A rare observation of mandibular buccal ramus variant of stafne bone defect
2 Temple University, Kornberg School of Dentistry, 3223 North Broad Street, Philadelphia, PA 19140, USA
Received: 05-Jul-2018 Accepted Date: Jul 25, 2018; Published: 03-Aug-2018
Citation: Day I, Bell A, Joy A. A rare observation of mandibular buccal ramus variant of stafne bone defect. Int J Anat Var. 2018;11(3):84-86.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
The characteristically incidental finding of a mandibular bone depression, most commonly known as Stafne defect, typically presents as an asymptomatic, radiolucent lesion. Classically observed on the lingual surface of the mandibular angle, below the level of the inferior alveolar icanal, these rare idiopathic bone cavities may carry significant management implications for the treating dentist and can be difficult to diagnose in the setting of an atypical presentation. The present report describes one such unusual presentation of a Stafne bone defect identified in the mandible of an 89-year- old African-American male donor during routine anatomical dissection.
Keywords
Stafne defect; Anatomy; Oral surgical management
Introduction
In “Bone cavities situated near the angle of the mandible”, published in The Journal of the American Dental Association, Edward C. Stafne described the incidental finding of thirty-five bone cavities observed during “complete roentgenologic examination” of thirty-four patients. Due to the distinct absence of an epithelial lining, the asymptomatic cavities, which now bear his name, can usually be identified as well-circumscribed mandibular radiolucencies of non-cystic origin.
Although the pathogenesis is yet unclear, suggested origins for these defects include, failure of normal bone development [1-6], entrapment of salivary gland tissue during mandibular development [7-13], neural or vascular neoplasms [14,15], or localized pressure atrophy [3,16-18].
A variety of reports point to several locations where Stafne defect may be observed in the mandible including, the ramus, angle, and anterior regions [4,10,19-30]. Three lingual variants of these “mandibular bone depression(s)” [18] anterior, posterior, and ramus [4,6,11,12,31] are well documented. The present report describes a cadaveric observation of the extremely rare buccal ramus variant first described by Edward D. Shields in 2000.
Case Report
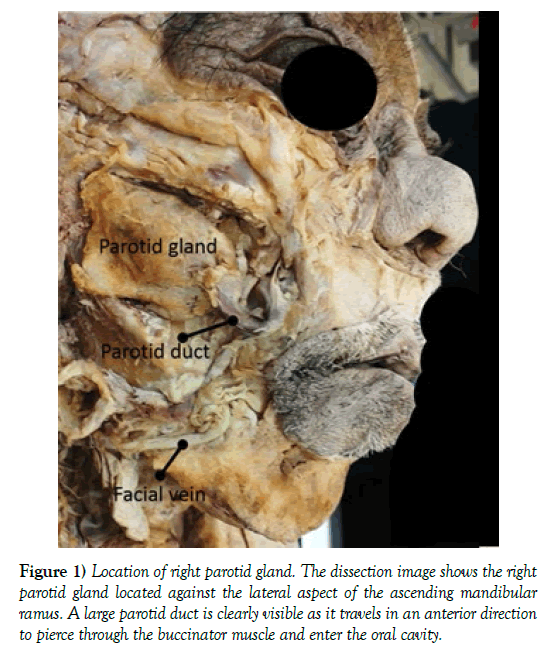
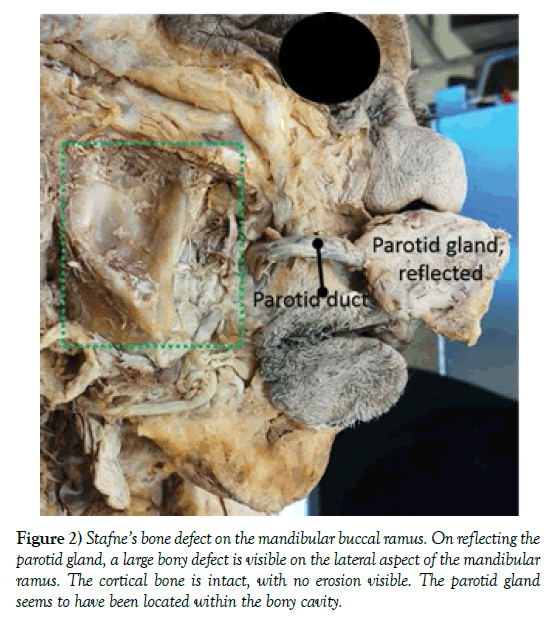
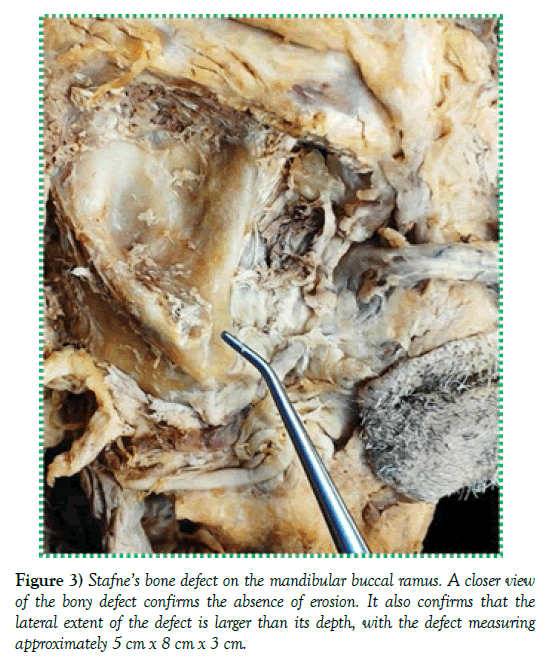
During routine cadaveric dissection of the deep face and temporal fossa regions of an 89-year-old African-American male donor, the student dissection team encountered a soft tissue mass, initially thought to be a benign or malignant tumor (Figure 1). The structure was definitively identified as an unusually large parotid gland located in the expected anatomical position, i.e., against the lateral aspect of the ascending mandibular ramus (Figure 1). As anticipated, Stensen duct emerged from the substantially sized gland, and was observed travelling in an anterior direction, ultimately piercing the buccinator muscle to gain access into the oral cavity. Anterior reflection of the grossly dissected parotid gland with its surrounding connective tissue capsule revealed a large bony depression along the lateral aspect of the ramus (Figures 2 and 3). The depression measured approximately 5 cm x 8 cm x 3 cm and was bound by prominent bony ledges creating a ‘V’-shape (Figure 3– metal probe indicates lower tip of the ‘V’-shaped depression). The associated cortical