Accessory Attachment Between the Uvula and the Palatine Tonsil - A Case Report
Received: 03-Apr-2023, Manuscript No. ijav-23-6318; Editor assigned: 04-Apr-2023, Pre QC No. ijav-23-6318 (PQ); Accepted Date: Apr 21, 2023; Reviewed: 18-Apr-2023 QC No. ijav-23-6318; Revised: 21-Apr-2023, Manuscript No. ijav-23-6318 (R); Published: 28-Apr-2023, DOI: 10.37532/1308-4038.16(4).253
Citation: Aaron P, Saylor F, Kaya G et al. Accessory Attachment between the Uvula and the Palatine Tonsil - A Case Report. Int J Anat Var. 2023;16(4):281-282.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Assessing anatomical variation can reveal a more complete understanding of clinical correlates. Variations in the palatal region of the pharynx have been the focus of many research studies. Most reports closely examine the role of tonsillar infections in the development of abnormal uvular structure. In this report, we outline a considerable uvular attachment to a palatine tonsil in an 80-year-old female donor discovered during anatomical dissection. A thin extension of tissue originating in the apex of the uvula attached distally into the medial surface of the right palatine tonsil. This discovery inspired further investigation and a review of the literature.
Keywords
Uvula; Uvular variation; Tonsillar attachment
INTRODUCTION
Knowledge of the human body both grossly and down to the molecular level is fundamental to understanding the structures and physiological functions of different body systems. In today’s healthcare, there is an increase in the use of technology to aid in diagnosis and treatment. From computed tomography (CT) to magnetic resonance imaging (MRI), physicians must use their knowledge of anatomical structures to quickly point out a lesion or decipher the root cause of a disease. As a result, knowledge of anatomy has been increasingly necessary to not only interpret imaging, but to understand how certain medications and therapies may target different tissues and organs.
A cadaver approach to learning anatomy in supplement with a lecture-based curriculum serves to be both an efficient and effective approach. Students can take what they learn in the confines of a classroom and directly apply it as they dissect in the lab. Cadavers uniquely portray a realistic nature and allow students to compare “healthy” and “pathological” immediately. Additionally, anatomical dissections in a group setting reinforce the respectful and compassionate attitudes student physicians must uphold as they continue their medical career.
CASE REPORT
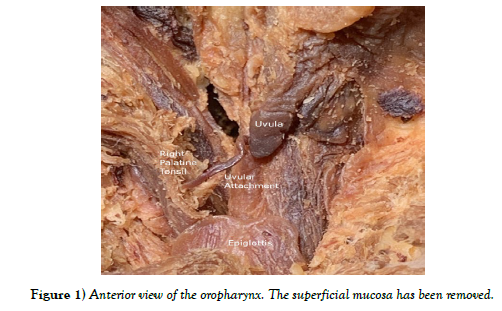
During an anatomical dissection of an 80-year-old female formalin-fixed whole-body donor, an abnormal attachment of the uvula to the right palatine tonsil was observed (Figure 1). In situ, the uvula appeared proportional to surrounding structures, but there was a distinct, thin extension of tissue arising from the apex of the uvula, measuring approximately 1.75 inches in length during initial dissection. The distal aspect of the tissue extension was attached to the medial surface of the right palatine tonsil. This connection deviated the uvula slightly to the right but did not appear to create any tractional tension on the involved structures. Neither the tissue extension nor its attachment to the tonsil created any appreciable obstruction in the oral cavity. The surrounding regions and structures were carefully dissected to analyze any additional relationships or abnormalities. The photos referenced in this report were approved after the dissection was completed.
The uvula is a small, midline structure hanging from the posterior inferior distal third of the soft palate. While the function of the uvula is not entirely known, it is known that the uvula plays a role in swallowing and guiding contents within the oral cavity [1]. The uvula receives its blood supply from branches of the palatine and pharyngeal arteries, while being innervated by the pharyngeal plexus [2]. Embryologically, fusion of the palatal shelves will go on to create the soft palate and thus the uvula [3].
