeficiency Virus (HIV) infection, and patients on voriconazole therapy.
Keywords
Mucormycosis; COVID-19; Human Immunodeficiency Virus (HIV); aspergillosis
Introduction
Mucormycosis is an opportunistic, potentially lethal, angioinvasive infection caused by many ribbon-like, broad, non-septate fungal elements of order Mucorales [1]. Its predilection to blood vessels favors rapid and extensive spread to tissues and organs. Diabetes mellitus is the most common underlying risk factor followed up by group of patients with hematopoietic stem cells and solid organ transplant recipients on immunosuppressive therapy, Human Immunodeficiency Virus (HIV) infection, and patients on voriconazole therapy [2]. Rhino-Orbito Cerebral Mucormycosis (ROCM) is the most common type of clinical presentation in cases reported so far [3]. There has been an upsurge in the number of cases of mucormycosis during the second wave of COVID-19 pandemic which may be attributable to an increase in the indiscriminate usage of steroids. Other contributing factor may be increased ferritin/zinc levels. By and far, uncontrolled sugar levels have high probability of harboring systemic fungal co-infections and have identified invasive aspergillosis, candidiasis and mucormycosis as the causative organisms [4]. The mainstay of treatment is use of Amphotericin B and surgical debridement. Mucormycosis has been declared as a notifiable disease in various states of India. Indian Council of Medical Research (ICMR) advisory issued on 10.05.2021, say that mucormycosis if uncared for, may turn fatal [5].
Case Presentation
Case 1
A 43 years old man was admitted to the ENT department at a tertiary care hospital, Gurugram, India. He presented with epistaxis from both nostrils and headache since 3 days for which he got investigated and was suspected to have fungal elements in nasal cavity. The patient is a known case of chronic kidney disease and was treated for COVID infection few days back from previous hospital. The patient had a past history of hypertension since 10 years for which he is taking medication. On physical examination, nasal cavity crusting was noted in both the nares. Laboratory investigations were suggestive of anemia, leukocytosis, and dyselectrolytemia, raised serum creatinine and raised inflammatory markers. 