Sign up for email alert when new content gets added: Sign up
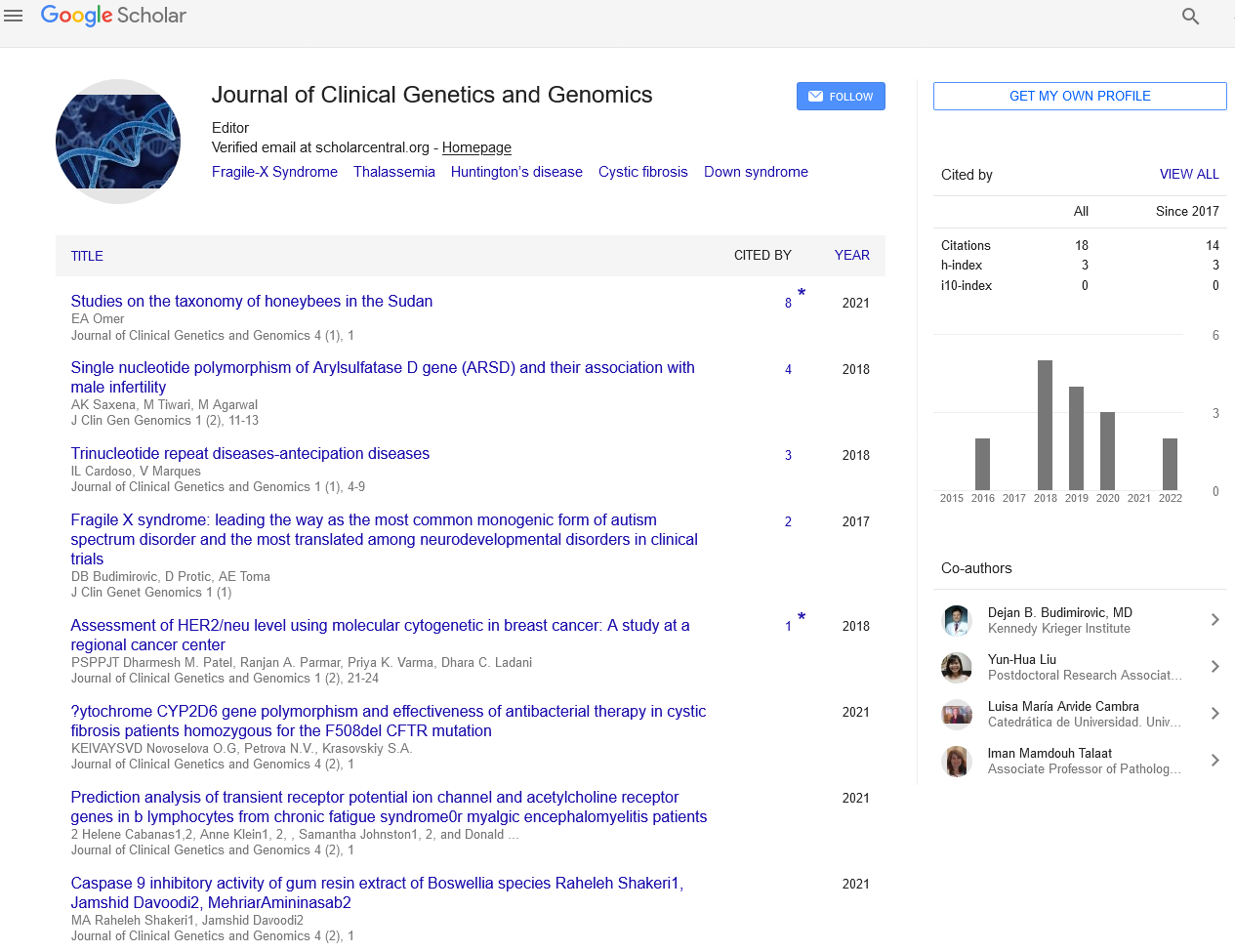
Regeneration of the immune system to fight leukemia at relapse post alloHSCT
International Conference on STEM CELLS AND REGENERATIVE MEDICINE
November 06-07, 2019 | Tokyo, Japan
Andrzej Lange
Lower Silesian Center for Cellular Transplantation with National Bone Marrow Donor Registry, Poland
Keynote: J Clin Gen Genomics
Abstract :
The use of allogeneic hematopoietic stem cell transplantation in AML patients suffering from intermediate and high-risk disease was the real breakthrough in improvement of treatment results. AlloHSCT offers rebuilding of the normal hematopoiesis ruined by leukemia and chemotherapy as well as regeneration of the immune system which after transplantation has the immune system potential of healthy donor what also means that if exposed to leukemic blasts may identify them as alien. Therefore, allogeneic hematopoietic stem cell transplantation makes the immune response against the transplanted patient cells including the blasts possible. If the immune response is not effective enough the donor lymphocytes may be infused (DLI). This approach proved to be effective especially in chronic myelogenous leukemia and in some indolent lymphomas but not good enough in AML. Unfortunately, DLI associates with a considerably toxicity with acceleration of the graft vs host process as a main cause.
Having under our observation an ALL patient who relapsed after alloHSCT with leukemic infiltrations of the bones but not the marrow we injected the donor cells directly to the bone lesions with a positive effect. To exploit this approach further we started a project on the use of intra-bone route for injection of donor lymphocytes directly to the marrow cavity at relapse - thus providing the direct contact between the leukemic cells and the fresh lymphocytes from which those seeing blasts may be recruited.
Nine patients they relapsed after alloHSCT entered the experimental group having as counter-partners the patients they received at relapse standard therapy. The aim of the project was to evaluate the feasibility of the use of intra bone route and also to identify the cells which boosted in their potential by IB-DLI might be involved in anti-leukemic effect in other words in graft vs leukemia. The observation led to the following conclusions:
• The intra-bone route proved to be convenient and free from unwanted effects.
• The lymphocyte used for infusion were taken from the primary transplant material (stimulated) or obtained de novo from the blood with the use of leukophoresis (unstimulated), both cell populations except of the content of CD34+ cells did not differ especially the proportion of CD3+ cells was very similar.
• Local anesthesia and low molecular heparin secured that infusion procedure was undisturbed
• The patients which received IB-DLI enjoyed better 12- and 18-months survival as compared to those on standard therapy (77% vs 11%, p=0.006 and 55% vs 11%, p=0.035, respectively).
• The positive effect was seen rather in the patients having the leukemic cells invaded by CD8+ lymphocytes which proportion in the marrow cell population declined as leukemia vanished (3053±1036 vs 937±±47 × 10E6 cells/L, p<0.070). The same was with the proportions of CD8+cells co-expressing PD-1 (1238±476 vs 255±73 × 10E6 cells/L, p<0.060).
• The key observation was associated with the analysis of the clonotype profiles (next generation sequencing) which showed that: (i) dominant clones identified in the recipients of IB-DLI were different from those seen in the lymphocytes prior to infusion (ii) the dominant clones rather persisted along the observation time even when the leukemia cells disappeared from the marrow, (iii) the profile of clonotypes in the marrow and in the blood was very similar in 32 out of 50 immunodominant clones what shows on the similarity between the immune system potential of the blood and marrow lymphocytes, however, the marrow lymphocyte had their local environment dependent distinctiveness.
In conclusion the IB-DLI (i) is feasibly, (ii) results with the improvement of the patients survival, (iii) is effective rather in those they have already responded to the leukemic cells with CD8+ cells but they had to be regenerated (PD-1 positivity of CD8+ cells) by providing fresh cells to achieve reversal of T-cell exhaustionand, finally, to exert clinically relevant activity.
Biography :
Andrzej Lange graduated with a medical degree with distinction from the Medical School in Wroclaw, Poland is a professor in the Institute of Immunology and Exp Therapy of the Polish Academy of Sciences and a founder and head of the Lower Silesian Center of Cellular Transplantation in Wroclaw. His international experience started in 1973-1974 as a Leverhulme fellow in the Middlesex Hospital Medical School, London. He has been a visitor and lectured in several European and North American scientific institutions. Known from his activity in the field of bone marrow transplantation and regenerative medicine. Andrzej Lange was awarded several scientific distinctions and served to a number of National and European institutions were also active in co-editing journals. He is an author and co-author of 249 scientific papers, in peer-reviewed journals with a cumulative IF of 270 in the years 1995–2017.
E-mail: lange@dctk.wroc.pl