A rare case of cardiac tamponade due to rifampicin resistance in tuberculosis: A real diagnostic and therapeutic challenge
2 Department of Anatomo-pathology, Errazi Hospital, Mohammed VI University Teaching Hospital, Marrakech, Morocco
3 Department of Microbiology, Errazi Hospital, Mohammed VI University Teaching Hospital, Marrakech, Morocco
Received: 24-Feb-2020 Accepted Date: May 01, 2020; Published: 07-May-2020
Citation: Azmoun S, Ismael G, Laalou A, et al. A rare case of cardiac tamponade due to rifampicin resistance in tuberculosis: A real diagnostic and therapeutic challenge. Clin Cardiol J 2020;4(1):1-3.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Pericarditis is a rare manifestation of tuberculosis. We report here the case of a 35-year-old woman admitted to clinical tamponade. The echocardiogram revealed a pericardial effusion of great circumferential abundance with significant respiratory variations and a bilateral pleural effusion of average abundance on chest radiography. The patient underwent emergency pericardial drainage. The initial tuberculosis assessment was negative. The culture of the liquid returned positive at 8 days revealing rifampicin-resistant tuberculosis (RR-TB).Therefore, examination of the pericardial fluid is useful in the diagnosis of tuberculous pericarditis. This case was considered TB-RR. The patient was put on a special treatment regimen after consensus, with good clinical improvement. Pericardial tuberculosis remains a rare disease. It is important to consider it as an etiological diagnosis, especially in endemic countries because it has a poor therapeutic prognosis. Early diagnosis would allow better management of these cases in order to limit cases of resistance.
Keywords
Pericarditis; Cardiac tamponade; Tuberculosis
Introduction
Globally, in 2018, approximately 10.0 million people fell ill with TB. The African Region recorded 24% of new cases. In Morocco, an incidence of 36,000 cases the same year according to the WHO [1]. TB accounts for <5% cases of pericardial disease in developed world, yet is the cause of 50% to 70% of cases in developing world [2].
Quick treatment of tuberculous pericarditis can be lifesaving and it requires a fast and accurate diagnosis for disease, but it frequently can be difficult [3]. Multidrug resistant tuberculosis (MDR-TB) has spread to most regions of the world and represents a serious threat to the success of the struggle against tuberculosis [4].
The existence of Rifampicin Resistante- Tuberculosis (RR-TB) is a serious public health problem with a prevalence in Ethiopia (9–10.3%) and Nigeria (12.1%) [5].
We report here the case of isolated RR pericardial tuberculosis revealed by a pericardial tamponade. This case hopes to illustrate the importance of a complete etiological investigation before any pericarditis in a region of tuberculosis endemic like Morocco.
Case Report
A 35-year-old woman from low socioeconomic strata, with two months history of low grade fever, breathlessness and significant weight loss was admitted in the cardiology unit of Medical hospital of Marrakech. There was no past history of diabetes, heart disease or tuberculosis.
The onset of symptoms dates back to two weeks with the setting up of an atypical chest pain worsening on deep inspiration, without radiation associated with dyspnea of effort stage II of NYHA and a productive cough with whitish sputum motivating the whole evolving in a context of fever and night shivers.
The patient consulted a general practitioner who, after clinical examination and initial evaluation, put the patient on antibiotic treatment and iron supplementation.
The clinical course is marked by the persistence of the same clinical symptomatology with an aggravation of the dyspnea becoming stage III then IV of NYHA, shortness of breath on exertion associated with orthopnea.
At admission, the patient was conscious but presented with haemodynamic and respiratory instability with a respiratory rate of 45 cpm and tachycardia with a heart rate of 150 cpm. MT: 110/67 mmHg, saturation at 96% in the open air, no coldness of the extremities.
On physical examination, the palpebral conjunctiva were not very colored; cardiac auscultation, the sounds of the hearts are muffled without breaths, a slight decrease in vocal vibrations in basithoracic, there are no signs of right or left heart failure.