2D Echo was s/o concentric left ventricular hypertrophy and normal Left Ventricle (LV) systolic function, Left Ventricle Ejection Fraction (LVEF) 55% and Grade 1 LV diastolic dysfunction. Ultrasonography KUB was s/o bilateral polycystic kidneys. Hemodialysis was done in view of ascites. Magnetic Resonance Imaging (MRI) face and brain reported diffuse mucosal thickening with evidence of focal areas of T2 shortening in the left maxillary and ethmoidal sinuses and left middle turbinate with edema in the adjacent periantral fat plane, pterygopalatine fossa, masticator space and extraconal left orbit s/o invasive fungal sinusitis (Mucormycosis). Endoscopic nasal debridement was done involving left sphenopalatine region, left eustachian tube region and nasoharynx. Sample sent for KOH revealed broad, aseptate ribbon like hyphae s/o mucormycosis (Figure 1).
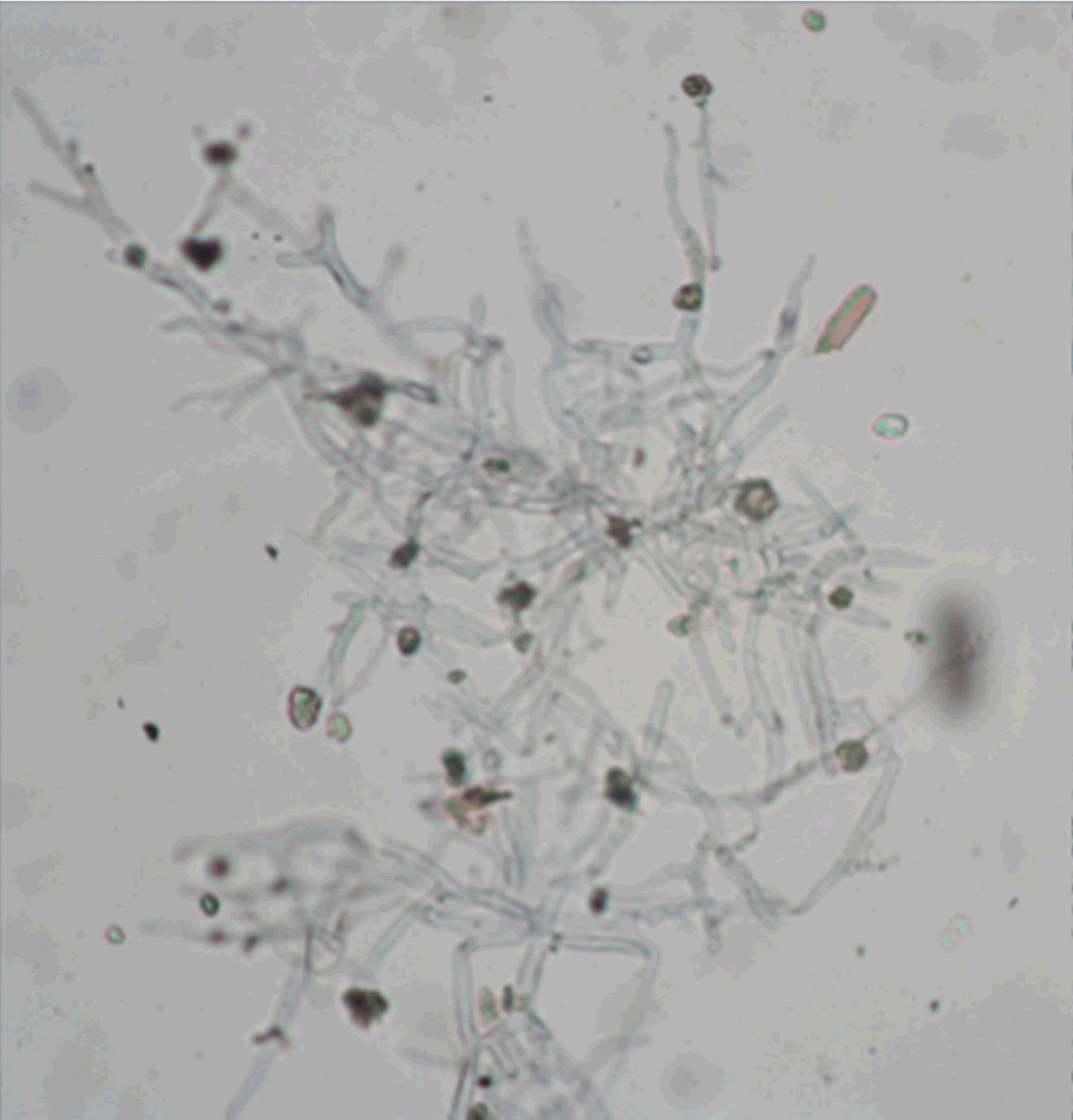
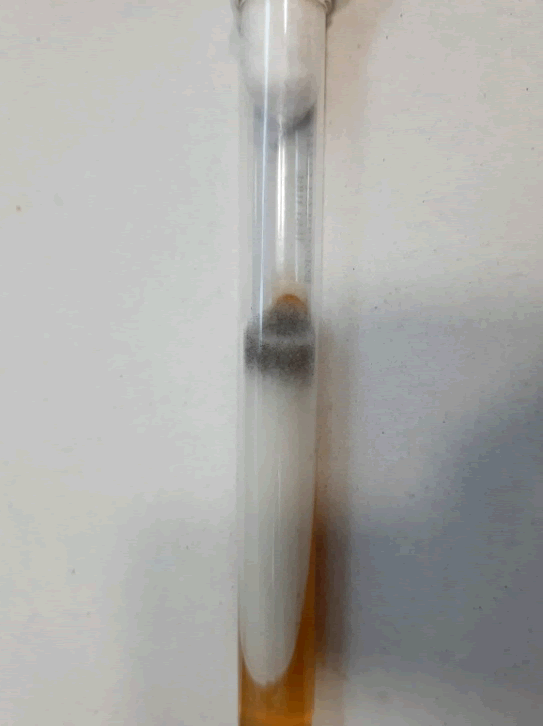
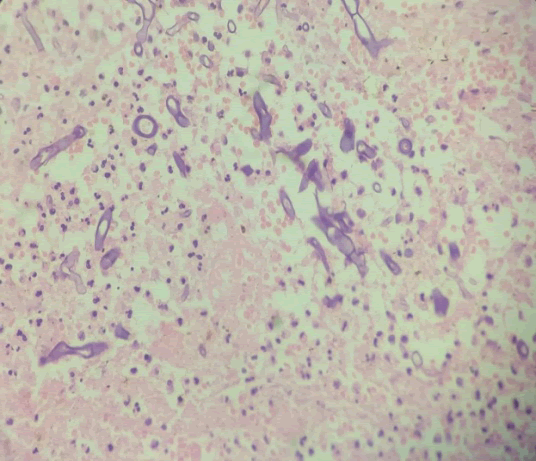
Histopathology (HPE) report showed zygomycotic infection (Mucormycosis). Fungal culture and Lactophenol Cotton Blue (LPCB) stain findings were consistent with mucor species (Figures 2 and 3). Accordingly Injection Liposomal Amphoterecin B was given with nephrology review. Blood transfusion was done and cycles of hemodialysis were planned accordingly. Regular ENT review was put on board. Pus c/s showed growth of Escherichia coli and Staphylococcus aureus. Repeat MRI Paranasal Sinus (PNS) contrast was s/o post-operative changes in bilateral nasal fossae and bilateral maxillary sinuses with polypoidal mucosal thickening in bilateral fronto-ethmoidal air cells and sphenoid sinuses. Ophthalmological consultation was done and advice followed. Currently he is hemodynamically stable and hence discharged with follow up advice.
