Right congenital pleuro-peritoneal hiatus hernia
Devi Sankar K*, Sharmila Bhanu P, Susan PJ, Gajendra K
Department of Anatomy, Narayana Medical College, Chinthareddy Palem, Nellore, Andhra Pradesh, India.
- *Corresponding Author:
- Devi Sankar K, MSc
Assistant Professor, Department of Anatomy, Narayana Medical College, Chinthareddy Palem, Nellore, Andhra Pradesh, 524 002, India.
Tel: +91 949 0948006
E-mail: lesanshar@gmail.com
Date of Received: July 15th, 2009
Date of Accepted: December 25th, 2009
Published Online: December 31st, 2009
© IJAV. 2009; 2: 153–155.
[ft_below_content] =>Keywords
diaphragmatic hernia, unilateral congenital diaphragmatic hernia, mediastinal shift, dextrocardia, pulmonary hypoplasia
Introduction
Congenital diaphragmatic hernia (CDH) is the herniation of abdominal contents into the thoracic cavity due to the defect in the diaphragm. CDH occurs 1 in every 2000-4000 live births and accounts for 8% of all major congenital anomalies [1]. CDH is a life-threatening malformation believed to be the consequence of failure of closure of the pleuropenitoneal canal which is usually unilateral most frequently seen on left side. Very rarely diaphragmatic hernia occurs bilaterally [2]. We report a case of unilateral congenital right diaphragmatic hernia (CRDH) with left mediastinal shift. The fetus with CRDH was in no danger until birth but died shortly after birth due to respiratory distress [3].
In human, CRDH are approximately five times less common than those on the left. Defects of the right diaphragm, although surgically and anatomically similar to those on the left, are more inconspicuous in presentation. Because the symptoms of the former are less severe, however, they tend to be diagnosed later. Some are asymptomatic and go unrecognized through life [4].