A twelve-lead electrocardiogram documented sinus tachycardia, diffuse micro voltage, diffuse negative T waves, and signs of electrical alternation.
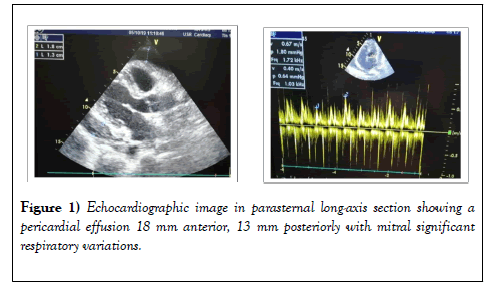
Transthoracic echocardiography (Figure 1) was performed and the result revealed a large and abundant pericardial effusion with signs of cardiac tamponade (with RV collapse on the diastole and significant respiratory variations); therefore, drainage and pericardial puncture were performed urgently with 500 ml initially removed and in total the drain brought back 3 liters of serohematic fluid with the presence of some fibrinous deposits.
The initial biological evaluation revealed: normochromic inflammatory normochromic anemia at 9.3 g/dl, a predominantly neutrophilic number of hyperleukocytosis at 11980 and lymphopenia. Reactive protein C was high, 122 mg/L and the sedimentation rate was 63.
As part of the etiological assessment:
Citrine yellow liquid, lymphocyte-dominant exudative
Evaluation of tuberculosis: search for negative bacilli in the sputum, the Genexpert is negative in the sputum and in the fluid. The Quanti FERON-TB Gold In-Tube assay returned positive. The tuberculin skin test (TCT) was not performed; LDH.
Hepatic, syphilitic and HIV serologies returned negative
Thyroid balance returned negative, phosphocalcic and renal balance is normal, LDH returned to normal.
In addition, the search for a neoplastic pathology was negative except for the tumor marker Ca125 which, in isolation, had no predictive value.
Sputum, urine and stool culture did not reveal any growth of any identified pathogen.
The initial management consisted of an emergency pericardiocentese which improved the life prognosis of the patient with a marked clinical improvement in dyspnea and tachycardia.
The patient was initially put on antibiotic therapy based on amoxicillin clavulanic acid 1g three times a day.
At 8 days of hospitalization
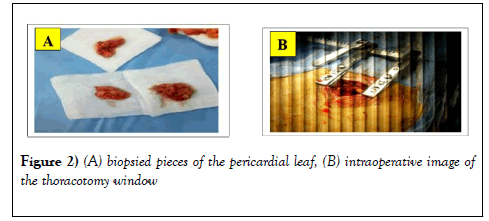
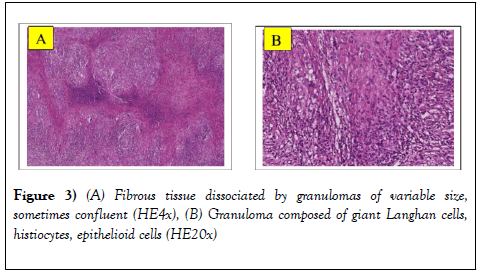
The clinical evolution is marked by a persistence of NYHA stage II dyspnea, and on the blan biology an inflammatory assessment remained positive and on the ultrasound a pericardial effusion which was reconstituted. A small thoracotomy to create a pleuropericardial window was performed in the operating room under general anesthesia. At the opening we note the presence of microadenopathies along the mediastinal chain and a biopsy of the pericardium performed (Figure 2). An anatomo- pathological examination revealed the presence of giganto-epithelioid follicles with signs of necrosis thus confirming the diagnosis of pericardial tuberculosis (Figure 3).
