Estimating the cost of delivering pre-exposure prophylaxis (prep) in preventing HIV-1 infections among adolescents and young people in an urban health center in Lusaka, Zambia
2 Department of Epidemology and Biostatistics, University of Zambia, Lusaka, Zambia
Received: 10-May-2024, Manuscript No. PULHPM-23-6418; Editor assigned: 12-May-2024, Pre QC No. PULHPM-23-6418 (PQ); Reviewed: 26-May-2024 QC No. PULHPM-23-6418; Revised: 31-Jul-2024, Manuscript No. PULHPM-23-6418 (R); Published: 08-Aug-2024, DOI: https://www.pulsus.com/scholarly-articles/estimating-the-cost-of-delivering-pree
Citation: Chileshe NN, Kaonga P, Chewe M, et al. Estimating the cost of delivering pre-exposure prophylaxis (prep) in preventing HIV-1 infections among adolescents and young people in an urban health center in Lusaka, Zambia. J Health Pol Manage 2023;6(2):15-21.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: There has been massive scale-up of HIV prevention interventions by the Zambian government especially among adolescents and young people. One such intervention is Pre-Exposure Prophylaxis (PrEP), and its implementation may hinge on the cost compared to the benefits. While most studies and reviews on PrEP have focused on cost-effectiveness, very few studies have been done on the cost of delivering PrEP in adolescents and young people. Such data are critically needed to guide national health policy in areas of preventing HIV/AIDS in adolescents and young people.
Methods: A cost analysis of PrEP using micro-costing or ingredients approach to estimate the required resources for effective PrEP among adolescents and young people data between October 2020 and September 2021. All expenditure data was collected from programmatic activity records at Kalingalinga Health Centre and all projected costs were obtained from Ministry of Health (MOH) implementation programme from a provider perspective. We estimated total and unit costs in 2021 United States Dollars (USD) from MOH reports. Data was analysed using a standardized cost collection template in Microsoft Excel-based format.
Results: The total number of the clients that accessed PrEP for the period under review October 2020 and September 2021, were 941 of which 64% (623/941) were adults and 34% (318/941) were Adolescents and Young People (AYP). Of the 318 AYP, 280/318 females were (88%) while males 38/318 (12%). The total annual program cost of providing PrEP at Kalingalinga health centre over 12 months of 941 clients was $200,964.99 and $67,913.57 for the AYP, with a unit cost of $213.57 per client-year. The main drivers of costs were PrEP medication, medical personnel salaries, and allowances, building and administrative/supervision costs, laboratory test kits and surgical materials respectively. The major cost component being 78.87% for PrEP medication, followed by building maintenance at 3.47%.
Conclusion: This study suggests that the annual program cost of implementing PrEP among AYP at Kalingalinga health center was$67,913.78. More analysis of the cost associated with other clinics, monitoring and technical support should be included to assess cost-effectiveness of delivering PrEP to adolescents and young people.
Keywords
HIV; Pre-exposure prophylaxis; Cost analysis; Adolescents and young people;
Introduction
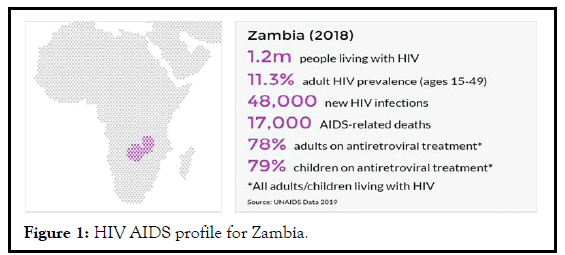
The Zambia national HIV and AIDS strategic framework 2017-2021 has recognised the need for (PrEP) to be provided to everyone or populations atrisk of HIV infection, in particular serodifferent couples and sex workers. However, it does not provide much guidance on how PrEP should be implemented and incorporated in the treatment guidelines for these target populations especially adolescents and young adults. National guidelines of implementing PrEP in risk target populations exist but its implementation is not linked to an enabling environment for certain key populations, which is currently lacking [1]. Figure 1 shows the prevalence of HIV in Zambia.
Figure 1: HIV AIDS profile for Zambia.