Case Report
A 36-year-old pregnant woman from a nearby village was admitted in maternity ward of Narayana General Hospital, Nellore. The prenatal ultrasonographic findings at 36th week of gestation showed CRDH. A single male infant weighing 2,572 grams was delivered vaginally at 38 weeks of gestation after spontaneous labor. The infant developed severe respiratory distress immediately after birth and died 2 hour of age despite intensive resuscitation. With the parent’s written consent, the dead infant was sent to anatomy department museum, Narayana Medical College, Nellore. The infant was injected and immersed in routine formalin and allowed for fixation. The infant’s chest and abdominal wall was incised and opened carefully. Chest cavity showed mediastinal shift towards left side.
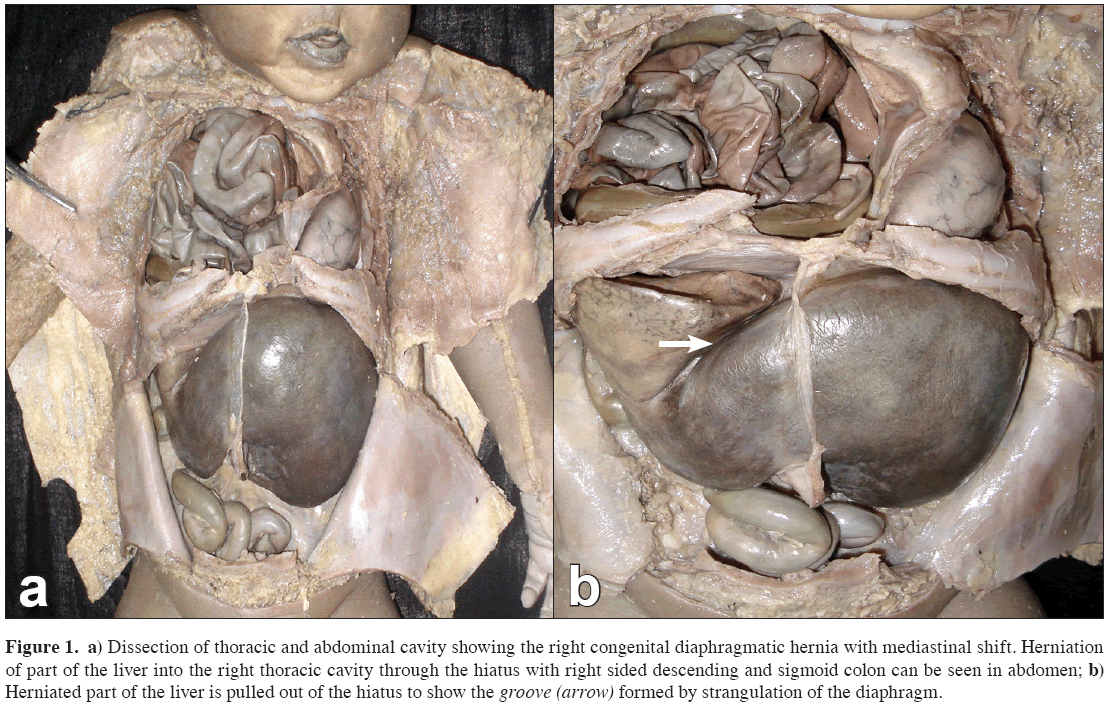
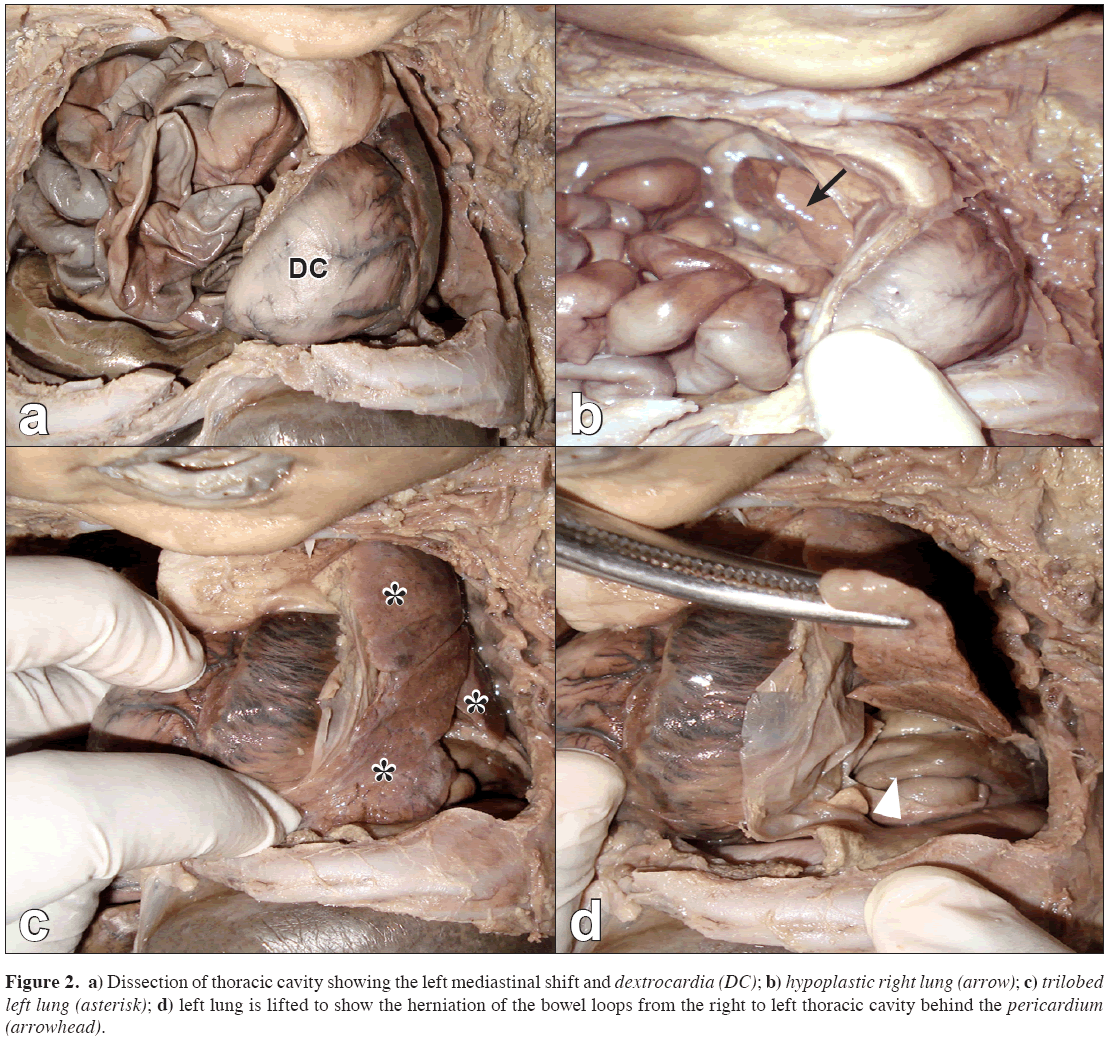
A large defect was found in the right side of the diaphragm, confirming the CRDH. All parts of the gastrointestinal system including a part of the right lobe of liver were herniated first into the right side and then left pleural cavities behind the pericardium. Only a small portion of the gastrointestinal system (most of the liver, right sided descending and sigmoid colon) and urinary organs were seen in the abdominal cavity. There was a complete absence of spleen. The right pleural cavity showed severe hypoplasia of right lung. In addition, the thoracic cavity showed trilobed left lung and dextrocardia (Figures 1, 2).
