Adult antiretroviral drugs special considerations for treatment and prevention of HIV infection
Received: 07-Sep-2021 Accepted Date: Sep 21, 2021; Published: 28-Sep-2021
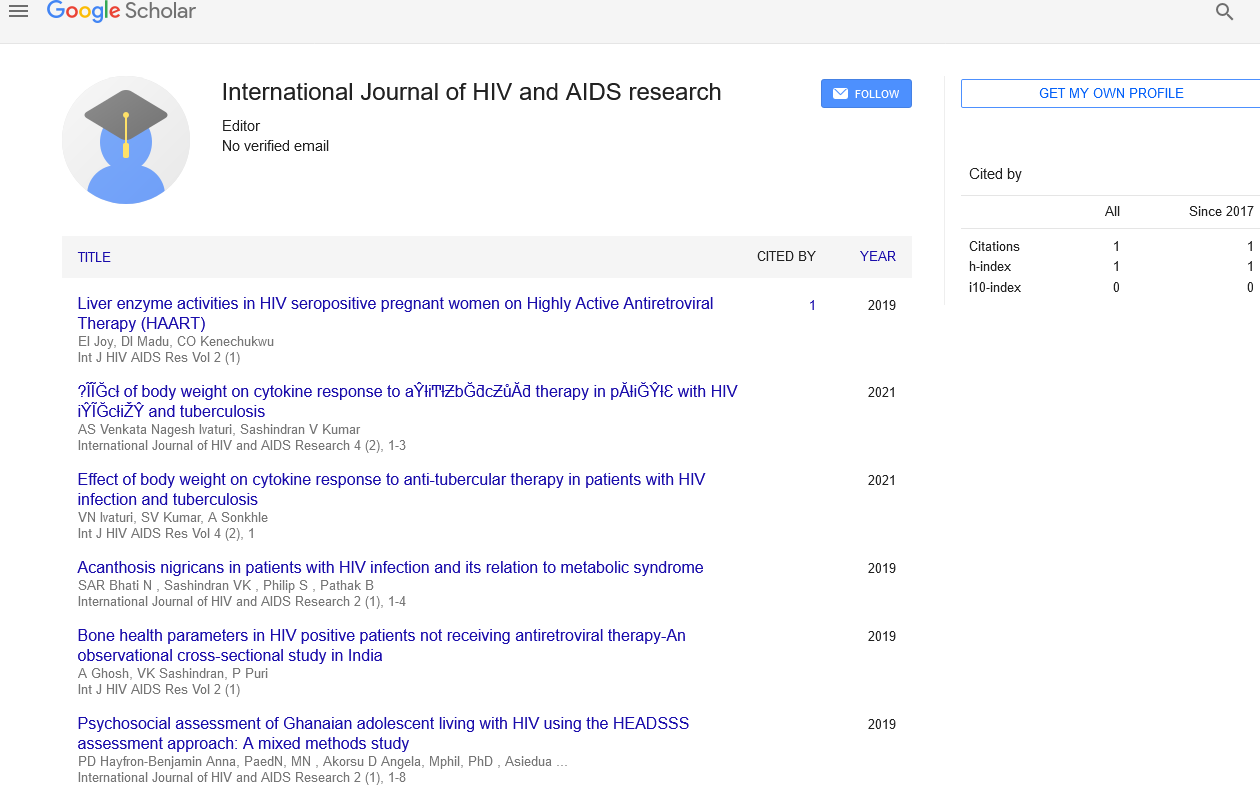
Citation: Geethanjali K. Adult antiretroviral drugs special considerations for treatment and prevention of HIV infection. Int J HIV AIDS Res. 2021;4(5): 1-1.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Commentary
HIV-positive pregnant women should start Antiretroviral Therapy (ART) for their personal health and to lower the risk of HIV transmission to the baby (evidence rating AIa). Abacavir/lamivudine (if the patient is HLA-B*5701 negative), TDF/emtricitabine, or zidovudine/lamivudine are all nucleoside reverse transcriptase inhibitors. The zidovudine/lamivudine regimen has the most clinical experience, but it also has the most toxic side effects. The approved InSTI for use during pregnancy is raltegravir. Atazanavir/r (once daily) or darunavir/r are two boosted PIs that are recommended (twice daily). When started after the first eight weeks of pregnancy, the NNRTI efavirenz is indicated. If an HIV-positive woman on efavirenz becomes pregnant, the regimen may be continued; changing it risks virologic control being lost.
Coinfection with the hepatitis B virus
Patients with HIV who also have hepatitis B virus (HBV) should start an ART regimen that includes TDF or TAF (evidence rating AIa), lamivudine or emtricitabine, and a third component.
60–62 both lamivudine and emtricitabine have potent antiviral properties against HBV. However, if these medications are administered without TDF or TAF, there is a considerable risk of HBV resistance and viral breakthrough, and none is indicated for HBV coinfection alone. HBV infection may be treated with entecavir (evidence rating AIII). Entecavir should be avoided if HIV RNA is not suppressed because it can select for lamivudine- and emtricitabine-resistant HIV.
Coinfection with the hepatitis C virus
Patients with HIV and Hepatitis C Virus (HCV) should begin Antiretroviral Therapy (ART) with medications that do not have substantial drug interactions with HCV therapies (evidence rating AIIa). Dolutegravir/ abacavir/lamivudine and dolutegravir or raltegravir plus TAF/emtricitabine are the recommended regimens with the fewest medication interactions with current HCV therapies. Before employing any other ART regimens, especially those that involve NNRTIs, boosted HIV PIs, or elvitegravir/c, clinicians should examine current HCV therapy guidelines.
Disease of the bones
HIV infection increases the risk of osteoporosis and fractures.
64 Patients may lose 2% to 6% of their bone mineral density at the hip and spine during the first 1 to 2 years after starting ART. Patients on TDFcontaining regimens experience a larger initial loss of bone mineral density than those on TAF- or abacavir-containing regimens. As a result, TDF is not advised for patients who have osteopenia or osteoporosis (evidence rating BIII).
Kidney illness
When starting or changing ART, monitoring for kidney damage with eGFR, urinalysis, and testing for glycosuria, albuminuria, or proteinuria is advised, as is testing for glycosuria, albuminuria, or proteinuria every 6 months (along with HIV RNA) once HIV RNA is stable (evidence rating BIII). TDF (particularly with a raised PI) enhanced the risk of chronic renal disease in cohort studies. Patients with an eGFR of less than 60 mL/min should not use tenofovir disoproxil fumarate. Abacavir (which does not require dose adjustment in this context) or TAF (if creatinine clearance is more than 30 mL/min) are the two alternatives (evidence rating AIIa). There are few long-term data on TAF in individuals with pre-existing renal illness. If renal function worsens, especially if there is evidence of proximal tubular dysfunction (e.g., euglycemic glycosuria or urinary phosphate squandering), tenofovir disoproxil fumarate (TAF) should be stopped (evidence rating AIIa). TAF’s safety in individuals with active TDF-related proximal tubulopathy has yet to be established. If at all possible, TAF should be started only after tubulopathy has cured, with recurrence being monitored. HIVpositive patients with end-stage renal illness should be considered for kidney transplantation, with good patient and graft survival rates expected (evidence rating AIIa).