Anatomical variations of sacral hiatus and associated clinical relevance - A review
Received: 01-Nov-2017 Accepted Date: Nov 07, 2017; Published: 14-Nov-2017
Citation: Rajani S. Anatomical variations of sacral hiatus and associated clinical relevance - A review. Int J Anat Var. 2017;10(4): 96-98.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Sacral hiatus is caudal opening of sacral canal. Caudal epidural anaesthesia for various therapeutic and diagnostic procedures is administered through sacral hiatus. 25% failure rate of caudal epidural block has been reported in literature. The failure rate of this procedure may be due to variant anatomical features of sacral hiatus. Hence knowing the anatomical variations in shape, size, level of apex and baseof sacral hiatusis of paramount importance to clinicians to reduce failure rate of caudal epidural block. For this review, literature search was done in the department of anatomy using databases, Scielo, Scopmed, medline, pubmed and Wiley online library. Only English language articles and standard text books were referred. The anatomical features of sacral hiatus has immense value to orthopaedic surgeons, obstretricians, paediatricians, anaesthecians and anatomists. This review will update and consolidate the information on sacral hiatus and will serve a ready reference for future researchers and clinicians.
Keywords
Sacral hiatus; Sacral canal; Epidural anesthesia; Apex of sacral hiatus
Introduction
The word os sacrum was derived from Greek word hieron osteon and was first used by Romans. A more plausible explanation may be that the holiness of the sacral bone was an attribute borrowed from the ancient Egyptians, who considered this bone sacred to Osiris, the god of resurrection and agriculture [1]. The sacrum is formed by fusion of five sacral vertebrae and present between the two innominate bones forming postero-superior wall of pelvic cavity [2]. Vertebral foramina of sacrum forms sacral canal.
It contains cauda equine, spinal meninges, sacral and coccygeal nerve roots. The opening present at the caudal end of sacral canal is known as sacral hiatus. Its shape is variable but generally it is triangular in shape with apex upward and base downward. It contains fifth pair of sacral nerve, coccygeal nerve and filum terminale. It is formed due to the failure of fusion of laminae of the fifth sacral vertebra. It is located inferior to the 4th fused sacral spines or lower end of median sacral crest.
The inferior articular process of fifth sacral vertebra projects downward on both sides of sacral hiatus which is known as sacral cornua (horn). It is an important landmark to locate the sacral hiatus during caudal epidural anaesthesia. On the body surface the hiatus can be marked two inches above the tip of coccyx beneath the skin of natal cleft [2,3].
The hiatus is covered posteriorly by skin, a subcutaneous fatty layer and the sacrococcygeal membrane [4]. The dural sac ends at the level of the S2 vertebra. The sacral canal below this level contains extradural fat, vertebral venous plexus, lower sacral nerve roots and the filum terminale [2,5,6].
Epidural anaesthesia in obstetrics [7] and transpedicular and lateral mass screw placement in orthopaedic practice [4] is done through sacral hiatus Thus the more precise knowledge of anatomical variations of sacral hiatus as observed by various authors [4,8-12], the more successful and reliable caudal epidural anaesthesia will be. As the variations in location, shape and size of the sacral hiatus are also caused by occult sacral spina bifida and fusion of coccygeal vertebra so knowledge of these anatomical variants also improve the above clinical procedures. The variant morphology and morphometry of sacral hiatus is important for successful colposcopy also [13]. The large sacral hiatus due to development, sacral bifida or otherwise will reduce the area for the attachment of extensor muscle at back causing painful conditions [14]. Sacral hiatus with guide wire assistance is an accessible conduit for uncomplicated entry into the subarachnoid and basal cisternal space without damaging the surrounding structures [15].
Thus the precise knowledge of not only anatomical variants like absence of sacral hiatus and narrowing of sacral canal but also variant size and shape of sacral hiatus are essential for successful anaesthetic procedures. Caudal epidural block is used for anaesthesia and analgesia below umbilicus in young ages and in urgent procedures like incarcerated hernia, perineal procedure, and lower limb surgery and in superficial operations such as skin grafting [16]. Tsui et al. [17] reported failure rate of caudal epidural block as high as 25%. Due to such immense clinical implications associated with variant anatomical features of sacral hiatus, updating present and past research work carried out by researchers and consolidating the knowledge of all the variations for ready reference for future researchers and clinicians so study has been carried out.