bone was intact, with no visible signs of erosion. The presence of the bony defect seemed to indicate an alternate diagnostic possibility. The defect was subsequently photographed and a thorough literature review undertaken to identify the defect, understand its pathogenesis, and uncover clinical implications. Here, we report on the extremely rare buccal ramus variant of Stafne bone defect, associated with the parotid gland. In addition to the review of literature, we also discuss the possible clinical implications of such defects in the dental patient.
Figure 1) Location of right parotid gland. The dissection image shows the right parotid gland located against the lateral aspect of the ascending mandibular ramus. A large parotid duct is clearly visible as it travels in an anterior direction to pierce through the buccinator muscle and enter the oral cavity.
Discussion
Stafne defect is a rare, localized, asymptomatic, non-progressive, and non-healing bony defect seen in the mandible. The original pathogenesis was attributed to entrapment of salivary gland tissue within the developing mandibular bone [4], or due to a failure of ossification of Meckel’s cartilage [4,6]. Later, evidence of salivary gland inclusions within these defects [7,8,13,32,33], together with development of these defects in older patients [34] seemed to indicate a defect caused as a consequence of salivary gland inclusions, especially the submandibular gland, during ossification rather than during mandible development [3]. Cases reported in literature typically indicate diagnosis of this defect in patients older than 40 years of age [15,30], further strengthening a non-developmental origin for this cavity.
The appearance of a bony defect later in age could also be explained by pressure exerted on the bone by neighboring anatomical structures, especially the major salivary glands that are often associated with these defects [18,35].
In the current case, an unusually large parotid gland was located in close proximity to the bony defect. With increasing age, non-specific inflammatory infiltration with fibrosis of major salivary glands is a common finding. This fibrosis could result in hypertrophy and/or hyperplasia of glandular tissue resulting in transformation of glandular tissue to a fibrotic mass. In addition, an intact connective tissue capsule around the parotid gland allows the gland to slide against the mandibular surface without exerting pressure. However, large masses when coupled with capsular breakdown could exert enough pressure resulting in pressure resorption in the underlying bone that can manifest as bony cavities during radiographic examinations [23,30,36]. We speculate that in the current case, such a pathogenesis most likely occurred to result in the bony cavity that is documented.
Literature reports that Stafne defects seem to occur more commonly in the lingual aspect of the mandible, and may be associated with the anterior, posterior, or ramus regions. Irrespective of location, these defects are asymptomatic and are diagnosed during incidental radiographic observations [21,37-39]. Both lingual anterior and lingual posterior variants are seen on radiographs as well-circumscribed circular or ovoid radiolucencies. The defects seem to always be located inferior to the mandibular canal, with no evidence of erosion of the mandibular canal, or involvement of the neurovascular structures within the mandibular canal. The defects also do not affect the integrity of the inferior mandibular border, as they are situated above the inferior margin of the mandible.
