An Indian boy with post-infantile acquired cerebral palsy caused by submersion injury: A rare etiology and a therapeutic challenge
Received: 04-Mar-2022, Manuscript No. PULJCP-22-4403; Editor assigned: 12-Mar-2022, Pre QC No. PULJCP-22-4403(PQ); Accepted Date: Mar 19, 2022; Reviewed: 14-Mar-2022 QC No. PULJCP-22-4403(Q); Revised: 16-Mar-2022, Manuscript No. PULJCP-22-4403(R); Published: 24-Mar-2022, DOI: 10.37532/puljcp.2022.6(2).11-14
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
INTRODUCTION: Cerebral palsy is a heterogeneous disorder that can cause a lifelong disability that is associated with a nonprogressive damage in the brain. It is commonly caused by antenatal, perinatal, early postnatal and neonatal conditions. However, post-neonatal cases of acquired cerebral palsy have also been reported, and were commonly caused by infection.
CASE PRESENTATION: The father of an Indian boy, who developed severe cerebral palsy caused by submersion injury before about three months, consulted us during December, 2021 about the possible therapies for his condition. Clinical picture and brain imaging abnormalities are described, and the relevant literatures were reviewed with the aim of suggesting possible evidence-based therapies.
RESULTS: At the age of 21 months, a previously healthy boy who was living in Houston, Texas, was involved in a near fatal drowning accident. The boy was hospitalized, and severe global brain damage resulted in no vision, hearing, and motor skills. The doctors in Houston, Texas, USA told the father that his son won’t be able to ever get any motor skills back, and will remain in vegetative state factorial therapies including cerebrolysin, citicoline, piracetam.
DISCUSSION: Cerebral palsy is a heterogeneous disorder that can cause a lifelong disability that is associated with a non-progressive damage in the brain. It is commonly caused by antenatal, perinatal, early postnatal and neonatal conditions. However, post-neonatal cases of acquired cerebral palsy have also been reported, and were commonly caused by infection.
CONCLUSION: In this paper, the rare occurrence of severe postinfantile cerebral palsy is described. Emphasis is made on the possibility of using evidence-based multi-factorial therapies in cerebral palsy.
Key Words
Acquired post-infantile; Cerebral palsy; Submersion injury; Multifactorial therapies
INTRODUCTION
Cerebral palsy is a heterogeneous disorder that can cause a lifelong disability that is associated with a non-progressive damage in the brain. It is commonly caused by antenatal, perinatal, and early postnatal and neonatal conditions. However, post-neonatal cases of acquired cerebral palsy have also been reported, and were commonly caused by infection [1-10].
Case Presentation
The father of an Indian boy, who developed severe cerebral palsy caused by submersion injury before about three months, consulted us during December, 2021 about the possible therapies for his condition. Clinical picture and brain imaging abnormalities are described, and the relevant literatures were reviewed with the aim of suggesting possible evidence-based therapies.
Results
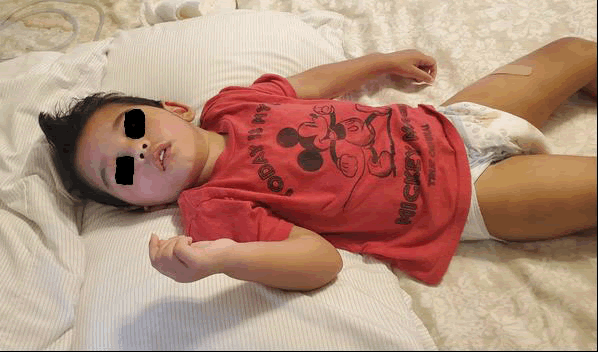
At the age of 21 months (September, 2021), a previously healthy boy (Figure 1) who was living in Houston, Texas, was involved in a near fatal drowning accident. The boy was hospitalized (Figure 2), and severe global brain damage resulted in no vision, hearing, and motor skills. The doctors in Houston, Texas, USA told the father that his son won’t be able to ever get any motor skills back, and will remain in vegetative state.
Figure 2: The boy was hospitalized after a near fatal drowning accident
The boy was hospitalized for one and half month ago and was receiving hyperbaric oxygen therapy at 1.2 atm pressure. He has completed 23 dives out of 40. After discharge from hospital he was responding to painful stimuli.
On the 28th of September, 2021, MRI showed extensive and relatively symmetric regions of gliosis and volume loss especially involving the basal ganglia and thalami and brainstem and occipital cortex. There was also global atrophy of the cerebral hemispheres and cerebellum, moderately extensive cystic encephalomalacia in the bilateral globus pallidus medial aspect of the putamen bilaterally and with volume loss, and T2 hyperintensity in the bilateral thalami and seen in the bilateral midbrain and in the bilateral pons in the bilateral cerebellar hemispheres.
In addition, there was T2 hyperintensity and volume loss within cortex especially in the bilateral occipital lobes medially and diffuse volume loss of cerebral cortex throughout some volume loss of cerebral white matter. This is associated with enlargement of lateral ventricles and third ventricle and fourth ventricle. There was no shift of midline. No subdural collections.