Materials and Methods
Literature search was conducted in the department of Anatomy, AIIMS Rishikesh using following data bases for updating knowledge of variant features of sacral hiatus and to bring out associated clinical consequences.
Thedatabasesused for searchareScielo, Scopmed, medline, pubmed and Wiley online library. The papers containing original data were selected and secondary references retrieved from bibliographies. The search was restricted to English language articles and selected reference text books. Search terms used for surfing the literature were as follows-Sacral hiatus, variations of sacral hiatus, anatomical features of sacral hiatus and sacral hiatus and its clinical implications [18,19].
Results and Discussion
Caudal opening of sacral canal, due to posteriorly unfused laminae of 5th sacral vertebra, is known as sacral hiatus. Shape and size of the hiatus depends on the number of laminae that fails to fuse in the midline posteriorly. These features of sacral hiatus are important for administering caudal epidural anesthesia. The variations in the position of apex and base coupled with shape of sacral hiatus are described as under-
Level of apex of sacral hiatus: Standard textbooks of Anatomy describe that the apex of sacral hiatus is at the level of 5th vertebra. The position of apex of sacral hiatus can vary from S2 to S5 vertebrae. Location of apex of sacral hiatus as elucidated by various authors is tabulated in Table-1. The most common level of apex of sacral hiatus is S4 vertebra followed by S3and least common in S2 as illustrated in table.
| S.No | Level of apex | kumarVinod et al. (1992) [10] | Sekiguchi M et al. (2004) [4] | Nagar S.K. (2004) [18] | Shinde V.K. et al. (2016) [19] | Kumari Rita et al. (2016) [16] |
|---|---|---|---|---|---|---|
| 1. | S2 vertebra | 4.95% | 4% | 3.40% | 1.03% | 0 |
| 2. | S3 vertebra | 8.91% | 15% | 37.30% | 17.52% | 4.76% |
| 3. | S4 vertebra | 76.23% | 65% | 55.90% | 79.38% | 80.95% |
| 4. | S5 vertebra | 7.43% | 15% | 3.40% | 2.06% | 7.14% |
Table 1: Showing level of apex of sacral hiatus as reported by various authors
Apex of sacral hiatus at the level of S1, S2 and S3 has also been described by Singh R [20]. But the term sacral spina bifida ocuulta (SSBO) was used by her. Apex of sacral hiatus at the level of S1 is not reported in literature may be due to extremely rare frequency of occurrence.