The prevalence of HIV stands at 11.3% in adults while in adolescents 7% [2]. Women, particularly adolescent girls and young women are worse affected than men. In 2017, 14.3% of women aged 15 and over were living with HIV, compared to 8.8% of their male counterparts. Data of HIV positive clients on ART at Kalingalinga health centre shows that 6.85% are adolescents and young people aged between 10 and 24 while 42% of young people are living with HIV (aged 15-24) at the national level. This is an indication that there is a need for scaling-up HIV preventative measures such as PrEP. These HIV preventative measures need to be made widely available and accessible to adolescents and young people at a larger scale so as to reduce the infection rate to zero.
In response to the fight against HIV, a number of preventive interventions have been implemented in Zambia and have shown positive impact in the reduction of HIV infection transmission. Today, more tools than ever have been made available to prevent HIV infections. People can use strategies such as abstinence; avoid sharing needles and condom use every time one is involved in sexual activities. People may also be able to take advantage of HIV preventive drugs such as PrEP and Post-Exposure Prophylaxis (PEP). If one has HIV, there are many actions they can take to prevent transmitting HIV to others. This is evidenced by a reduction in prevalence from 2007 (14%) to 2016 (11.3%) [3]. As a country, Zambia's response to the vice started with preventive interventions such as Voluntary Psychosocial Counseling and Testing (VCT) in the late 1990’s. The interventions later evolved to behaviour change, condom use, and treatment for prevention such as Prevention of Mother to Child Transmission (PMTCT) and Voluntary Medical Male Circumcision (VMMC).
Despite having put in place such interventions to curb the vice, there is very little information that indicates specific tailored HIV preventive interventions for adolescents and young people compared to adults and children [4]. Adolescents and young people account for over a quarter (27%) of the total population and have a significant influence on health trends [5]. About 32% of adolescents aged 15-17 and 60% of those aged 18-19 is sexually active in Zambia, and therefore face risks to HIV and other STIs, especially as only 40% of them report regular condom use. A related fact is that 42% of women aged 20-24 in Zambia report having been married by age 18.
While the understanding of some of the features of different prevention strategies is increasingly refined, very little information is available on the relative cost and likely impact of each intervention in different settings either individually or combined. Despite knowing the fact that resources are scarce, prioritization is desirable to facilitate decision-making, planning and resource allocation. By acknowledging the scale and magnitude of HIV/ AIDS in Zambia, good and sound allocation of limited and scarce resources for prevention is essentially critical for consistent implementation [6].
Cost evaluation and estimation is important in maintaining an adequate and timely supply of PrEP to the Adolescents and Young People (AYP) in Lusaka and possibly scale-up of such interventions to other provinces. The cost analysis will enable budget creation and management thus this study is necessary [7]. This study was necessary and timely in order to determine an estimate cost of delivering PrEP to adolescents and young people so as to help prevent the spread of HIV/AIDS. Kalingalinga health centre was chosen for the research due to its location and the population it caters for in terms of medical service delivery. Therefore, this study was aimed at finding out the estimated costs of delivering PrEP to adolescents and young people at Kalingalinga health centre.
Methods significance of the study
The findings generated from this study will help address issues of resource allocation amidst scarce and constrained resources to more cost-effective interventions for preventing HIV amongst adolescents and young people in Zambia. More information will further be used for identifying neglected interventions, redirecting resources to better use, maximise benefits and lead to improved health service delivery to better allocation of scarce resources. Furthermore, results will also enhance and inform policy makers and program managers to make decisions which are evidence based and of cost-effectiveness in nature.
Objective
General objective: To estimate the cost of providing PrEP treatment among adolescents and young people at Kalingalinga urban health centre in Lusaka, Zambia.
Specific objectives:
• To estimate the total cost of delivering PrEP treatment in preventing
HIV-1 among adolescents and young people at Kalingalinga urban
health centre in Lusaka, Zambia.
• To estimate the unit cost of providing PrEP treatment per client at
Kalingalinga urban health centre in Lusaka, Zambia.
• To estimate total number of adolescents and young people receiving
PrEP at Kalingalinga urban health centre in Lusaka, Zambia.