Figure 3: (A) Fibrous tissue dissociated by granulomas of variable size, sometimes confluent (HE4x), (B) Granuloma composed of giant Langhan cells, histiocytes, epithelioid cells (HE20x)
The culture on Lowenstein Jensen medium showed rough and buff colonies evoking Mycobacterium tuberculosis (M. tuberculosis) after 8 days of incubation and was confirmed by rapid acid staining and biochemical with a strain resistant to rifampicin. After the advice of pulmonologists and infectiologists, the patient was first put on ERIPK4 1cp/day. A discussion was conducted with the doctor responsible for the national tuberculosis control center so that the patient can be followed up in a center close to her place of residence with the molecules (ERIPK4 + Cycloserine). The patient was also placed on a steroid regimen, oral prednisolone 60 mg ounce per day.
Discussion
For most of recorded history, tuberculosis has been a problem of enormous dimensions worldwide and it still is. Extrapulmonary tuberculosis presents more of a diagnostic and therapeutic problem than does pulmonary tuberculosis [6].
Pericardial tuberculosis (TB) is a rare presentation of extrapulmonary TB. Extrapulmonary tuberculosis usually develops in 20% of patients with TB infection. It has been estimated that around 1-4 % incidence of TB pericarditis commonly occurs via dissemination of lung, spine, sternum, mediastinal lymph node, as well as during milliary infection [7].
Tuberculous pericarditis is a serious form of extrapulmonary TB associated with substantial morbidity (i.e., cardiac tamponade and constrictive pericarditis) and death during treatment for TB. Tuberculosis is said to be the most frequent cause of constrictive pericarditis in Africa and Asia [8].
Tuberculous pericarditis is estimated to occur in 1% to 2% of instances of pulmonary tuberculosis [9].
In developed countries, TB‐related pericardial disease is uncommon (<1% of extrapulmonary TB), and cases complicated by life‐threatening cardiac tamponade are extremely rare [10].
The clinical manifestations of tuberculous pericarditis are wide‐ranging and varied. While chest pain, cough, and dyspnea are common, nonspecific constitutional symptoms, including fevers, night sweats, weight loss, and fatigue, may also arise [11]. In some cases, it can be presented with chronic cardiac compression mimicking heart failure or may be presented acutely with cardiac tamponade [12]. This patient was admitted with symptoms mimicking heart failure. The patient complained of a progressive aggravation of her dyspnea evolving since one month admitted in cardiac tamponade requiring an emergency pericardiocentesis.
Active pulmonary tuberculosis and pleural effusion can be observed in 30% of cases of tuberculous pericarditis while 90% of the cases presented characteristics of active pulmonary tuberculosis [11]. Our patient presented clinically a pleural effusion syndrome confirmed by radiological explorations.
The incidence of tuberculous pericarditis is increasing with the advent of the AIDS pandemic. Tuberculosis accounts for up to 4% of acute pericarditis and 7% of cardiac tamponade. The mortality rate of tuberculosis still ranges from 14-40% [13]. Tuberculous pericarditis is a potentially lethal condition.
The pericardial effusion is mainly due to hypersensitivity to tubercular protein [14]. Multidrug-resistant tuberculosis is ubiquitous and the number of cases appears to be gradually increasing. Globally in 2018, approximately 3.4% of new cases and 18% previously treated cases had MDR-TB/RR [15].
According to the Moroccan Ministry of Public Health, in 2015, 160 MDRTB cases out of 30,636 tuberculosis cases registered, therefore 0.52%. A diagnosis of tuberculous pericarditis requires analysis of pericardial fluid or tissue. Therefore, routine testing of all patients with TB is widely recognized as the most appropriate surveillance approach for monitoring trends in drug resistant TB [15].
The development of molecular techniques, in particular GeneXpert, has not only made it possible to make a much faster diagnosis, with relatively good sensitivity and specificity and dependent on the type of sample, but also to rapidly detect any resistance to rifampicin and to isoniazid [16]. After eight days of liquid culture, the laboratory confirms us the presence of mycobacterium tuberculosis with a strain resistant to rifampicin. Note that only the Quantiferon-Gold test returned positive. No other etiological evaluation guided us with certainty towards pericardial tuberculosis.
Treating resistant TB is difficult, complicated, and requires experience and skills. Treatment can be standardized or individualized.
Conventional regimen takes up to 24 months but recently shorter regimen of up to 12 months was introduced in specific subset of MDR-TB/RR-TB patients [13]. A few reviews on the use of corticosteroids have shown that it reduced the mortality rate and reaccumulated of fluid after 18-24 months of follow-up, however, the drawback of the reviews is that, the small sample size renders the results to be inconclusive [17].
Conclusion
Tuberculosis remains an endemic disease in Morocco. Pericardial effusions are well documented, but cases of cardiac tamponade are rare. Even if the etiological evaluation of any pericardial effusion includes the systematic search for tuberculosis; emphasis must also be placed on the sensitivity of the strains and strict adherence to treatment in order to avoid cases of resistance to treatment since the treatment of RR-TB is extremely complex. The case described here reminds us that the presence of rifampicin resistance is a serious challenge. To prevent the development of highly drugresistant TB, the approach should go in the direction of finding contextualized solutions to limit the impact and spread of MDR/RR TB.
Conflict of Interests
There are no conflicts of interests for the development of this publication.
REFERENCES
- World Health Organization. Global Tuberculosis Report 2019. WHO. 2019.
- https://www.ncbi.nlm.nih.gov/pmc/articl es/PMC4027275/pdf/apjtd-03-02-161.pdf
- Johari MI, Ramli AW, Lawi, FM, et al. A rare case of purulent pericardial TB. Cureus. 2019; 11:5356.
- Zellweger JP. Multidrug resistant tuberculosis – Its extent, hazard and possible solutions. Revue des Maladies Respiratoires. 2011;28:1025-33.
- Arega B, Menbere F, Getachew Y. Prevalence of rifampicin resistant Mycobacterium tuberculosis among presumptive tuberculosis patients in selected governmental hospitals in Addis Ababa, Ethiopia. BMC Infectious Diseases. 2019;19:307.
- Broaddus VC, Mason RJ, Gotway MB. Murray and Nadel’s Textbook of Respiratory Medicine, 6th Edn, Elsevier. 2001;593-628.
- Khandaker MH, Espinosa RE, Nishimura RA, et al. Pericardial disease: Diagnosis and management. Mayo Clinic Proceedings. 2010;85(6):572-93.
- Mayosi BM. Tuberculous pericarditis and myocarditis in adults and children. Tuberculosis; 2009;31:351-60.
- Fowler NO. Tuberculous pericarditis. JAMA. 1991;266:99-103.
- Houston A, Macallan DC. Extrapulmonary tuberculosis. Medicine. 2014;42(1):18-22.
- Mayosi BM, Burgess LJ, Doubell AF. Tuberculous pericarditis. Circulation. 2005;112(23):3608-16.
- Wallrauch C, Brunetti E, Heller T, et al. Tuberculosis pericarditis with cardiac tamponade: Management in the resource-limited setting. The American Journal of Tropical Medicine and Hygiene. 2010;83(6):1311-4.
- Prasd R, Gupta N, Banka A. Multidrug- resistant tuberculosis/rifampicin-resistant tuberculosis: Principles of management. Lung India. 2018;35(1):78-81.
- Wanjari K, Baradkar V, Mathur M, et al. A case of tuberculous pericardial effusion. Indian J Med Microbiol. 2009;27(1):75-7.
- Snider DE, Kelly GD, Cauthen GM, et al. Infection and disease among contacts of tuberculosis cases with drug-resistant and drug- susceptible bacilli. Am Rev Respir Dis. 1985;132(1):125-32.
- Prasad R. Multidrug and extensively drug-resistant TB (M/XDR-TB): problems and solutions. Indian J Tuberc. 2010;57(4):180-91.
- Ntsekhe M, Wiysonge C, Volmink JA, et al. Adjuvant corticosteroids for tuberculous pericarditis: Promising, but not proven. QJM. 2003;96(8):593-9.