Depending on whether the defects are located on the lingual or buccal aspect of the mandible, these defects are further classified as lingual anterior variants, lingual posterior variants, lingual ramus variants, and buccal ramus variants. The lingual variants are almost always associated with the submandibular gland, while the parotid gland is associated with the buccal ramus variant and is extremely rare [12,13,31,40]. With the lingual anterior variant, the concavity is usually noticed in relation to the roots of the mandibular anterior teeth and can mimic the radiographic appearance of a periapical lesion [21].
Clinical implications of Stafne defect can include diagnostic difficulties wherein, the defect can mimic cystic lesions or other bony lesions [8,41- 44]. To confirm diagnoses, often conventional radiography may need to be supplemented with computed tomography and other imaging modalities, including sialograms [2,8].
In addition to diagnostic complications, Stafne defects can have clinical implications for the practicing dentist. The buccal or lingual variants of Stafne defect can have dental implications depending on their proximity to the alveolar arch. Defects located in the region of the premolars and molars could potentially compromise bone integrity as related to surgical procedures and implant placement. A defect very close to teeth roots could result in variations of root/root canal morphology, with implications for various dental procedures [21]. In addition, depending on location and size of the concavity in the mandible, surgical procedures, including dental implant placement can be adversely affected due to lack of bone structure. It is therefore important for the dentist to be aware of this condition, which might warrant a thorough radiographic evaluation before surgical procedures and implant procedures are planned for a patient.
REFERENCES
- Oikarinen VJ, Julku M. An orthopantomographic study of developmental mandibular bone defects (Stafne’s idiopathic bone cavities). Int J Oral Surg. 1974;3:71-6.
- Oikarinen VJ, Wolf J, Julku M. A stereosialographic study of developmental mandibular bone defects (Stafne’s idiopathic bone cavities). Int J Oral Surg. 1975;4:51-4.
- Segev Y, Puterman M, Bodner L. Stafne bone cavity--magnetic resonance imaging. Med Oral Patol Oral Cir Bucal. 2006;11: E345-7.
- Stafne EC. Bone cavities situated near the angle of the mandible. J Am Dent Assoc. 1942;29:1969-72.
- Aguiar LB, Neves FS, Bastos LC, et al. Multiple stafne bone defects: a rare entity. ISRN Dent. 2011.
- Tolman DE, Stafne EC. Developmental bone defects of the mandible. Oral Surg Oral Med Oral Pathol. 1967;24:488-90.
- Palladino VS, Rose SA, Curran T. Salivary Gland Tissue in the Mandible and Stafne’s Mandibular ‘Cysts’. J Am Dent Assoc. 1965;70:388-93.
- Bourjat P, Cavezian R, Pasquet G. Stafne’s lacuna, a salivary inclusion in the mandible. Apropos of a case. J Radiol. 1985;66:71-3.
- Salman L, Chaudhry AP. Malposed sublingual gland in the anterior mandible: a variant of Stafne’s idiopathic bone cavity. Compendium. 1991;12:40-3.
- Ariji E, Fujiwara N, Tabata O, et al. Stafne’s bone cavity. Classification based on outline and content determined by computed tomography. Oral Surg Oral Med Oral Pathol. 1993;76:375-80.
- Richard EL, Ziskind J. Aberrant salivary gland tissue in mandible. Oral Surg Oral Med Oral Pathol. 1957;10:1086-90.
- Barker GR. A radiolucency of the ascending ramus of the mandible associated with invested parotid salivary gland material and analogous with a Stafne bone cavity. Br J Oral Maxillofac Surg. 1988;26:81-4.
- Barker GR. Xeroradiography in relation to a Stafne bone cavity. Br J Oral Maxillofac Surg. 1988;26:32-5.
- Mann RW, Tsaknis PJ. Cortical defects in the mandibular sulcus. Oral Surg Oral Med Oral Pathol. 1991;71:514-6.
- Minowa K, Inoue N, Sawamura T, et al. Evaluation of static bone cavities with CT and MRI. Dentomaxillofac Radiol. 2003; 32:2-7.
- Grellner TJ, Frost DE, Brannon RB. Lingual mandibular bone defect: report of three cases. J Oral Maxillofac Surg. 1990; 48:288-96.
- Philipsen HP, Srisuwan T, Reichart PA. Adenomatoid odontogenic tumor mimicking a periapical (radicular) cyst: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;94:246-8.