Materials and Methods
Study area and period
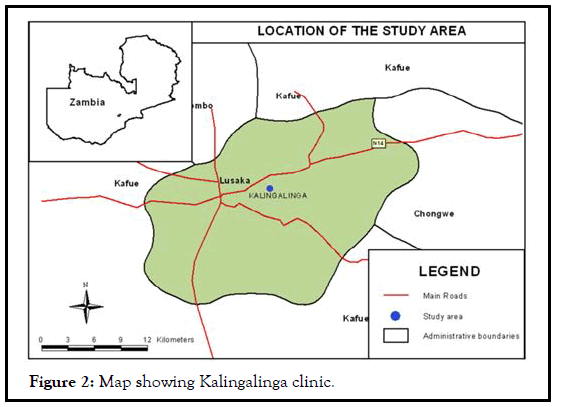
Kalingalinga township is one of the sub-districts of Lusaka district in Lusaka province, the capital city of Zambia. Lusaka district is divided into six sub-districts namely, Chelstone, Chipata, Matero, Kanyama, Chawama, and Chilenje. According to Zambia HMIS 2019, Kalingalinga has a population of 102,481. It is served with Kalingalinga health centre and several private health facilities within the catchment area shown in Figure 2.
The study was conducted at Kalingalinga health centre situated in Lusaka urban, Zambia. Kalingalinga health centre is one of the 22 health centres under the Lusaka District Health Office (LDHO) of the ministry of health. It has in-patient and out-patient facilities including Maternal and Child Health (MCH) and the ART clinic where the study was conducted. It has a catchment population of 56,491. The ART clinic handles HIV patients referred from the in-patient facilities, MCH and youth friendly corner as well as referrals from outside the health centre. Consultations in the ART clinic are done daily from Monday to Friday between 08:00 hours and 16:00 hours. Daily, clinicians attend to between 50 and 100 clients in the ART clinic. The study was conducted for a period of 12 months, from October 2020 to September 2021.
Study population
The study target population was all PrEP clients of HIV-1 exposure reported and recorded at the study site from October 2020 to September 2021.
Inclusion criteria
Data for all AYP aged between 10 to 24 years who sought PrEP services and had a HIV negative result during the period of study at Kalingalinga health centre in Lusaka were considered for study.
Exclusion criteria
All clients that were tested and found to be HIV positive were excluded from the study as they were referred for further management under the ART treatment programme. Children below the age of 10 and adults above the age of 24 who were on PrEP were not included in the study. Data for AYP before the study began and beyond (between October 2020 and September 2021) were also not considered for the study.
Cost analysis
Cost data was analysed in 2021 Microsoft excel (MS-excel). At the facility, the resources employed in delivering PrEP to clients were determined to help identify the cost for each service provided. The resources were then valued using information on their unit cost estimates and related parameters to generate total and driver costs. Average costs were estimated from provider perspective. All the costs were adjusted to 2021 USA dollar (US$) by using appropriate factors such as inflation rates and exchange rates where suitable. Provider’s costs were related to the costs incurred by the provider during any stage of the treatment process. Total annual provider’s costs included medical supplies, staff, building and equipment maintenance, equipment and buildings.
Table 1 show a description of fixed and variable costs while. Table 2 shows a description of direct and indirect costs of PrEP that were considered when calculating the cost of PrEP. Whether fixed or variable costs, costs are further categorised into direct or indirect costs and they make up the total cost. In this case the fixed and variable costs make up the total cost of the PrEP programme for the adolescents and young people at Kalingalinga health center.
| Fixed costs | Variable costs |
|---|---|
| Personnel salaries/allowances. | Clinical personnel salaries/allowances. |
| Medical doctors under CDC/partners. Clinical officers GRZ. Clinical officers under CDC/partners. Nurses GRZ. Nurses under CDC/partners. Pharmacist under GRZ. Pharmacist CDC. Treatment supporters. Under CDC/partner support. |
Weekend allowances for staff per month. |
| Drugs | |
| Emtricitabine/tenofovir (TDF/FTC) truvada subsidised. | |
| Laboratory testing. | |
| Lab costs creatinine per client (3 times a year), HIV, hepatitis, STI, liver and kidney function test number of HIV clinic visits within 12 months for those on prep. | |
| Other medical supplies. | |
| Surgical materials; gloves, needles for all clients. | |
| Building and administrative/supervision. | |
| Cleaners GRZ salary. Utility charges. Building costs. Building maintenance. Equipment costs. |
|
| Cleaning materials. |
Table 1: Fixed and variable categories of the main costs of PrEP.