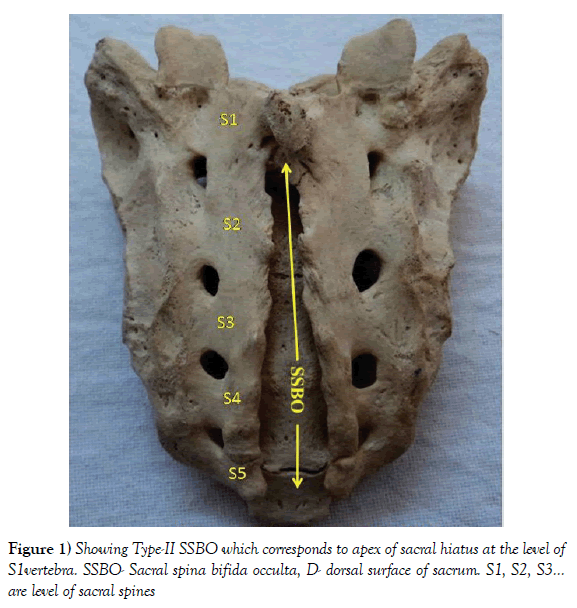
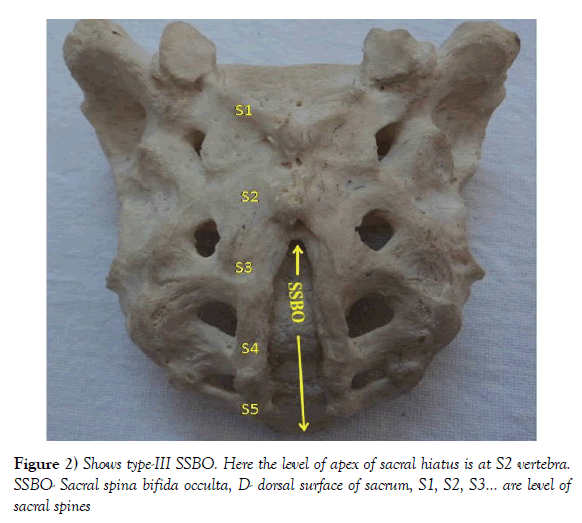
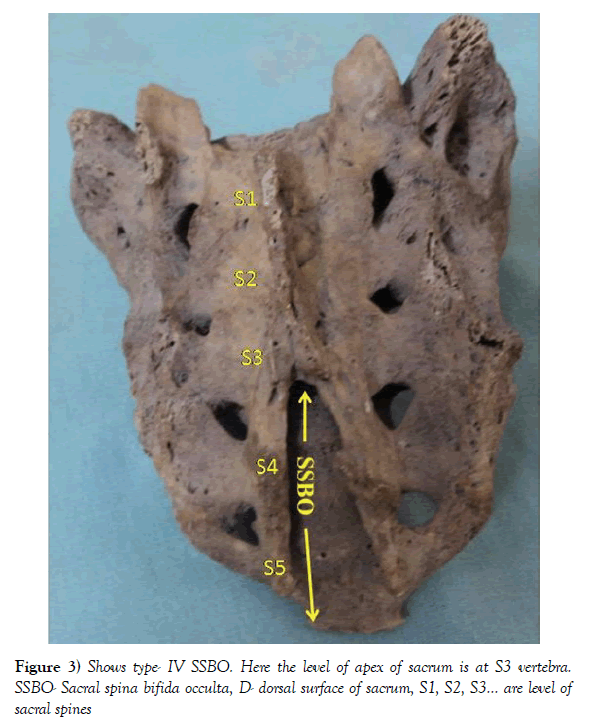
Apex of sacral hiatus at S1 level corresponds to Type-II SSBO (Figure 1) and that at S2, S3 to Type III (Figure 2) and Type IV SSBO (Figure 3) respectively as reported by Singh R [20]. In addition to this she is of the view that opening of sacral canal at various levels is due to double mutation of Foxc2 and Pax9 genes. Hence higher level of apex of hiatus may also be due to double mutation of Foxc2 and Pax9 genes. Shifting apex of sacral hiatus at higher level is due to failure of fusion of continuously higher laminae culminating in progressively increasing length of sacral hiatus/SSBO [12,20].
Increase in length of the sacral hiatus is caused by the defect of unfused 2nd and 3rd and 4th pair of sacral laminae and also by coccygeal ankylosis [12,21].
Duncan et al. [22] stated that, distance from the apex of the sacral hiatus to the lower lumbar spinous processes is important to develop the techniques to prevent the neurological injury associated with the neuraxial injections.
Base of sacral hiatus: Variations in the base of sacral hiatus have been detected by many authors and are described below.
Most common level of base of sacral hiatus as detected by various authors is S5 vertebra with occurrence ranging from 70% to 98.96% (Table 2) [16,19,23-25]. But Mustafa et al. [26] found base of sacral hiatus at the level of S5 vertebra in all observed sacra. The variation found in the level of base of sacral hiatus may be due to varied sample size, specimen from various regions and also due to sacra from different sexes.
| S.No. | Level of base | Kumari Rita et al. [16] | ShindeVK et al. [19] | Desai et al. [23] | Seema et al. [24] | Sinha et al. [25] |
|---|---|---|---|---|---|---|
| 11 | S4 vertebra | - | 1.03% | 4.33% | 13.42% | - |
| 22 | S5 vertebra | 39 sacra | 98.96% | 75.19% | 70.46% | 80.71% s |
Table 2: Showing comparison of base of sacral hiatus as described by various authors
Shape of sacral hiatus: Lot of variations in the shapes of sacral hiatus like inverted U, inverted V, irregular and dumbbell shaped were detected by various authors. Comparison of shapes of sacral hiatus as reported by various authors is tabulated in Table-3. Data of Table-3 reveals that the most common shape is inverted U followed by inverted V.