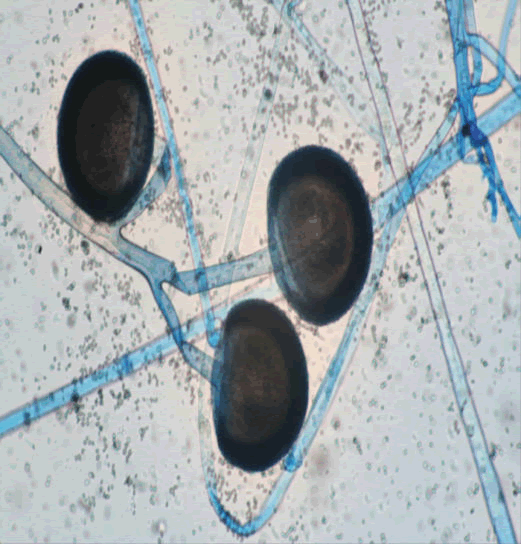
A 40 year old female presented with complaints of unilateral facial pain, heaviness and numbness accompanied by watering of the eye since 6 days. She had past history of COVID-19 infection 3 weeks back. Along with it she was freshly diagnosed as diabetic with HbA1c 10.1. The patient is also a known case of hypertension. After complete recovery of her previous ailment she got readmitted with the above complaints at a tertiary care hospital, Gurugram, India. On physical examination, left maxillary region bogginess was noted on the face. The patient vitals were stable with maintenance of spO2 95% on room air, however random blood sugar levels were 289 mg/dl. Her initial investigations revealed deranged kidney function test and low Haemoglobin. Left nasal crust sent for KOH mount revealed broad, aseptate fungal hyphae s/o mucormycosis. HPE findings showed fungal colonization consistent with mucormycosis (Figure 4).
Left nasal pus c/s showed mixed growth of Klebsiella pneumoniae and Pseudomonas Aeruginosa. MRI Face+Brain showed post op changes with residual mucosa thickening with evidence of focal T2 shortening in the left maxillary sinus with edema and enhancement in the adjacent periantral fat plane, pterygopalantine fossa, masticator space and extraconal left orbit suggestive of invasive fungal sinusitis also in sphenoid sinus with asymmetrical prominence of left cavernous sinus and dural enhancement along left temporal lobe, no neuroparenchymal involvement seen. She was managed with Liposomal Amphotericin B along with Intravenous (IV) Antibiotics, IV fluids with electrolyte correction, Insulin according to blood sugar level and other supportive medications. With socio-psychological support and glycemic control at home, patient was instructed to follow diabetic diet chart plan. The patient was discharged in a stable condition and with a follow up advice.
Case 3
A 43 years old male patient presented with complaints of pain and swelling in the left eye since 2-3 days. He is a known case of Type 2 Diabetes mellitus since 7 years and had been on steroids for COVID-19 disease recently. He was admitted under neurosurgery team with the above mentioned complaints and was thoroughly investigated. Based on the findings from history, clinical examination and imaging studies, patient was diagnosed with rhino-orbital mucormycosis. Endoscopic nasal debridement was suggestive of Deviated Nasal Septum (DNS) to left, minimal crust in bilateral middle turbinate, left bulla ethmoidalis and ethmoid sinus appears unhealthy and pale. Fungal debris was seen near left optic recess following which left side eye exenteration was done. HPE findings reported fungal colonization suggestive of mucormycosis. Patient was started on systemic antifungals. Relook nasal endoscopy after few days showed presence of fungal ball in left ethmoidal region and left lamina which appeared black and unhealthy. It was partly removed and sent for HPE examination. MRI brain with contrast s/o bulky left cavernous sinus with left basifrontal abscess for which neurology opinion was taken and advice followed. Patient continued to have hypokalemia despite corrective measures. In addition patient started developing thrombocytopenia hence was shifted to Intensive Care Unit (ICU) in view of intracranial abscess. Patient tolerated surgery well and was shifted to neurosurgery ICU. Patient was kept on multiple inotropic supports in view of hypertension. Blood culture and sensitivity was suggestive of Multidrug Resistant (MDR) Escherichia coli. Sputum culture and sensitivity reported mixed growth of gram negative bacilli. Antibiotics were modified for the same. Patient was kept under close observation and monitoring. Nephrology opinion was taken in view of persistent hypokalemia and hematology department review was taken for persistent thrombocytopenia. The patient was discharged in a stable condition after a week.