| Direct costs | Indirect cost |
|---|---|
| Personnel salaries/allowances | Building and administrative/supervision |
| Medical doctors under CDC/partners | Exchange rate, Zambian kwacha to USD over year 2020-21 |
| Clinical officers GRZ | Cleaners GRZ salary |
| Clinical officers under CDC/partners | Utility charges |
| Nurses GRZ | Building costs |
| Nurses under CDC/partners | Building maintenance |
| Pharmacist under GRZ | Equipment costs |
| Pharmacist CDC | Cleaning materials |
| Treatment supporters under CDC/partner support | |
| Weekend allowances for staff per month | |
| Drugs | |
| Emtricitabine/tenofovir (TDF/FTC) truvada subsidized | |
| Laboratory testing | |
| Lab costs creatinine per client (3 times a year) HIV, hepatitis, STI, liver and kidney function test number of HIV clinic visits within 12 months for those on prep | |
| Other medical supplies | |
| Surgical materials; gloves, needles for all clients | |
| Specimen containers for all clients |
Table 2: Direct and indirect categories of the main costs of PrEP.
Data collection
Cost data: Data collection took place from October 2020 to September 2021 at Kalingalinga urban health centre in Lusaka, Zambia through e-Data which was obtained from experts handling the HIV program, based on MOH reports and consultation from MOH officials. Retrospective financial costs and client’s data were collected simultaneously. Costs of HIV testing and PrEP services were collected by programmatic activity (HIV testing and counselling, PrEP initiation and PrEP visit, adherence counselling, physical check, clinic visit, prescribing drugs and blood draw), by input type (personnel, drugs and commodities, supplies, test kits, laboratory testing including creatinine, hepatitis B, syphilis screening, biochemistry and haematology), and by source of support. Quantitative data were analysed using Microsoft excel in the local currency Zambian kwacha (ZMW) and converted to US dollar.
The programme implementation data were used to calculate the cost for delivering the intervention and the results were used to interpret the findings and identify the cost of delivering the intervention. The costs were estimated from the provider perspective and they focused on expenditure costs which included PrEP medication, medical supplies, clinic staff salaries and allowances, and facility overheads. The total annual cost of delivering PrEP service was calculated as the total cost divided by the number of clients. The average cost (unit) per client-month of PrEP was calculated as the total annual cost divided by the total number of months of PrEP coverage. The annualised cost of capital goods was discounted at the rate of 3% and assumed a life of 5 years for all capital goods. Since building costs were not available, we approximated the cost of the clinic based on construction costs and the area (calculated at $ 350 per m2 based of experts from MOH which was annualized at a rate of 3% with a life of 20 years). Land cost was not included in the cost estimation.
Data analysis: We estimated the annual cost of delivering oral PrEP to AYP enrolled in a PrEP programme located in Kalingalinga health centre, in Lusaka Zambia. Kalingalinga health centre is located in Lusaka assuming the service was provided throughout the period of study. We estimated 941 client resource use based on these guidelines from the day of PrEP initiation for 12 months, 318 adolescents and young adults assuming continuous PrEP use for the duration. These direct service delivery costs included drugs, laboratory tests, and medical supplies. Assuming full adherence to guidelines, we then applied the unit costs to the resources expected to be used over the 12 months period.
The youth friendly spaces are dedicated to AYP who need PrEP and other HIV/AIDS related services. The study derived total annual costs and the average cost per client-month of PrEP by input type (variable or fixed) and visit type (initiation or follow-up). The estimation of all costs was done as implemented in the programme and under implementation by the Zambian Ministry of Health (MOH), both at the program volume observed and if the facilities were delivering PrEP at full capacity (scaled by MOH). Data entry and analysis were done using Microsoft Excel and costs converted to US dollars (2021).
The study conducted a retrospective cost analysis of PrEP from October 2020 to September 2021 (12 months period) to derive the cost associated with HIV testing and PrEP services from a provider’s perspective. To calculate personnel costs, information collected from the facility and project staff on their salaries and allowances, and assumed staff worked eight hours per day for 20 days each month. The cost of supplies and equipment associated with laboratory testing was based on price per test using the ministry of health costings. The cost of drugs and commodities was determined by multiplying the MOH unit price with the quantities used.
Operational definition
Adolescent: An individual between 10-19 years age group.
Young youth or people: As an individual between the 15–24 years age group.