The palatine tonsils are paired, bilateral structures composed of lymphoid tissue located in the oropharyngeal mucosa. Anteriorly, the tonsils are bordered by the palatoglossal arch, while posteriorly they are bound by the palatopharyngeal arch [4]. Since palatine tonsils are composed of lymphoid tissue, their function is primarily immunological; they play a key role in immune mucosal defense against airborne and alimentary pathogens. The palatine tonsils receive their blood supply from an extensive network of fenestrated capillaries [5]. The palatine tonsils are formed from the second pouch of the embryological pharyngeal arch [3].
DISCUSSION OF OTHER ABNORMALITIES REGARDING THE UVULA
Symptoms of tonsillitis include sore throat, halitosis, cervical lymphadenopathy, and the presence of inflammatory tissue debris on tonsillar surfaces [6]. Patients with recurrent tonsillitis experience recurring episodes of infection of the palatine tonsils by bacteria colonized within the tonsillar crypts [6]. The bacteria are released to the tonsillar surface during acute exacerbations, causing infection and an inflammatory response to ensue. Infectious organisms, such as Staphylococcus aureus (S. aureus), Klebsiella pneumoniae (K. pneumoniae), and Treponema pallidum (T. pallidum) causing syphilis, have been associated with colonization of tonsillar and palatine tissues that can disrupt the anatomical structure and positioning of the uvula. For example, Coulson (1862) provided a case report describing a syphilis patient with soft palate adhesions to the posterior pharynx, obstructing the lumen between the nasopharynx and oropharynx leading to subsequent symptoms including anosmia, ageusia, breathing and speech difficulties. Furthermore, a second case study by Cooke [7] discussed a syphilitic patient who experienced sore throat, dysphagia, and hemorrhagic symptoms due to an enlarged, flat, elongated, and superficially ulcerated uvula that adhered to the posterior pharyngeal wall, right tonsil, and right palatine arch [6]. (2021) compared the bacterial colonization prevalence of Staphylococcus aureus (S. aureus) versus Klebsiella pneumoniae (K. pneumoniae) on the tonsillar surface or crypts in twenty-five recurrent tonsillitis patients through a case series study to evaluate proper identification of the causative organism of tonsillitis through methods of swabbing tonsillar surfaces and obtaining a punch biopsy of tonsillar crypts. The researchers found S. aureus to be more common on the tonsillar surfaces and K. pneumoniae within the tonsillar crypts; however, both organisms produced biofilms with antimicrobial drug resistance, indicating difficulty in their eradication and likelihood to cause reinfection [6]. These studies suggest that disruption of the microbiota with opportunistic organisms can induce inflammatory processes that can alter the structure and function of oropharyngeal tissues. For patients with recurrent tonsillitis symptoms, tonsillar removal via a tonsillectomy procedure is often warranted, yet such procedures come with risks to uvula positioning and structure.
Chang [8] used before and after lateral cephalogram images taken three months apart to compare differences in uvula position and palatal length between the uvula tip (UT) and posterior nasal spine (PNS), the palatal angle between the nasal floor and junction of the PNS and UT, and the retrouvula length between the anterior cervical vertebrae and UT, in children with tonsillitis who received an adenotonsillectomy versus those who did not. These researchers found that patients who underwent adenotonsillectomy had presented with a significant increase in palatal length, palatal angle, and retrouvula length after surgery, while control patients presented with changes in retrouvula length and palatal angle only, but no significant difference in palatal length within three months [8]. They concluded that adhesion of the anterior tonsillar pillars to the posterior tonsillar pillars after an adenotonsillectomy does create a positional change of the uvula, but it is still unknown the clinical importance of this positional change [8]. Yet, this does indicate that the size of the retropalatal space and location of the uvula can be altered with manipulation of soft palate tissue after surgery. Furthermore, other cases of uvula necrosis with severe sore throat and foreign body sensation symptoms have been reported after endotracheal intubation procedures required during certain surgeries. Both [9] and [10] discuss cases of patients presenting with elongated, swollen, ulcerated and necrotic uvula tips during follow-up appointments for surgical procedures that required endotracheal intubation. Both reports suspect the uvula suffered a compression injury from the tube that blocked the proper blood supply and oxygen content from reaching the uvula tissue, leading to ischemic damage and necrosis. Noting these changes to the uvula is important because structural damage affects proper functioning of the uvula to close the nasopharynx opening during swallowing, so food and other secretions do not enter the nasal cavity. Thus, serious complications disrupting speech patterns and breathing capabilities from the presence of uvula and tonsillar swellings and adhesions can result if these tissue alterations are not attended.
