Breastfeeding in HIV-Infected Mothers: Demystifying The Dilemma
Received: 30-Jun-2022, Manuscript No. PULIJHAR-22-5119; Editor assigned: 01-Jul-2022, Pre QC No. PULIJHAR-22-5119(QC); Reviewed: 15-Jul-2022 QC No. PULIJHAR-22-5119; Revised: 29-Aug-2022, Manuscript No. PULIJHAR-22-5119(R); Published: 05-Sep-2022
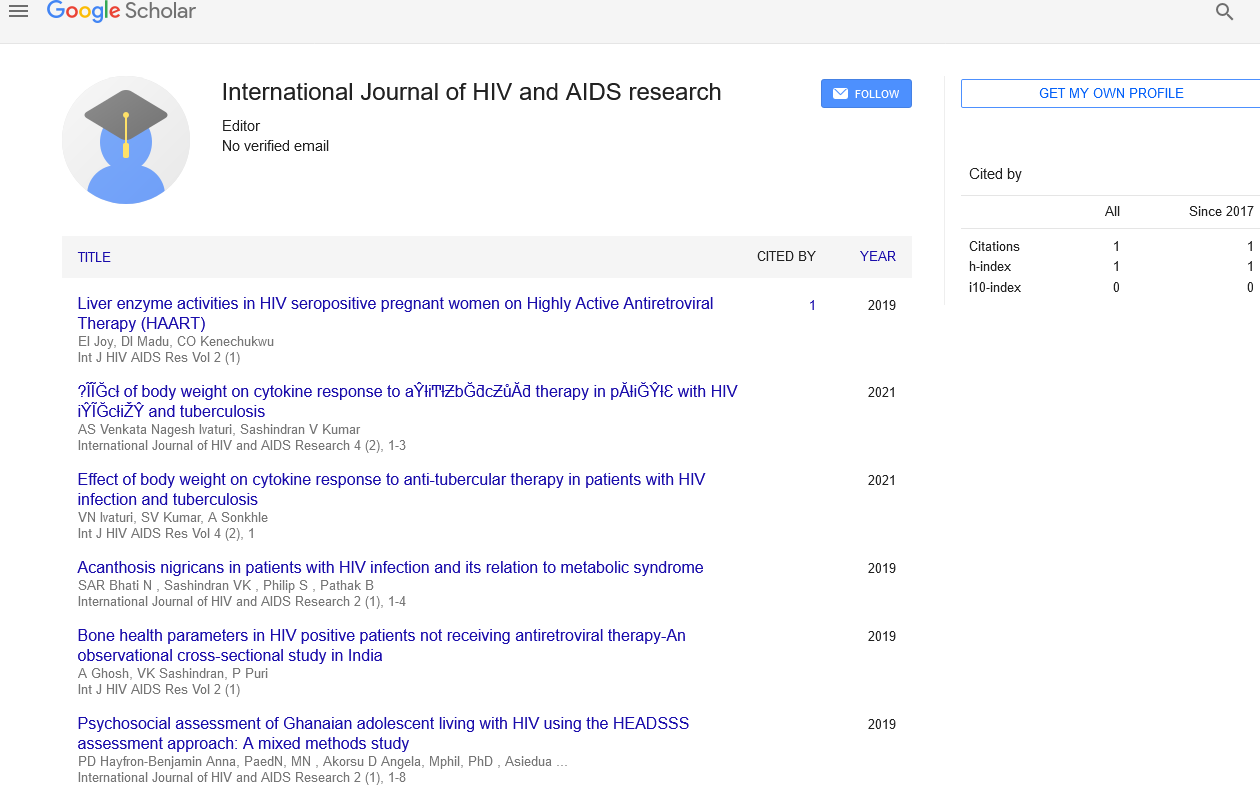
Citation: Shubha HV. Breast feeding in HIV infected mothers: demystifying the dilemma. Int J HIV AIDS Res. 2022;5(3):6.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Editorial
In the developing and under developed countries, breastfeeding is one of the cornerstone practices considered to be of utmost importance for child’s health, development and survival and is also highly considered as the safest and cheapest way to feed an infant. This is mainly because in a child of less than five years of age, diarrhea, respiratory infections (pneumonia) and undernutrition are the leading causes of mortality and therefore, exclusive breastfeeding up to six months of life is highly recommended. However, for an HIV infected mother, breastfeeding is still a major challenge and they remain dubious or uncertain about it. In this context, World Health Organization (WHO) in 2010 for the first time recommended the use of antiretroviral drugs to prevent postnatal transmission of HIV through breastfeeding and has also put forwarded a public health approach and recommended the national authorities to encourage and assist one feeding practice to all women infected with HIV accessing care in public health facilities. Many countries have largely enforced the recommendations in the 2010 WHO guidelines on HIV and infant feeding.
In 2014, the guidelines on HIV and infant feeding were reviewed and four aspects were given priority while the rest of the 2010 guidelines were considered as rational and logical. Those four aspects with the updated 2016 WHO recommendations are as follows:
What is the duration of breastfeeding by mothers living with HIV?
• Recommendation: HIV infected mothers should breastfeed for at least 12 months and may continue up to 24 months or longer while being fully supported for ART adherence.
What are the interventions to support infant feeding practices by mothers living with HIV?
• Recommendation: National and local health authorities should actively participate and execute services in health facilities and activities in workplaces, communities and homes to protect, encourage and support breastfeeding among women living with HIV.
What to advise when mothers living with HIV do not exclusively breastfeed?
• Recommendation: Mothers living with HIV should be reassured that Anti-Retroviral Therapy (ART) reduces the risk of postnatal HIV transmission in the setting of mixed feeding. Although exclusive breastfeeding is highly recommended, the use of mixed feeding is not a reason to terminate breastfeeding in the presence of ARV drugs.
What to advise when mothers living with HIV do not plan to breastfeed for 12 months?
• Recommendation: HIV infected mothers can be reassured that shorter durations of breastfeeding of less than 12 months are better than never commencing breastfeeding at all.
In a developed country, such as in the United States, where mothers with HIV are affordable, babies are fed with instant formula milk in contrast to the WHO recommendation of exclusive breastfeeding in HIV infected mothers with ART in progress. However, this concept of high resource countries is not accepted widely as it does not seem to be either feasible or practical in many ways. If women with HIV intend to feed her child with breast milk, then the doctors and other health care professionals must extend a helping hand and guide her regarding this. Since the risk of transmission of HIV through breast milk is very low, a close monitoring of the babies born to HIV infected women who wish to breastfeed is advised. The British HIV association 2018 guidelines also advise against breastfeeding but recommends support for women who wish to breastfeed only if the viral load is undetectable.
Breastfeeding is unquestionably an important human right and its benefits both on mother’s and child’s health are well proven and substantiated. On completely exploring the risks and benefits of breastfeeding in a HIV infected mother, the contraindication of breastfeeding for a women infected with HIV can be incomprehensible. Therefore, the emerging trend is to advise, encourage and support the decision of HIV infected mothers who really want to breastfeed but remain vague about the strategies that should be followed. There is a need to throw light and spread awareness in this regard.