Figure 1: a) Dissection of thoracic and abdominal cavity showing the right congenital diaphragmatic hernia with mediastinal shift. Herniation of part of the liver into the right thoracic cavity through the hiatus with right sided descending and sigmoid colon can be seen in abdomen; b) Herniated part of the liver is pulled out of the hiatus to show the groove (arrow) formed by strangulation of the diaphragm.
Figure 2: a) Dissection of thoracic cavity showing the left mediastinal shift and dextrocardia (DC); b) hypoplastic right lung (arrow); c) trilobed left lung (asterisk); d) left lung is lifted to show the herniation of the bowel loops from the right to left thoracic cavity behind the pericardium (arrowhead).
Discussion
Congenital diaphragmatic hernias seen in the fetal and newborn are due to large defect or complete absence of the diaphragm and have many problems in diagnosis and treatment [5]. The defects are usually unilateral and 75% of cases were found to be left CDH. Bilateral hernias are rare and found in only 2% of cases [6]. Although the CDH usually presents during neonatal period, 13% of cases may be found in the later periods, the approximate age being 16-18 years [7].
The pleuroperitoneal canals close during 10 week of intrauterine life which allow fetal diaphragm to separate the thoracic and abdominal cavities. Physiologically herniated fetal gut has to return into the abdominal cavity by 10-12 weeks which when the diaphragm is not closed, moves into the chest cavity resulting in CDH frequently seen on the left side. [8].
This type of hernias occur during the development due to the lack of fusion of pleuropenitoneal membrane with septum transversum which results in the congenital communication between the peritoneal and thoracic cavities, often seen on the left side [9]. The opening is usually triangular or elliptical in shape which may be within the diaphragmatic muscle or with a complete absence of posterolateral part of the muscle. The abdominal viscera usually involved in this type of hernia are caecum, appendix, ascending colon, transverse colon and all parts of small intestine and sometimes spleen also may be involved. The stomach is usually seen in the abdomen [10,11]. The herniated viscera compresses the developing lung tissue and lead to pulmonary hypoplasia on contralateral sides because of the mediastinal shift which reduces the number of bronchial generations results in hypoplastic lungs [7,12].
In our case, a large elliptical opening was found in the right side of the diaphragm which is a pleuropenitoneal hiatus. Except the liver, descending and sigmoid colon and the urinary organs, all the abdominal viscera are herniated into the thoracic cavity. In pleuropenitoneal hiatus hernia usually the stomach is retained in the abdominal cavity [11]; but in our case, whole of the stomach was herniated. In addition, part of the right lobe of the liver also was herniated with strangulation formed by the band of diaphragmatic muscle forming a groove on its anterior surface. The left lobe was markedly enlarged. Another striking feature in our case is that there was a complete absence of spleen. The thoracic cavity showed severe hypoplasia of right lung, trilobed left lung and dextrocardiac heart with its apex directed towards the right side.
Pulmonary hypoplasia and hypertension may be the reasons of high mortality rate at birth. The dysfunction of surfactant system combined with cardiac malformations may further complicate the conditions of congenital diaphragmatic hernia [1,13]. The hypoplasia of the right lung may be the reason for the respiratory distress which would have lead to the death of the baby in our case. The agenesis of spleen observed in our case may be associated with congenital malformations of heart and sometimes instead of spleen the other organs like kidneys may also be absent [14].
The occurrence of CRDH associated with other anomalies like gastrointestinal, cardiac and abdominal wall defects which can be diagnosed prenatally, allows the evaluation of fetal life after the birth. The definitive diagnosis of this type of hernias can be demonstrated by the degree of displacement of abdominal organs into the thoracic cavities, by ultrasonographic examinations. Knowledge of this right diaphragmatic hernia during the prenatal and antenatal periods may assure for its management and surgical corrections which can help to reduce the mortality rate.