Discussion
Mucormycosis is an opportunistic, angioinvasive disease which may prove fatal if timely diagnosis and treatment are not given. The exact incidence of mucormycosis in India is unknown due to lack of population based studies. Estimated prevalence of mucormycosis is around 70 times higher in India than globally [3]. Several genera are associated with this disease, namely Rhizopus, Rhizo-mucor, Absidia in descending order of their prevalence. Rhino-Orbital-Cerebral (ROCM) is the most common clinical presentation followed by pulmonary, gastrointestinal, cutaneous renal and disseminated mucomycosis [6]. Rhinocerebral mucormycosis is the most common and fulminating type of mucormycosis, which may lead to fatal consequences. Most common underlying predisposing factor is Diabetes ketoacidosis, neutropenia, steroid and deferoxamine therapy. The fungus spreads by inhalation of affected mold spores in the air via nasal mucosa to turbinate bones, paranasal sinuses, orbit and palate with extension to the brain where massive invasion to blood vessels causes major infarct. Clinical presentation can be diverse. The most common symptoms include facial swelling and pain, headache, nasal or sinus congestion. Physical examination reveals brownish, blood stained nasal discharge, black eschar on palate, tissue necrosis, fixed and dilated pupil, proposes, ptosis and visual loss in later stages. Infection may disseminate to lungs and other organs. The host immune response to the virus triggers hyperactive immune response in the host resulting in an excessive inflammatory reaction in the form of 'cytokine storm' eventually leading to multi-organ failure in severe COVID-19 infection [7]. Management of rhino cerebral mucormycosis requires surgical sino-nasal drainage and debridement of orbital or cerebral disease, combined with a prolonged course of intravenous antifungal therapy. The limits of debridement will depend on the extent of invasion. First line medical treatment consists of IV Amphotericin-based antifungals, with a course of at least 6 weeks duration. Liposomal formulations of Amphotericin B have proven efficacy and safety [8]. In case of failure, second-line antifungals such as IV posaconazole can be tried as salvage therapy [9]. In histological examination of the tissue involved by mucormycosis, show varying amounts of necrosis which is infiltrated by higher number of fungal organisms. These fungal elements show ribbon-like, broad aseptate hyphae which marks a hallmark for zygomycetes group of fungi. Special stains for fungus along with culture from necrotic areas confirm the diagnosis. The histopathology report along with microbiological culture evidence confirms with the clinical diagnosis.
Conclusion
Mucormycosis is increasingly emerging fungal infection with a formidable mortality rate. Studies suggest the infection usually happens 3-42 days after the onset of COVID-19 [10]. Hence, the clinician must be aware of every possibility of fungal infection in an immunocompromised diabetic patient along with co morbid conditions and steroid therapy. Blood sugar should be restored to normal level as early as possible. Once suspected, diagnosis is not very difficult thereby immediately treatment may be instituted in form of surgical debridement as well as antifungal regimen.
References
- Honavar SG. Code Mucor: Guidelines for the Diagnosis, Staging and Management of Rhino-Orbito-Cerebral Mucormycosis in the Setting of COVID-19. Ind J Ophthalmol. 2021;69(6):1361-5.
- Skiada A, Floerl C L, Klimko N, et al. Challenges in the diagnosis and treatment of mucormycosis. Medical Mycology. 2018;56(1):93–101.
- Prakash H, Chakrabarti A. Epidemiology of mucormycosis in India. Microorganisms. 2021;9:523.
- Amalanathan S, Colbert K R, Chockalingam SK. Mucormycosis complicating diabetes mellitus and COVID-19: a diagnostic and therapeutic threat. Int J Otorhinolaryngol Head Neck Surg. 2021;7(4):679-82.
- Cornely OA, Izquierdo AA, Arenz D, et al. Global guideline for the diagnosis and management of mucormycosis:an initiative of the European Confederation of Medical Mycology incooperation with the Mycoses Study Group Education and Research Consortium. Lancet Infect Dis. 2019;19(12):e405-e21.
- Auluck A. Maxillary necrosis by mucormycosis. A case report and literature review. Med Oral Patol Oral Cir Bucal. 2007;12(5):360-64.
- Shamsudeen M, Hameed C P, Paul L, et al. Asymptomatic COVID 19 infection: An innocent bystander in Mucormycosis or maybe not? Indian J Microbiol Res. 2021;8(2):182–84.
[Crossref]
- Kontoyiannis DP, Lewis RE. How I treat mucormycosis. Blood. 2011;118(12):16-24.
- Almannai M, Imran H, Estrada B et al. Successful treatment of rhino-orbital mucormycosis with posaconazole and hyperbaric oxygen therapy. Pediatr Hematol Oncol. 2013,30(3):184-86.
- Sen M, Lahane S, Lahane TP, et al. Mucor in a Viral Land: A Tale of Two Pathogens. Indian J Ophthalmol. 2021;69(2):244-52.