Pre-exposure Prophylaxis (PrEP): Is medicine that people at risk of contracting HIV take before having sex (time before sex) to prevent getting HIV from unprotected sex or injection drug use [8].
Cost of the product is equal to the acquisition price of the product, including the costs of financing minus depreciation. The accounting cost of a health service is its costs estimated by a cost allocation report. It encompasses direct and indirect costs [9].
Cost analysis: This is the process of evaluation that focuses on the costs of implementing a program regards to the ultimate outcome [10].
Cost per unit/average: cost of goods sold or the cost of sales is how much money a company spends on producing one unit of the product they sell.
Direct costs: Are costs which can be traced to the finished products manufactured. In other words, a relationship can be established between costs and finished products manufactured.
Indirect costs: Are costs which cannot be traced to the finished products manufactured. They are also known as overheads. Overheads can be apportioned/distributed to the finished product.
Variable cost: Is an expense that changes in proportion to how much a company produces or sells. Variable costs increase or decrease depending on a company's production or sales volume they rise as production increases and fall as production decreases. It can be contrasted with a fixed cost.
Fixed cost: Are expenses that are not dependent on the level of goods or services produced by the business (indirect or overhead cost). They tend to be recurring, such as interest or rents being paid per month.
Total cost: Is the sum of all the fixed and variable costs associated with a particular scale of provision of a programme or intervention. The greater the scale of provision, the larger will be the total costs.
Results
PrEP outcomes
Table 3 presents PrEP outcome for the period under review, October 2020 to September 2021. The total number of clients on PrEP was 941 of which 64% (623/941) were adults and 34% (318/941) were Adolescents and Young People (AYP). The definition of adolescents and young people is an individual between 10–24 years age group. Therefore, 318 clients were eligible for calculation of cost of providing PrEP for AYP, 280/318 (88%) were females and 38/318 (12%) males.
| Age group (years old) | Female | Male | Total |
|---|---|---|---|
| 10-14 | 0 | 4 | 4 |
| 15-19 | 69 | 13 | 82 |
| 20-24 | 211 | 21 | 232 |
| 25+ | 521 | 102 | 623 |
| Total | 801 | 140 | 941 |
Table 3: PrEP outcomes.
Cost analysis
Table 4 the total cost for providing PrEP was calculated at $200,964.99 with fixed and variable costs $33,706.57 and $167,258.42 respectively. The main cost component being drug provision at $158,507.55 (78.87%) and the remaining was apportioned building maintenance $6,668.64 (3.4%) and medical personnel at $5,895.77 (2.93%).
| Cost input | Number of people on PrEP | ZMW | US$ | Cost per person on PrEP (US$) | Proportion (%) |
|---|---|---|---|---|---|
| Fixed costs | |||||
| Medical personnel | 941 | 101,525.08 | 5,895.77 | 6.27 | 2.93% |
| Treatment supporters | 941 | 9,697.00 | 563.12 | 0.6 | 0.28% |
| Support staff | 941 | 84,000.00 | 4,878.05 | 5.18 | 2.43% |
| Utility charges | 941 | 36,000.00 | 2,090.59 | 2.22 | 1.04% |
| Building maintenance | 941 | 120,000.00 | 6,968.64 | 7.41 | 3.47% |
| Cleaning materials | 941 | 72,000.00 | 4,181.18 | 4.44 | 2.08% |
| Building and facilities | 941 | 81,022.00 | 4,705.11 | 5 | 2.34% |
| Equipment | 941 | 76,183.00 | 4,424.10 | 4.7 | 2.20% |
| Total fixed cost | 580427.08 | 33,706.57 | 35.82 | 16.77% | |
| Variable costs | |||||
| Laboratory test | 941 | 84,690 | 4,918.12 | 5.23 | 2.45% |
| Medical supplies | 941 | 66,000 | 3,832.75 | 4.07 | 1.91% |
| Drugs | 941 | 2,729,500 | 158,507.55 | 168.45 | 78.87% |
| Total variable costs | 2,880,190.00 | 167,258.42 | 177.75 | 83.23% | |
| Total costs | 3,460,617.08 | 200,964.99 | 213.57 | 100.00% | |
Table 4: Fixed and variable costs.
The Table 5 shows direct and indirect costs that were used for apportionment of the overhead costs which include personnel salaries and allowances, laboratory testing and medical supplies. The total indirect and direct costs were calculated at US$ 27,247.68 and US$ 173,717.31, respectively. Direct cost taking the largest proportion of 86.44% and indirect cost at 13.56%.
| Cost input | Number of people on PrEP | ZMW | US$ | Cost per person on PrEP (US$) | Proportion (%) | |
|---|---|---|---|---|---|---|
| Indirect costs | ||||||
| Cleaners GRZ salary | 941 | 84,000.00 | 4,878.05 | 5.18 | 2.43% | |
| Cleaning materials | 941 | 72,000.00 | 4,181.18 | 4.44 | 2.08% | |
| Building maintenance | 941 | 120,000.00 | 6,968.64 | 7.41 | 3.47% | |
| Utility charges | 941 | 36,000.00 | 2,090.59 | 2.22 | 1.04% | |
| Building cost | 941 | 81,022.00 | 4,705.11 | 5 | 2.34% | |
| Equipment cost | 941 | 76,183.00 | 4,424.10 | 4.7 | 2.20% | |
| Sub-total | 469,205.00 | 27,247.68 | 28.96 | 13.56% | ||
| Direct costs | ||||||
| Medical personnel | 941 | 101,525.08 | 5,895.77 | 6.27 | 2.93% | |
| Volunteer time | 941 | 9,697 | 563.12 | 0.6 | 0.28% | |
| Laboratory supplies | 941 | 84,690 | 4,918.12 | 5.23 | 2.45% | |
| Medical supplies | 941 | 66,000 | 3,832.75 | 4.07 | 1.91% | |
| Drugs | 941 | 2,729,500 | 158,507.55 | 168.45 | 78.87% | |
| Sub-total | 2,991,412.08 | 173,717.31 | 184.61 | 86.44% | ||
| Total | 3,460,617.08 | 200,964.99 | 213.57 | 100.00% | ||
Table 5: Indirect and direct costs.
Table 6 describes a summary of the total annual program cost of providing PrEP to AYP at Kalingalinga health centre. A total number of clients that accessed PrEP were 941 of which 318 were AYP aged between 10 and 24 years old. The total annual cost for delivering PrEP to the AYP was $67,913.78 was the annual unit cost per client-year for providing PrEP was $213.57 for the entire population that accessed the service.
| Cost item | Total cost of PrEP for AYP | |||
|---|---|---|---|---|
| Cost per person on PrEP (US$) | Number of people on PrEP | ZMW | US$ | |
| Indirect costs | ||||
| Support staff | 5.18 | 318 | 28,386.82 | 1,648.48 |
| Cleaning materials | 4.44 | 318 | 24,331.56 | 1,412.98 |
| Building maintenance | 7.41 | 318 | 40,552.60 | 2,354.97 |
| Utility charges | 2.22 | 318 | 12,165.78 | 706.49 |
| Building cost | 5 | 318 | 27,380.44 | 1,590.04 |
| Equipment cost | 4.7 | 318 | 25,745.16 | 1,495.07 |
| Sub-total | 28.96 | 158,562.37 | 9,208.04 | |
| Direct costs | ||||
| Medical personnel | 6.27 | 318 | 34,309.22 | 1,992.41 |
| Volunteer time | 0.6 | 318 | 3,276.99 | 190.3 |
| Laboratory supplies | 5.23 | 318 | 28,620.00 | 1,662.02 |
| Medical supplies | 4.07 | 318 | 22,303.93 | 1,295.23 |
| Drugs | 168.45 | 318 | 922,402.76 | 53,565.78 |
| Sub-total | 184.61 | 1,010,912.90 | 58,705.74 | |
| Total | 213.57 | 1,169,475.27 | 67,913.78 | |
Table 6: Total annual program cost of PrEP for adolescents and young people.
Discussion
We estimated the annual program total costs of delivering oral PrEP to clients as part of integrated HIV and SRH services at Kalingalinga health center. Total annual program costs of PrEP for the ATP (318) were $67,913.78 and unit of cost of $213.57 for all the 941 clients that accessed the PrEP program. AYP represented about 34% of the total 941 clients on PrEP. The estimated total annual cost of providing PrEP to one (1) $213.57 per year. The major cost component was attributable to PrEP medication $53,565.78 (78.87%), followed by building maintenance $6,968.64 (3.4%) and medical personnel (2.93%).
Like other PrEP programs in sub-Saharan Africa, our study revealed that the most contributing costs were attributed by the PrEP drug seconded by administrative coordinating costs. Recent data from Zimbabwe showed that the total annual PrEP program costs were $1,113,430 across the seven sites, with recurrent costs contributing 93% ($1,036,199) of the cost, personnel was one-third of the cost. For the PSI sites, demand creation including mobilizer costs contributed 27% to the cost and PrEP drugs 9%. For the government SGBV clinic, the largest cost (25%) was the PrEP drug 25%. The average cost per person initiated on PrEP was $238, ranging from $183 at the largest PSI facility in Harare to $302 at the small clinic in a medium size town and $86 at the government SGBV clinic. While from the Kenyan study, in their first year of programmatic PrEP delivery in 25 HIV-1 care clinics, 2,567 persons were initiated on PrEP and covered 8,847 total months of PrEP coverage, accounting for 2 % of total outpatient clinic visits. The total financial cost to the Ministry of Health was $91,175, translating to an average of $10.31 per person per month. The majority of the financial cost were attributable to PrEP medication (69), followed by administrative supplies (17 %) and training (9%).
Our study was not much different from other studies in the region as estimates showed that the average cost per person in the region to access PrEP was between $10 to $24 per monthly and $183 to $238 annually respectively. While the major contributing costs in providing PrEP was attributable to the PrEP drug cost and followed by personnel cost.
Conclusion
The ART clinic at Kalingalinga health centre offers a potential PrEP delivery platform to efficiently reach large numbers of adolescents and young people at risk in HIV burden settings. Prioritising more investment in PrEP delivery in AYP would significantly reduce the cost of drugs. Further specific costing studies with similar settings are needed to evaluate the costs of delivering PrEP. Cost-effectiveness studies of PrEP scale-up need context-specific costing data in order to effectively and accurately informs policy.
The study estimated the cost of providing PrEP to AYP from 10 to 24 years old at $67,913.78 annually while the cost for the entire population of 941 clients was $200,964.99 for delivering PrEP service at Kalingalinga health centre. The estimated value of providing PrEP to one (1) adolescent per year was $213.56. In a practical implementation setting, we estimated the cost of PrEP delivery among AYP at Kalingalinga health centre and the results indicated that the major cost driver for delivering PrEP were the drugs. In all scenarios, medication was the main contributor of total annual costs, highlighting the need to find ways to lower the price of drugs (Emtricitabine/Tenofovir (TDF/FTC) Truvada) used in PrEP would inform budget impact and cost effectiveness analysis to maximise health outcomes for the resources available.
Limitations
This analysis has several limitations. First, our estimates of costs determined were only done for total and average cost for providing PrEP. The establishment of the cost drivers was not considered during analysis, but it is one important aspect of determining what contributes to the cost of delivering the service which can be considered for further studies. Secondly, the cost estimates presented here are based on annual PrEP enrolment of approximately 318 at one facility, accounting for approximately 34% of total client volume. In this setting, the additional work burden was readily absorbed by existing staff and facilities; as such, we did estimate the economic cost of components such as building rental and supervision, as the proportional allocation of these existing resources to PrEP would was shared with the ART clinic. While we assume that reallocation of time to PrEP delivery does not impact ART delivery, the true opportunity cost of staff time is uncertain, and future analyses of the net cost of PrEP provision should account for any changes to ART delivery. Thirdly, lack of dedicated staff to PrEP programme specifically for adolescents and young people difficult to accurately collection and interpretation very difficult data as provided data was for all the PrEP clients, regardless of their age. Lastly, other costs such as training, mobilisation and sensitisation on PrEP were not made available therefore, they were not included in the analysis. Nevertheless, PrEP implementation remains a relatively new service, and program modifications in the future are likely. Despite these limitations the study shows some positive worthiness in improving the service delivery of PrEP. First, the study used primary data, which can be adaptive in costing PrEP in the national policy in Zambia. Second, the study findings compare relatively well with findings from other literature. The study by case and others, son cost-effectiveness of PrEP as a treatment intervention, showed that PrEP could be effective in averting HIV if programmatic information could be updated as well as ex post modelling to evaluate and inform efficient deployment of resources in support of PrEP, especially among key populations, using direct evidence of cost, adherence and uptake patterns. This was the closest paper done on economic assessment from Zambia, but the results were based on modelling.
Therefore, the findings from this study form the basis for economic evaluation of costing the delivery of PrEP in AYP and suggest future economic analysis of PrEP interventions for further scaling-up in Zambia. However, cost analysis findings should be interpreted with caution as they may not present the economic cost because perspective costs analysis did not other primary calculation of overheads, training, mobilization, sensitisation and facility administration costs as calculated in other studies. Cost estimates should be periodically updated to reflect such changes to maintain accurate budget impact and cost-effectiveness estimates to facilitate program scale-up in other similar settings.
Ethical considerations
Ethical approval (UNZABREC) granted permission to conduct research within Zambia using secondary data. Collection of data was done after approval was granted from UNZABREC to collect data from various owners of dataset, organisations such as NAC, ministry of health and other organisations involved in the implementation of interventions. Confidentiality was maintained and only shared among the research team and there was minimal risk to data leaking to third persons. No consent form was required of participants as the data that was used was collected from the health centre database which was anonymous and de-identified.
Recommendations
Further studies in other health centres should be considered to build a standard cost for providing PrEP to AYP and lowering the cost of PrEP drug in delivering the service in urban health centres.
Further in research, there is need to carry out similar studies in costing interventions in delivering health care services as such and a larger sample size can be implored to improve on the power of the study.
Availability of Data
Data is found with a corresponding author and any one can find it by requesting.
Conflict of Interest
Authors revealed that there has not been a conflict of interest.
Authors' Contributions
Authors added contributions based on their work divisions for producing this research article.
References
- Walker D. Cost and cost-effectiveness of HIV/AIDS prevention strategies in developing countries: is there an evidence base?. Health Policy Plan. 2003;18(1):4-17.
[Crossref] [Google Scholar] [PubMed]
- Centers for Disease Control and Prevention. Compendium of evidence-based interventions and best practices for HIV prevention. Atlanta, GA: Author. 2014.
- Johns B, Baltussen R, Hutubessy R. Programme costs in the economic evaluation of health interventions. Cost Eff Resour Alloc. 2003;1(1): 1-10.
[Crossref] [Google Scholar] [PubMed]
- Oostenbrink JB, Koopmanschap MA, Rutten FF. Standardisation of costs: the Dutch Manual for Costing in economic evaluations. Pharmacoeconomics. 2002;20(7):443-54.
[Crossref] [Google Scholar] [PubMed]
- Peebles K. Low costs and opportunities for efficiency: A cost analysis of the first year of programmatic PrEP delivery in Kenya’s public sector. BMC Health Serv Res. 2021;21(1):1-8.
[Crossref] [Google Scholar] [PubMed]
- Mangenah C, Nhamo D, Gudukeya S, et al. Efficiency in PrEP delivery: estimating the annual costs of Oral PrEP in Zimbabwe. AIDS Behav. 2022;26(1):161-70.
[Crossref] [Google Scholar] [PubMed]
- Nagot N. Extended pre-exposure prophylaxis with lopinavir–ritonavir versus lamivudine to prevent HIV-1 transmission through breastfeeding up to 50 weeks in infants in Africa (ANRS 12174): a randomised controlled trial. Lancet. 2016;387(10018):566-73.
[Crossref] [Google Scholar] [PubMed]
- Hensen B, Phiri M, Schaap A, et al. Yathu Yathu (For us, by us): Design of a cluster-randomised trial of the impact of community-based, peer-led comprehensive sexual and reproductive health services for adolescents and young people aged 15 to 24 in Lusaka, Zambia. Contemp Clin Trials. 2021;110:106568.
[Crossref] [Google Scholar] [PubMed]
- Kasaro MP, Sindano N, Chinyama M, et al. Integration of HIV Prevention with sexual and Reproductive Health Services: evidence for Contraceptive Options and HIV Outcomes Study experience of integrating oral pre-exposure HIV Prophylaxis in Family Planning Services in Lusaka, Zambia. Front Reprod Health. 2021;13(3):684717.
[Crossref] [Google Scholar] [PubMed]
- Chang LW, Serwadda D, Quinn TC, et al. Combination implementation for HIV prevention: moving from clinical trial evidence to population-level effects. Lancet Infect Dis. 2013;13(1):65-76.
[Crossref] [Google Scholar] [PubMed]