| S. No. | Authors | Inverted U % | Inverted V % | Irregular % | Dumbell % |
|---|---|---|---|---|---|
| 11. | Seema et al. [24] | 42.95 | 27.51 | 16.1 | - |
| 22. | Njihia et al. [27] | - | 32.1 | - | - |
| 33. | Kumari Rita et al. [16] | 40.47 | 33.33 | 21.42 | - |
| 44. | Desai et al. [23] | 42.12 | 35.43 | 12.99 | 5.51 |
| 55. | Mustafa et al. [26] | 26 | 24 | 22 | 22 |
Table 3: Showing variations in the shapes of sacral hiatus
Inverted U and V shapes provide enough space for needle access during caudal epidural anesthesia making anesthetists more comfortable in giving anesthesia, whereas dumbbell and irregular shapes provide challenge for this process [26,27].
Clinical implications associated with sacral hiatus: In 1900, caudal epidural anesthesia was done for the first time involving injection of a drug into the epidural space through sacral hiatus for analgesia [11]. In 1901, technique of caudal epidural injection developed [28]. In 1942 continuous caudal epidural anesthesia was introduced [7]. Edward [7] used sacral hiatus for continuous caudal analgesia during labour for the first time.
Anatomical abnormalities of the sacrum include upward and downward displacement of the sacral hiatus, narrowing or partial obliteration of the sacral canal, ossification of the sacrococcygeal membrane, absence of bony posterior wall of the sacral canal and variation in shape of the sacral hiatus [29]. While performing caudal epidural block, needle passes through skin, subcutaneous tissue and sacrococcygeal ligament and needle enters into caudal epidural space [4]. When caudal epidural block is done under the guidance of ultrasonography then the success rate is 100% but it is not always possible due to various reasons such as availability of instrument, cost etc. [23] Epidural space is approached through sacral hiatus for giving analgesia and anesthesia for various surgical manipulations, treatment of lumbar spinal disorders and management of chronic back pain. Sacral hiatus has also been utilized for administration of epidural anesthesia in obstetrics for painless deliveries, perineal surgeries, colposcopy, orthopaedic diagnosis and surgery, treatment of sciatica to give corticosteroids injections, also used to provide pre and post - operative analgesia in adults and children or it may be combined with general anesthesia. The variant shape, size and location of sacral hiatus provide variable space through which caudal epidural anaesthesia is given for various purposes. The sacral cornua are bony landmark to locate the sacral hiatus.
An important point in caudal epidural block is awareness of the distance between the sacral hiatus and dural sac anatomically to avoid dural puncture [30] hence anatomical variation of sacral hiatus is important to prevent the iatrogenic injury of dural sac during caudal epidural anesthesia. According to Dalens [31], the known shape and size of sacral hiatus provides easy access to the sacral epidural space at a level below the termination of the dural sac where most of the roots of the cauda equina are no longer inside the sacral canal.
Conclusion
Thorough and detailed knowledge of anatomical variant features of sacral hiatus will improve failure rate of caudal epidural block for anesthesia and analgesia in surgical manipulations of orthopaedic, lumbar spinal disorders, chronic back pain, obstetrics for painless deliveries, perineal surgeries and colposcopy and in the treatment of sciatica to give corticosteroids injections, to provide pre and post - operative analgesia in adults and children.
REFERENCES
- Sugar O. How the Sacrum Got Its Name. JAMA. 1987;257:2061-3.
- Soames RW. Gray’s Anatomy. Edinburgh Churchill Livingstone. 2008;528-31.
- Moore KL, Dalley AF. Clinically oriented Anatomy. New York, Lippincott Williams & Wilkins. 1995.
- Sekiguchi M, Yabuki S, Satoh K, et al. An anatomical study of the sacral hiatus: a basis for successful caudal epidural block. Clin J Pain. 2004;20:51-4.
- Waldman SD. Caudal epidural nerve block: prone position. In: Atlas of Interventional Pain Management. Philadelphia, Saunders, 2004;380-92.
- Ellis H. The sacrum and the caudal block. Anaesth Intensive Care Med. 2006;7:397-8.