- Philipsen HP, Takata T, Reichart PA, et al. Lingual and buccal mandibular bone depressions: a review based on 583 cases from a world-wide literature survey, including 69 new cases from Japan. Dentomaxillofac Radiol. 2002;31:281-90.
- Barakat N, Nasseh I. Stafne’s cyst simulating a periapical cyst. Apropos 2 cases. Rev Stomatol Chir Maxillofac. 1992; 93:119-21.
- Belmonte-Caro R, Velez-Gutierrez MJ, Garcia De La Vega-Sosa FJ, et al. A Stafne’s cavity with unusual location in the mandibular anterior area. Med Oral Patol Oral Cir Bucal. 2005;10:173-9.
- Bornstein MM, Wiest R, Balsiger R, et al. Anterior Stafne’s bone cavity mimicking a periapical lesion of endodontic origin: report of two cases. J Endod. 2009;35: 1598-1602.
- Bras J, Habets LL, Verbraak LA, et al. Radiolucencies in the region of the mandibular angle and below the mandibular canal. Stafne’s idiopathic bone defect]. Ned Tijdschr Tandheelkd. 1984;91:90-5.
- Campos PS, Panella J, Crusoe-Rebello IM, et al. Mandibular ramus-related Stafne’s bone cavity. Dentomaxillofac Radiol. 2004;33:63-6.
- Florin W, Mandel L. Stafne’s bone cavity anterior mandible. Case report. N Y State Dent J. 76:36-8.
- Friedrich RE, Zustin J, Scheuer HA, et al. An unilateral basal bone defect of the mandible occupied by fatty tissue: Stafne’s cavity. In Vivo. 26:1045-8.
- Lello GE, Makek M. Stafne’s mandibular lingual cortical defect. Discussion of aetiology. J Maxillofac Surg. 1985;13:172-6.
- Phillips A, Yates C. Case report: anterior lingual mandibular cortical bone concavity. Dent Update. 2004;31:175-6.
- Piette E. Lingual cortical mandibular defects (Stafne’s defects). Rev Belge Med Dent. 1986;41:47-53.
- Steiner RM, Goldstein BH, Gold L. The medial mandibular bone concavity (Stafne’s defect). Radiol. 1979;130:344.
- Campos PS, Oliveira JA, Dantas JA, et al. Satfne’s defect with buccal cortical exansion: a case report. Inter J Denti. 2010;2010: 3.
- Wolf J. Bone defects in mandibular ramus resembling developmental bone cavity (Stafne). Proc Finn Dent Soc. 1985;81: 215-21.
- Choukas NC, Toto PD. Etiology of static bone defects of the mandible. J Oral Surg Anesth Hosp Dent Serv. 1960;18:16-20.
- Adra NA, Barakat N, Melhem RE. Salivary gland inclusions in the mandible: Stafne’s idiopathic bone cavity. Am J Roentgenol. 1980; 134:1082-3.
- Hansson LG. Development of a lingual mandibular bone cavity in an 11-year-old boy. Oral Surg Oral Med Oral Pathol. 1980; 49:376-8.
- Turkoglu K, Orhan K. Stafne bone cavity in the anterior mandible. J Craniofac Surg 2010; 21:1769-75.
- Shimizu M, Osa N, Okamura K ,et al. CT analysis of the Stafne’s bone defects of the mandible. Dentomaxillofac Radiol. 2006; 35:95-102.
- Munevveroglu AP, Aydin KC. Stafne bone defect: report of two cases. Case Rep Dent. 2012;2012:654839.
- More CB, Das S, Gupta S, et al. Stafne’s Bone Cavity: A Diagnostic Challenge. J Clin Diagn Res. 2015;9:ZD16-9.
- Herranz-Aparicio J, Figueiredo R, Gay-Escoda C. Stafne’s bone cavity: An unusual case with involvement of the buccal and lingual mandibular plates. J Clin Exp Dent. 2014;6:e96-9.
- Shields ED. Technical note: Stafne static mandibular bone defect-further expression on the buccal aspect of the ramus. Am J Phys Anthropol. 2000;111:425-7.
- Kirkpatrick TJ. Stafne’s idiopathic bone cavity with complications in diagnosis. Dent Mag Oral Top. 1967;84:191-3.
- Salman L, Leffler M, Reddi T, et al. Stafne’s bone (defect) simulating dentigerous cyst of the mandible. J Oral Med. 1986;41:239-41.
- Bianchi SD, Boccardi A, Gandini G. Traditional radiologic and tomodensitometric aspects of the so-called Stafne’s cysts. Radiol Med. 1986;72:534-8.
- Simpson W. A Stafne’s Mandibular Defect Containing a Pleomorphic Adenoma: Report of Case. J Oral Surg. 1965;23:553-6.