Other abnormalities that have been reported regarding the uvula include isolated angioneurotic edema, also known as Quincke’s disease. Similar to uvular adhesions, cases of Quincke’s disease are also quite rare. Symptoms of Quincke’s disease that have been reported include foreign body sensation in the throat, excessive gag and vomiting sensation. Patients have denied fevers and chills. Upon physical examination, the uvula appeared swollen, erythematous and enlarged. Implicated etiologies of Quincke’s disease include trauma, drug reactions, inhalation exposure, and food allergies [11- 13].
As for this current case, our cadaver had her tonsils intact; however, the tip of her uvula was elongated and adhered to one tonsil. On visual inspection of our donor, her uvula was attached to the palatine tonsil, but the uvula and other pharyngeal structures were of normal anatomical size and proportion. This includes the tonsils which appeared normal. From the literature discussed previously, we can postulate that perhaps she had an infection that may have led to alteration of tonsillar tissues (i.e., swelling) or received prolonged endotracheal intubation that could have initiated the development of adhesions, leading to displacement of her uvula. The cause of death of our cadaver was reported as heart and lung disease, yet we did find a cancer port located in her right subclavian vein. Thus, we can assume our cadaver was likely immunocompromised and highly susceptible to infections like K. pneumoniae or S. aureus, which may have influenced these unique changes to her uvula and tonsillar tissues. Furthermore, it is unknown whether our patient received endotracheal intubation with endof- life care, for lung incapacities, or other previous procedures, however it is plausible to consider intubation as a potential contributor to our cadaver’s uvular tissue changes.
ACKNOWLEDGEMENT
The authors would like to thank the donor for her selfless gift to advance medical knowledge. Additionally, the authors would like to thank Dr. Aaron Beger, Dr. Jonathan Millard, and Dr. Michael Breiner for their help and guidance. The authors also emphasize their appreciation to Edward via College of Osteopathic Medicine for supporting research and creating educational opportunities.
REFERENCES
- Mukai S. Functions of the Uvula and Z-Pharyngoplasty. Psychiatry Clin Neurosci. 2000; 54(3):346-7.
- Olofsson K, Mattsson C, Hammarstrom M-L, Hellstrom S. Structure of the human uvula. Acta Otolaryngol. 1999; 119(6):712-717.
- Sadler, Thomas W. Langman's Medical Embryology. 14th ed. Wolters Kluwer, 2019; 311-312.
- Moore K, Agur A, Dalley A. Clinically Oriented Anatomy. Wolters Kluwer. 2018; 9-43.
- Jović M. Ultrastructure of the Human Palatine Tonsil and Its Functional Significance. Rom J Morphol Embryol. 2015; 56(2):371-7
- Klagisa R, Kroica J, Kise L. S. aureus and K. pneumoniae on the Surface and within Core of Tonsils in Adults with Recurrent Tonsillitis. Medicina (Kaunas). 2021: 22; 57(10):1002.
- Cooke AB. Adhesion of the soft palate and uvula to the posterior wall of the pharynx-operation-cure. Am J Dent Sci. 1873; 7(1):25-29.
- Chang SW, Song C, Hong Kim J, Lim G-C, Kang J, et al. Positional changes in the uvula tip after adenotonsillectomy in children: preliminary result. PeerJ. 2021: 1; 9:e12-243.
- Salengros JC, Founas WE, Velghe-Lenelle CE, Willemse E, Sosnowski M, et al. Uvular and tonsillar pillar mucosal necrosis as a cause of severe sore throat after orotracheal intubation. Anaesth Intensive Care. 2011; 39(4):772-773.
- Ji L, Goldin M. Uvula necrosis, an atypical presentation of sore throat. J Emerg Med. 2013; 44(1):185-186.
- Chandran A, Sakthivel P, Chirom AS. Quincke’s disease. BMJ Case Reports. 2019; 12:e231-967.
- Coulson, WJ. Adhesion of the soft palate to the posterior wall of the pharynx, following syphilitic ulceration. The Lancet. 1967; 29(2):103-104.
- Shiber JR. Quincke’s Disease: Isolated Uvulitis. West J Emerg Med. 2014; 15(6):6-63.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref