Unusual skin lesions in a patient with renal amyloidosis unmasked by nephrotic syndrome: A case report
2 Department of Pathology, Iran University of Medical Sciences, Tehran, Iran
3 Department of Pediatric Nephrology, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Received: 19-Jan-2022, Manuscript No. PULCNR-22-5501; Editor assigned: 21-Jan-2022, Pre QC No. PULCNR-22-5501 (PQ); Accepted Date: Jan 22, 2024; Reviewed: 25-Jan-2024 QC No. PULCNR-24-5501; Revised: 19-Jan-2024, Manuscript No. PULCNR-24-5501 (R); Published: 30-Jan-2024
Citation: Honarpisheh P, Akbari H, Mehrazma M et al. Unusual skin lesions in a patient with renal amyloidosis unmasked by nephrotic syndrome: A case report. Clin Nephrol Res 2023;7(1):1-2.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Primary systemic amyloidosis is a rare disease caused by abnormal deposition of amyloid protein in different organ systems and mainly involves the kidneys, heart, peripheral nerves, and liver. The kidney is one of the most frequently affected organs in systemic amyloidosis which typically presents with nephrotic syndrome. Cutaneous involvement in amyloidosis can occur as a skin limited disorder or as a manifestation of systemic amyloidosis. Various cutaneous lesions can be seen in systemic amyloidosis, especially in form of petechial, purpura, and ecchymosis. Nail dystrophy and bolus skin lesions are the rare manifestations of systemic amyloidosis. In this case, we report an Iranian 64 years old man with bolus skin lesions and nail dystrophy associated with systemic amyloidosis.
Keywords
Systemic amyloidosis; Nephrotic syndrome; Cutaneous amyloidosis; Nail dystrophy; Ecchymosis
Introduction
Amyloidosis is a disease caused by the extracellular deposition of insoluble misfold polymeric protein fibrils in tissues and organs. Amyloidosis is classified as localized or systemic forms depending on amyloid deposition in one or multiple organs respectively. Systemic amyloidosis is categorized into 18 different types which most clinically important types are primary amyloidosis (amyloidosis associated with light chain (AL amyloidosis)), secondary amyloidosis (apolipoprotein serum amyloid A (AA amyloidosis)), Amyloidosis Associated with Transthyretin (ATTR), and hemodialysis associated amyloidosis [1,2].
Almost all organ systems can be affected by amyloidosis leading to organ dysfunction [3]. Renal involvement as a part of primary systemic amyloidosis is not uncommon with an overall prevalence of 1.6% [4]. Nail lesions also can be seen in systemic amyloidosis and may be the first manifestation of systemic amyloidosis [5]. Skin manifestations in the form of bullous lesions are rare in amyloidosis and mimic bullous pemphigoid [6]. Here we describe a case of AL amyloidosis presenting bullous skin lesions and nail dystrophy unmasked by nephrotic syndrome 8 months later.
Case Presentation
A 64 years old white man was admitted to our hospital with generalized edema. He did not report any constitutional, musculoskeletal, gastrointestinal, or neurological symptoms. He also noticed bullous skin lesions and painful tip fingers with deformed nails from 8 months ago, without any other signs and symptoms. He has no past medical history of diabetes mellitus and chronic diseases such as tuberculosis, hepatitis, or chronic bronchitis. There was no history of taking drugs or herbal substances.