References
- Adzick NS, Harrison MR, Glick PL, Nakayama DK, Manning FA, de Lorimier AA. Diaphragmatic hernia in fetus: prenatal diagnosis and outcome in 94 cases. J Pediatr Surg. 1985; 20: 357–361.
- Furuta Y, Nakamura Y, Miyamoto K. Bilateral congenital posterolateral diaphragmatic hernia. J Pediatr Surg. 1987; 22: 182–183.
- Nakayama DK, Harrison MR, Chinn DH, Callen PW, Filly RA, Golbus MS, De Lorimier AA. Prenatal diagnosis and natural history of the fetus with a congenital diaphragmatic hernia: initial clinical experience. J Pediatr Surg. 1985; 20: 118–124.
- Stahl GE, Warren WS, Rosenberg H, Spackman TJ, Schnaufer L. Congenital right diaphragmatic hernia. A case report and review of the literature. Clin Pediatr (Phila). 1981; 20: 422–425.
- Song MS, Yoo SJ, Smallhorn JF, Mullen JB, Ryan G, Hornberger LK. Bilateral congenital diaphragmatic hernia: diagnostic clues at fetal sonography. Ultrasound Obstet Gynecol. 2001; 17: 255–258.
- Kufeji DI, Crabbe DC. Familial bilateral congenital diaphragmatic hernia. Pediatr Surg Int. 1999; 15: 58–60.
- Chetan G, Sreerag KS, Rathisharmila R, Barath J, Narayanan P, Jagdish S, Bhat VB. Unusual case of congenital diaphragmatic hernia – a case report. Curr Pediatr Res. 2008; 12: 5–7.
- Hamilton WJ, Mossman HW. Human embryology. 4th Ed., Cambridge, MacMillan Press Ltd. 1972; 356–361, 367–372.
- Levin DL. Morphologic analysis of the pulmonary vascular bed in congenital left-sided diaphragmatic hernia. J Pediatr. 1978; 92: 805–809.
- Harrington SW. Diaphragmatic hernia of children. Ann Surg. 1942; 115: 705–715.
- McGuigan R, Azarow KS. Living on the edge: current concepts in the management of congenital diaphragmatic hernia. Curr Surg. 2005; 62: 390–395.
- Adzick NS, Vacanti JP, Lillehei CW, O’Rourke PP, Crone RK, Wilson JM. Fetal diaphragmatic hernia: ultrasound diagnosis and clinical outcome in 38 cases. J Pediatr Surg. 1989; 24: 654–657.
- Phatak SV, Ghodke K. Antenatal diagnosis of congenital diaphragmatic hernia: a case report. Ind J Radiol Imag. 2006; 16: 793–795.
- Hu CH. Congenital malformation of heart with anomalous insertion of pulmonary veins, absence of spleen, situs inversus of abdominal viscera and other developmental errors. Am J Pathol. 1929; 5: 389–396.7.
Devi Sankar K*, Sharmila Bhanu P, Susan PJ, Gajendra K
Department of Anatomy, Narayana Medical College, Chinthareddy Palem, Nellore, Andhra Pradesh, India.
- *Corresponding Author:
- Devi Sankar K, MSc
Assistant Professor, Department of Anatomy, Narayana Medical College, Chinthareddy Palem, Nellore, Andhra Pradesh, 524 002, India.
Tel: +91 949 0948006
E-mail: lesanshar@gmail.com
Date of Received: July 15th, 2009
Date of Accepted: December 25th, 2009
Published Online: December 31st, 2009
© IJAV. 2009; 2: 153–155.
Abstract
be encountered in any period of life. Left mediastinal shift with right congenital diaphragmatic hernia is rare and life threatening malformation. We describe a case of right congenital diaphragmatic hernia of a newborn male infant, which died shortly after birth. The lobes of the liver were enlarged and occupied whole of the abdominal cavity. The stomach and intestinal loops were herniated into the right pleural cavity and partly into the left pleural cavity. Severe hypoplastic right lung, trilobed left lung and dextrocardia also were observed.