Flow-voids in major vessels at base of brain were generally normal. The A1 segment of the right anterior cerebral artery is hypoplastic, a normal variant of the circle of Willis. Optic nerves appear normal. Globes were normal. There was extensive opacification of paranasal sinuses and maxillary sinuses and ethmoid air cells are also opacification mastoid air cells middle ears.
Three months after the accident, at about the age of two years (Figure 3), the boy had poor spontaneous movements and was not producing any voice. He was receiving Keppra 100 mg three times daily, Baclofen 10 mg three times daily, and Clonazepam 0.1 mg three times daily.
The addition of oral citicoline based on the evidence provided by our publications was associated with the appearance of some purposeful movement his hands.
He was still not tolerating feeding with naso-gastric tube, and remained feeding via G/J tube, and needed suction of his secretions every two hours.
Discussion
Cerebral palsy is a heterogeneous disorder that can cause a lifelong disability that is associated with a non-progressive damage in the brain. It is commonly caused by antenatal, perinatal, early postnatal and neonatal conditions. However, post-neonatal cases of acquired cerebral palsy have also been reported, and were commonly caused by infection [1-15].
Blair and Stanley reported that 11% of cases of cerebral palsy in Western Australia were postnatally-acquired condition, and males under one year of age, were particularly vulnerable [16]. Infections such as meningitis and encephalitis accounted for more than 50% of the cases, and accidents accounted for about 25% of the cases. Other causes included epileptic fits and cerebrovascular accidents. Arens and Molteno from South Africa reported that the chief causes of postnatal acquired cerebral palsy were cerebral infections (particularly meningitis), cerebral trauma and cerebrovascular accidents [17].
Murphy, et al. from the USA reported that the Metropolitan Atlanta Developmental Disabilities (A population-based study, 1985-1987) found that 16% of children with cerebral palsy had a postnatallyacquired condition [18].
Cans, et al reported that 50% of cases of cerebral palsy with postneonatal origin (arising more than 28 days after birth, and before theage of 25 months) were caused by infection; 20% caused by vascular episodes, 18% caused by head injury [19]. They suggested that children with cerebral palsy of post-neonatal origin had a more severe functional pattern than non-post-neonatal cerebral palsy children.
Reid and colleagues from Australia reported that 10.7% of 339 cases of cerebral palsy had post-neonatally acquired condition caused by infection, traumatic head injury a, hypoxia, acute encephalopathies, and cerebrovascular accidents [20].
The work of Salih (from Sudan emphasized that prenatal causes were the most common causes of cerebral palsy, but post natal causes included neonatal jaundice and acquired sepsis [21].
For the patient in this report, we suggested the use of evidence-based treatments which included intramuscular cerebrolysin and oral citicoline.
Cerebrolysin solution contains free amino acids (85%) and 15% biologically active low molecular weight amino acids including neuropeptides (Brain-derived neurotrophic factor, glial cell line-derived neurotrophic factor, nerve growth factor, ciliary neurotrophic factor [22]. Cerebrolysin has been used safely with benefit in a variety of neuro-psychiatric disorders including idiopathic mental retardation, cerebral palsy, myelomeningocele, pediatric juvenile spinal muscular atrophy, pediatric Charcot Marie Tooth disease, kernicterus, and agenesis of corpus callosum with colpocephaly [23-31].
Citicoline, which has been increasingly grouped with the water soluble B vitamins, and is regarded as a form of the essential nutrient choline. It has been increasingly used with noticeable benefits in the treatment of several pediatric neuro-psychiatric disorders including, pervasive developmental disorders including Rett syndrome, and kernicterus.
CONCLUSION
In this paper, the rare occurrence of severe post-infantile cerebral palsy is described. Emphasis is made on the possibility of using evidence-based multi-factorial therapies in cerebral palsy.
Declarations
The author would like to express his gratitude for the family of the patients who willingly accepted publishing the photo of their child.
REFERENCES
- Mosawi Al AJ. Dramatic effect of nandrolone decanoate on motor development in cerebral palsy. Arch Dis Child 2008; 93(11); 338-339.
Google scholar Crossref - Mosawi Al AJ. Cerebral palsy: A unique illustrated experience. Med Res Chron. 2020;7(4):217-239.
Google scholar Crossref - Mosawi Al AJ. A novel therapeutic approach for the treatment of brain atrophy. Lambert Acad Publ; 2017.
Google scholar Crossref - Mosawi Al AJ. New therapies for the treatment of spastic cerebral palsy. Med J Clin Trials.2019; 3(2);209
Google scholar Crossref - Mosawi Al AJ. The pattern of cerebral palsy in Iraqi children. Med Life Clin. 2019;1(1):1001.
Google scholar Crossref - Mosawi Al AJ. The experience with the use of nandrolone decanoate and pyritinol in children with cerebral palsy. Op Acc J Bio Sci & Res. 2020; 2(3).