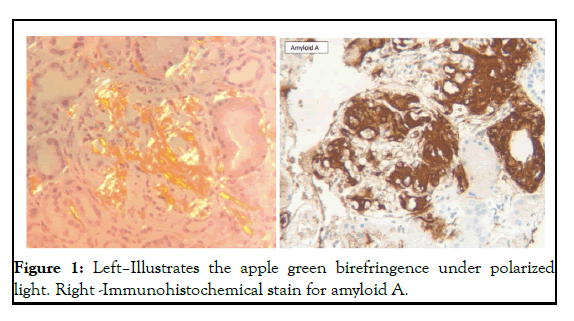
On physical examination, his vital signs were normal. General examination showed superficial bullous skin lesions containing clear fluid with positive koebner phenomenon on the extremities and abdomen. Nail dystrophy with tender hypertrophic nail bed was seen in all fingers. Pitting edema in both legs and hands was also detected. The lab test findings were isolated proteinuria of about 3755 milligrams (mg) in 24 hours urine collection, along with an acceptable renal function test (Blood Urea Nitrogen (BUN): 20 mg/dL, creatinine: 1.1 mg/dL). Hyperlipidemia and anemia were not detected. Other laboratory tests include: C-Reactive Protein (CRP): 32.5mg/liter, Erythrocyte Sedimentation Rate (ESR): 31 mm/hour, serum calcium level: 9.6 mg/dl, serum albumin: 3 g/dl, corrected serum calcium: 10.4, vitamin D: 23 ng/ml. In the complementary evaluation of nephrotic syndrome, serum complement levels of C3, C4, and CH50, immunologic markers include Antinuclear Antibody (ANA), Anti-double stranded DNA, both Perinuclear and Cytoplasmic Antineutrophil Cytoplasmic Autoantibody (P-ANCA, C-ANCA), Anti-Glomerular Basement Membrane (anti-GBM) antibody, cryoglobulin test and viral serology of hepatitis B, C, Human Immunodeficiency Virus (HIV) antibody, checked that all of them were negative. Neither serum free light chain (kappa/lambda) nor beta2 (ß2) microglobulin levels were positive but the serum protein immunofixation assay revealed a lambda monoclonal band. In imaging evaluation, abdominopelvic ultrasonic examination showed the normal size of both kidneys with bilaterally multiple cortical cysts up to 10 mm and gallbladder was full of tiny stones without sign of inflammation and otherwise were normal. Echocardiography was normal with an ejection fraction of 55%. For further investigation, a kidney biopsy was done which Light Microscopy (LM) and Immune Fluorescence (IF) features were compatible with amyloidosis as follows: The glomeruli were slightly enlarged with mildly increased mesangium that was not stained in the Jones methenamine silver stain section and palely stained with Periodic Acid Schiff (PAS). There was 5% tubular atrophy in favor of no chronicity. Congo red stain revealed amyloid deposits as foci of green birefringence under polarized light. Positive lambda staining in the IF study, concomitant with negative AA protein staining in Immune Histo Chemistry (IHC) was in favor of amyloid type AL. In consideration of AL amyloidosis, a bone marrow biopsy/ aspiration was done. It showed hypercellular marrow and plasma cell aggravation. On IHC, there was the positivity of CD138+ and scattered CD56+, also lambda chain restriction in plasma cell clusters. The plasma cell percentage was about 5%. Skin lesion biopsy revealed a subepidermal type vesiculobullous reaction and immunofluorescent examination was negative for porphyria cutanea tarda or bullous pemphigoid (Figure 1).
Results and Discussion
Primary amyloidosis is the most common form of systemic amyloidosis that is associated with plasma cell proliferation producing a monoclonal light chain immunoglobulin that its fragments deposit in different organs, and the majority of them present with plasma cell dyscrasia. The kidney is a common site in amyloid deposition. All structures of the kidney such as the glomerulus, tubules, interstitium, and renal vasculature can be complicated by the disease. Kidney involvement often presents with asymptomatic proteinuria or nephrotic syndrome due to glomerular damage, however, 5% of patients may be present with advanced renal failure with little or no proteinuria if amyloid predominantly affects the renal blood vessels or tubules. The End Stage Renal Disease (ESRD) develops in approximately 20 % of nephrotic syndrome and is associated with a poor prognosis of the disease [7]. There are several differential diagnoses of cutaneous manifestations associated with a nephrotic syndrome that include; systemic amyloidosis, Systemic Lupus Erythematosus (SLE), Granulomatosis with Polyangiitis (GPA), Polyarteritis Nodosa (PAN), Henoch-Schonlein Purpura (HSP), subacute bacterial endocarditis, cholesterol renal emboli, systemic sclerosis, malignant hypertension, hepatitis C virus, Human Immunodeficiency Virus (HIV) associated nephropathy, etc. [8]. Approximately 40% of patients with AL amyloidosis present with mucocutaneous lesions and skin manifestations depending upon the site of amyloid deposition [9]. The most common skin manifestation in systemic amyloidosis is petechiae/purpura or ecchymosis which occurs after minor trauma, particularly in the periorbital area, axillae, periumbilical and anogenital area, due to amyloid deposition in the blood vessels wall. Nontender nonpruritic papules that can be waxy, translucent, or hemorrhagic can also be seen. Nodules, plaques, target lesions, and Alopecia are less common [10]. Bullae are a rare lesion in the skin and mucosal membrane that resembles bullous pemphigoid. Nail dystrophy is a rare presentation in systemic amyloidosis that includes banding, brittleness, trachyonychia, subungual hemorrhage, longitudinal ridging, and onycholysis. It can be the initial sign of the disease.
The definitive diagnosis of systemic amyloidosis is based on clinical suspicion and by tissue biopsy with Congo red staining, but the first step in the evaluation of a patient is serum and urine immunofixation electrophoresis and a serum free light chain assay for kappa (κ) and lambda (λ) immunoglobin to seek monoclonal gammopathy. In patients with positive screening, Bone Marrow Biopsy (BMB) and fat aspiration should be considered. In highly suspicious patients with negative BMB/fat aspiration, a biopsy of the affected organ has an indication. The pattern of skin and nail involvement in our case was not a common feature of skin/nail lesions of amyloidosis, particularly together with renal involvement. We started conservative therapies with losartan 50 mg/day, furosemide 40 mg/day, and aldactone 25 mg/day to reduce proteinuria and edema and the patient was referred to a hematologist and underwent treatment for systemic amyloidosis with a combination bortezomib base regimen (bortezomib +melphalan+dexamethasone). Topical corticosteroid cream was also described for nail and skin lesions.
Conclusion
Skin and nail lesions can be the first manifestation of systemic amyloidosis. Atypical mucocutaneous presentations may be seen in amyloidosis and their recognition can help in the early diagnosis of underlying pathology.
Acknowledgments
The authors of this article would like to express special thanks to the patient for his cooperation to publish this report.
References
- Benson MD, Buxbaum JN, Eisenberg DS, et al. Amyloid nomenclature 2020: Update and recommendations by the International Society of Amyloidosis (ISA) nomenclature committee. Amyloid. 2020;27(4):217–22.
[Crossref] [Google Scholar] [PubMed]
- Picken MM. The pathology of amyloidosis in classification: A review. Acta Haematol. 2020; 143(4):322–34.
[Crossref] [Google Scholar] [PubMed]
- Gurung R, Li T. Renal amyloidosis: Presentation, diagnosis, and management. Am J Med. 2022;135: 38–43.
- Prat C, Moreno A, Vinas M, et al. Nail dystrophy in primary systemic amyloidosis. J Eur Acad Dermatol Venereol. 2008;22(1):107-9.
[Crossref] [Google Scholar] [PubMed]
- Asahina A, Hasegawa K, Ishiyama M, et al. Bullous amyloidosis mimicking bullous pemphigoid: Usefulness of electron microscopic examination. Acta Derm Venereol. 2010;90(4):427-8.
- van Herwerden MC, Wijnen M, Smedts FM, et al. Nephrotic syndrome and a maculopapular rash. Am J Kidney Dis. 2019;73(4): 13-6.
[Crossref] [Google Scholar] [PubMed]
- Kumar S, Sengupta RS, Kakkar N, et al. Skin involvement in primary systemic amyloidosis. Mediterr J Hematol Infect Dis. 2013;5(1).
- Silverstein SR. Primary, systemic amyloidosis and the dermatologist: where classic skin lesions may provide the clue for early diagnosis. Dermatol Online J. 2005;11(1).
- Litaiem N, Chabchoub I, Gara S, et al. Nail changes in systemic amyloidosis. Clin Case Reports. 2021;9(8):9–11.
- Gertz MA. Immunoglobulin light chain amyloidosis diagnosis and treatment algorithm 2021. Blood Cancer J. 2021;11(5):90.