-Keywords
diaphragmatic hernia, unilateral congenital diaphragmatic hernia, mediastinal shift, dextrocardia, pulmonary hypoplasia
Introduction
Congenital diaphragmatic hernia (CDH) is the herniation of abdominal contents into the thoracic cavity due to the defect in the diaphragm. CDH occurs 1 in every 2000-4000 live births and accounts for 8% of all major congenital anomalies [1]. CDH is a life-threatening malformation believed to be the consequence of failure of closure of the pleuropenitoneal canal which is usually unilateral most frequently seen on left side. Very rarely diaphragmatic hernia occurs bilaterally [2]. We report a case of unilateral congenital right diaphragmatic hernia (CRDH) with left mediastinal shift. The fetus with CRDH was in no danger until birth but died shortly after birth due to respiratory distress [3].
In human, CRDH are approximately five times less common than those on the left. Defects of the right diaphragm, although surgically and anatomically similar to those on the left, are more inconspicuous in presentation. Because the symptoms of the former are less severe, however, they tend to be diagnosed later. Some are asymptomatic and go unrecognized through life [4].
Case Report
A 36-year-old pregnant woman from a nearby village was admitted in maternity ward of Narayana General Hospital, Nellore. The prenatal ultrasonographic findings at 36th week of gestation showed CRDH. A single male infant weighing 2,572 grams was delivered vaginally at 38 weeks of gestation after spontaneous labor. The infant developed severe respiratory distress immediately after birth and died 2 hour of age despite intensive resuscitation. With the parent’s written consent, the dead infant was sent to anatomy department museum, Narayana Medical College, Nellore. The infant was injected and immersed in routine formalin and allowed for fixation. The infant’s chest and abdominal wall was incised and opened carefully. Chest cavity showed mediastinal shift towards left side.
A large defect was found in the right side of the diaphragm, confirming the CRDH. All parts of the gastrointestinal system including a part of the right lobe of liver were herniated first into the right side and then left pleural cavities behind the pericardium. Only a small portion of the gastrointestinal system (most of the liver, right sided descending and sigmoid colon) and urinary organs were seen in the abdominal cavity. There was a complete absence of spleen. The right pleural cavity showed severe hypoplasia of right lung. In addition, the thoracic cavity showed trilobed left lung and dextrocardia (Figures 1, 2).
Figure 1: a) Dissection of thoracic and abdominal cavity showing the right congenital diaphragmatic hernia with mediastinal shift. Herniation of part of the liver into the right thoracic cavity through the hiatus with right sided descending and sigmoid colon can be seen in abdomen; b) Herniated part of the liver is pulled out of the hiatus to show the groove (arrow) formed by strangulation of the diaphragm.
Figure 2: a) Dissection of thoracic cavity showing the left mediastinal shift and dextrocardia (DC); b) hypoplastic right lung (arrow); c) trilobed left lung (asterisk); d) left lung is lifted to show the herniation of the bowel loops from the right to left thoracic cavity behind the pericardium (arrowhead).
Discussion
Congenital diaphragmatic hernias seen in the fetal and newborn are due to large defect or complete absence of the diaphragm and have many problems in diagnosis and treatment [5]. The defects are usually unilateral and 75% of cases were found to be left CDH. Bilateral hernias are rare and found in only 2% of cases [6]. Although the CDH usually presents during neonatal period, 13% of cases may be found in the later periods, the approximate age being 16-18 years [7].
The pleuroperitoneal canals close during 10 week of intrauterine life which allow fetal diaphragm to separate the thoracic and abdominal cavities. Physiologically herniated fetal gut has to return into the abdominal cavity by 10-12 weeks which when the diaphragm is not closed, moves into the chest cavity resulting in CDH frequently seen on the left side. [8].
This type of hernias occur during the development due to the lack of fusion of pleuropenitoneal membrane with septum transversum which results in the congenital communication between the peritoneal and thoracic cavities, often seen on the left side [9]. The opening is usually triangular or elliptical in shape which may be within the diaphragmatic muscle or with a complete absence of posterolateral part of the muscle. The abdominal viscera usually involved in this type of hernia are caecum, appendix, ascending colon, transverse colon and all parts of small intestine and sometimes spleen also may be involved. The stomach is usually seen in the abdomen [10,11]. The herniated viscera compresses the developing lung tissue and lead to pulmonary hypoplasia on contralateral sides because of the mediastinal shift which reduces the number of bronchial generations results in hypoplastic lungs [7,12].
In our case, a large elliptical opening was found in the right side of the diaphragm which is a pleuropenitoneal hiatus. Except the liver, descending and sigmoid colon and the urinary organs, all the abdominal viscera are herniated into the thoracic cavity. In pleuropenitoneal hiatus hernia usually the stomach is retained in the abdominal cavity [11]; but in our case, whole of the stomach was herniated. In addition, part of the right lobe of the liver also was herniated with strangulation formed by the band of diaphragmatic muscle forming a groove on its anterior surface. The left lobe was markedly enlarged. Another striking feature in our case is that there was a complete absence of spleen. The thoracic cavity showed severe hypoplasia of right lung, trilobed left lung and dextrocardiac heart with its apex directed towards the right side.
Pulmonary hypoplasia and hypertension may be the reasons of high mortality rate at birth. The dysfunction of surfactant system combined with cardiac malformations may further complicate the conditions of congenital diaphragmatic hernia [1,13]. The hypoplasia of the right lung may be the reason for the respiratory distress which would have lead to the death of the baby in our case. The agenesis of spleen observed in our case may be associated with congenital malformations of heart and sometimes instead of spleen the other organs like kidneys may also be absent [14].
The occurrence of CRDH associated with other anomalies like gastrointestinal, cardiac and abdominal wall defects which can be diagnosed prenatally, allows the evaluation of fetal life after the birth. The definitive diagnosis of this type of hernias can be demonstrated by the degree of displacement of abdominal organs into the thoracic cavities, by ultrasonographic examinations. Knowledge of this right diaphragmatic hernia during the prenatal and antenatal periods may assure for its management and surgical corrections which can help to reduce the mortality rate.
References
- Adzick NS, Harrison MR, Glick PL, Nakayama DK, Manning FA, de Lorimier AA. Diaphragmatic hernia in fetus: prenatal diagnosis and outcome in 94 cases. J Pediatr Surg. 1985; 20: 357–361.
- Furuta Y, Nakamura Y, Miyamoto K. Bilateral congenital posterolateral diaphragmatic hernia. J Pediatr Surg. 1987; 22: 182–183.
- Nakayama DK, Harrison MR, Chinn DH, Callen PW, Filly RA, Golbus MS, De Lorimier AA. Prenatal diagnosis and natural history of the fetus with a congenital diaphragmatic hernia: initial clinical experience. J Pediatr Surg. 1985; 20: 118–124.
- Stahl GE, Warren WS, Rosenberg H, Spackman TJ, Schnaufer L. Congenital right diaphragmatic hernia. A case report and review of the literature. Clin Pediatr (Phila). 1981; 20: 422–425.
- Song MS, Yoo SJ, Smallhorn JF, Mullen JB, Ryan G, Hornberger LK. Bilateral congenital diaphragmatic hernia: diagnostic clues at fetal sonography. Ultrasound Obstet Gynecol. 2001; 17: 255–258.
- Kufeji DI, Crabbe DC. Familial bilateral congenital diaphragmatic hernia. Pediatr Surg Int. 1999; 15: 58–60.
- Chetan G, Sreerag KS, Rathisharmila R, Barath J, Narayanan P, Jagdish S, Bhat VB. Unusual case of congenital diaphragmatic hernia – a case report. Curr Pediatr Res. 2008; 12: 5–7.
- Hamilton WJ, Mossman HW. Human embryology. 4th Ed., Cambridge, MacMillan Press Ltd. 1972; 356–361, 367–372.
- Levin DL. Morphologic analysis of the pulmonary vascular bed in congenital left-sided diaphragmatic hernia. J Pediatr. 1978; 92: 805–809.
- Harrington SW. Diaphragmatic hernia of children. Ann Surg. 1942; 115: 705–715.
- McGuigan R, Azarow KS. Living on the edge: current concepts in the management of congenital diaphragmatic hernia. Curr Surg. 2005; 62: 390–395.
- Adzick NS, Vacanti JP, Lillehei CW, O’Rourke PP, Crone RK, Wilson JM. Fetal diaphragmatic hernia: ultrasound diagnosis and clinical outcome in 38 cases. J Pediatr Surg. 1989; 24: 654–657.
- Phatak SV, Ghodke K. Antenatal diagnosis of congenital diaphragmatic hernia: a case report. Ind J Radiol Imag. 2006; 16: 793–795.
- Hu CH. Congenital malformation of heart with anomalous insertion of pulmonary veins, absence of spleen, situs inversus of abdominal viscera and other developmental errors. Am J Pathol. 1929; 5: 389–396.7.