- Edward WB. Hingson RA. Continuous caudal anesthesia in obstetrics. AmJSurg. 1942;57:459-64.
- Trotter M, Lanier PF. Hiatus canalissacralis in American whites and Negroes. Hum Biol 1945;17:368-81.
- Trotter M. Variations of the sacral canal; their significance in the administration of caudal analgesia. Curr Res Anesth Analg. 1947;26:192-202.
- Kumar V, PandeySN, Bajpai RN, et al. Morphometrical study of sacral hiatus. J Anat Soc 1992;41:7-13.
- Chen PC, Tang SF, Hsu TC, et al. Ultrasound guidance in caudal epidural needle placement. Anesthesiology 2004; 101:181-4.
- Aggarwal A, Harjeet, Sahni D. Morphometry of sacral hiatus and its clinical relevance in caudal epidural block. Surg radiol anatomy. 2009;31:793-800.
- Mourgela S, Sakellaropoulos A, Anagnostopoulou S, et al. The dimensions of the sacral spinal canal in the colposcopy: a morphometric MRI study. Neuroanat 2009; 8:1-3.
- Brailsford JF. Deformities of lumbosacral region of spine. Br J Surg. 1929;16:562-627.
- Layer L, Riascos R, Firuzbakht F, et al. Subarachnoid and Basal Cistern navigation through the sacral hiatus with guidewire assistance. Neurol Res. 2011;33:633-7.
- Kumari Rita, Shobha Kumari, Atulya Prasad, et al. An Anatomical Study of Variations of Sacral Hiatus and Its Clinical Correlation. IOSR-JDMS. 2016;15:18-21.
- Tsui BC, Tarkkila P, Gupta S, et al. Confirmation of caudal needle placement using nerve stimulation. Anaesth Analg. 1999;91:374-8.
- Nagar SK. A study of sacral hiatus in dry humansacra. J Anat Soc India. 2004;53:18-21.
- Shinde VK, Shirbadgi SA. Study of variations in levels of sacral hiatus. Int J Anat Res. 2016;4:1882-5.
- Singh R. Classification, Causes and Clinical Implications of Sacral Spina Bifida Occulta in Indians. Ba Sci Med. 2013;2:14-20.
- Singh R. Sacrum with five pairs of sacral foramina. Int J Anat Var. 2011;4:139-40.
- Duncan MA, Sherriff M, O’Keeffe D, et al. A radiographic assessment of the distances from the sacral hiatus to the lower lumbar spinous processes. Eur J Anat. 2009;13:19-22.
- Desai Rajeev R, JadhavSurekha D, DoshiMedha A, et al. Variations in anatomical features of the sacral hiatus in indian dry sacra. Int J Med Res Health Sci. 2014;3:634-8.
- Seema, Singh M, Mahajan A. An Anatomical Study of Variations of Sacral Hiatus in Sacra of North Indian Origin and Its Clinical Significance. Int J Morphol. 2013; 31:110-4.
- Sinha MB, Rathore M, Trivedi S, et al. Morphology of first pedicle of sacrum and its clinical relevance. IJHBR. 2013; 1:234-40.
- Mustafa Mohamed S, Omayma M Mahmoud, Hoda H A El Raouf, et al. Morphometric study of sacral hiatus in adult human Egyptian sacra: Their significance in caudal epidural anesthesia. Saudi J Anaesth. 2012;6:350-7.
- Njihia BN, Awori KO, Gikenye G. Morphology of the sacral hiatus in an African Population-Implications for Caudal Epidural Injections. Ann Afr Surg. 2011;7:20-3.
- Collins VJ. Principles of anesthesiology. Philadelphia: Lea and Febiger. 1976;716-726.
- McLeod G. Spinal anaesthesia: Intradural and extradural. In: Lee’s Synopsis of Anaesthesia. Churchill Livingstone. 2006;471–536.
- Senoglu N, Senoglu M, Oksuz H, et al. Landmarks of the sacral hiatus for caudal epidural block: an anatomical study. Bri J Anaesth. 2005;95:692-5.
- Dalens BJ. Regional anesthesia in children. Churchill Livingstone. 2006;1719–1762.