Google scholar Crossref - Mosawi Al AJ. Congenital externally communicating porencephaly presenting as hemiplegic cerebral palsy: imaging study of a rare condition. Sun Krist J Neonat Pediatr.2021;3:1013.
Google scholar Crossref - Mosawi Al AJ. The early treatment of a boy from Virginia with ataxic cerebral palsy. J Pediatr Child Health. 2021; 2 (4):1-5.
Google scholar Crossref - Mosawi Al AJ. A girl from canada with severe cerebral palsy associated with hydrocephalus and mutation of kinase d-interacting substrate of 220-kda (kidins220) gene: a new syndrome with unique brain imaging findings and a therapeutic challenge. J Clin Res Radiol.2021;4(1)
Google scholar Crossref - Mosawi Al AJ. Cerebral palsy: An illustrated groundbreaking experience: evidence-based medicine (Dutch Edition). Publ Our Knowl.. 2020.
Google scholar Cross ref - Blair E, Stanley FJ. An epidemiological study of cerebral palsy in western Australia, 1956–1975. Iii: Postnatal aetiology. Dev Med Child Neurol.1982;24(6):575-585.
Google scholar Crossref - Himmelmann K, Uvebrant P. Function and neuroimaging in cerebral palsy: a population‐based study. Dev Med Child Neurol. 2011; 53(6):516-521.
Google scholar Crossref - Murphy CC, Yeargin- Allsopp M, Decouflé P, D. et al. Prevalence of cerebral palsy among ten-year-old children in metropolitan Atlanta, 1985 through 1987. J pediatr.1993; 123(5):13-20.
Google scholar Crossref - Cans C, McManus V, Crowley M, et al. SCPE (Surveillance of Cerebral Palsy in Europe) collaborative group. Cerebral palsy of post‐neonatal origin: characteristics and risk factors. Paediatr Perinat Epidemiol. 2004; 18(3):214-220.
Google scholar Cross ref - Reid SM, Lanigan A, Reddihough DS. Post‐neonatally acquired cerebral palsy in Victoria, Australia, 1970–1999. J Paediatr. 2006; 2(10):606-611.
Google scholar Crossref - Salih K. Pattern of cerebral palsy among Sudanese children less than 15 years of age. Cureus. 2020 Mar 10:12(3).
Google scholar Crossref - Mosawi Al AJ. Clinical uses of cerebrolysin in pediatric neuropsychiatry. Sci World J Pharm. Sci. 2020;1(1):1-4.
Google scholar Crossref - Mosawi Al AJ. A unique experience with mental and developmental retardation: Innovative Medical therapies for idiopathic mental retardation. Clin. Med Case Rep. 2020; 3(5):42-54.
Google scholar Crossref - Mosawi Al AJ. New therapies for Rett syndrome. J Bio Innov. 2019; 8(3):301-307.
Google scholar Crossref - Mosawi Al AJ. New therapies for the treatment of ataxic cerebral palsy caused by kernicterus. EC Clinical and Medical Case Reports. 2020; 3(4):26-31.
Google scholar Crossref - Mosawi Al AJ. New medical therapies for the treatment of myelomeningocele. Surg Med Open Access J. 2019; 2(4):1-4.
Google scholar Crossref - Mosawi Al AJ. A novel therapy for pediatric juvenile spinal muscular atrophy. Saarbrücken. 2018.
Google scholar Crossref - Mosawi Al AJ. The use of cerebrolysin in pediatric Wohlfart Kugelberg Welander syndrome. MOJ Clin. Med Case Rep .2020; 10(1):20-23.
Google Scholar Crossref - Mosawi Al AJ. A novel therapy for pediatric Charcot Marie Tooth disease. L Lambert Acad Publ. 2018.
Google scholar Crossref - Mosawi Al AJ. The use of Cerebrolysin in Pediatric Charcot Marie Tooth Disease. J Neurol Res Ther.2020;3(2).
Google scholar Crossref - Mosawi Al AJ. The novel use of cerebrolysin and citicoline in the treatment of kernicterus. J Neurol Brain Disord. 2019;3(1):208-12.
Google scholar Crossref - Mosawi Al AJ. The use of intramuscular cerebrolysin and citicoline in the treatment of kernicterus. Sun Krist J Neonat Pediat. 2019;1(1):1-5.
Google scholar Crossref - Mosawi Al AJ. Agenesis of corpus callosum with colpocephaly: A novel therapy. Lambert Acad Publ. 2019.
Google scholar - Mosawi Al AJ. The use of piracetam and cerebrolysin in the treatment of agenesis of corpus callosum with colpocephaly. EC Clinic Med Case Reports. 2020; 3(1):1-5.
Google scholar Crossref - Mosawi Al AJ. Citicoline research progress. Saarbrücken. 2019.
Google scholar Crossref - Mosawi Al AJ. The use of citicoline in pediatric neurology and pediatric psychiatry. Aust Pediatri. 2019; 6(1):1071-1072.
Google scholar Crossref