Gender and service utilization in adolescents with drug abuse and suicidality: Epidemiology and clinical considerations
Received: 15-Sep-2017 Accepted Date: Oct 16, 2017; Published: 20-Oct-2017
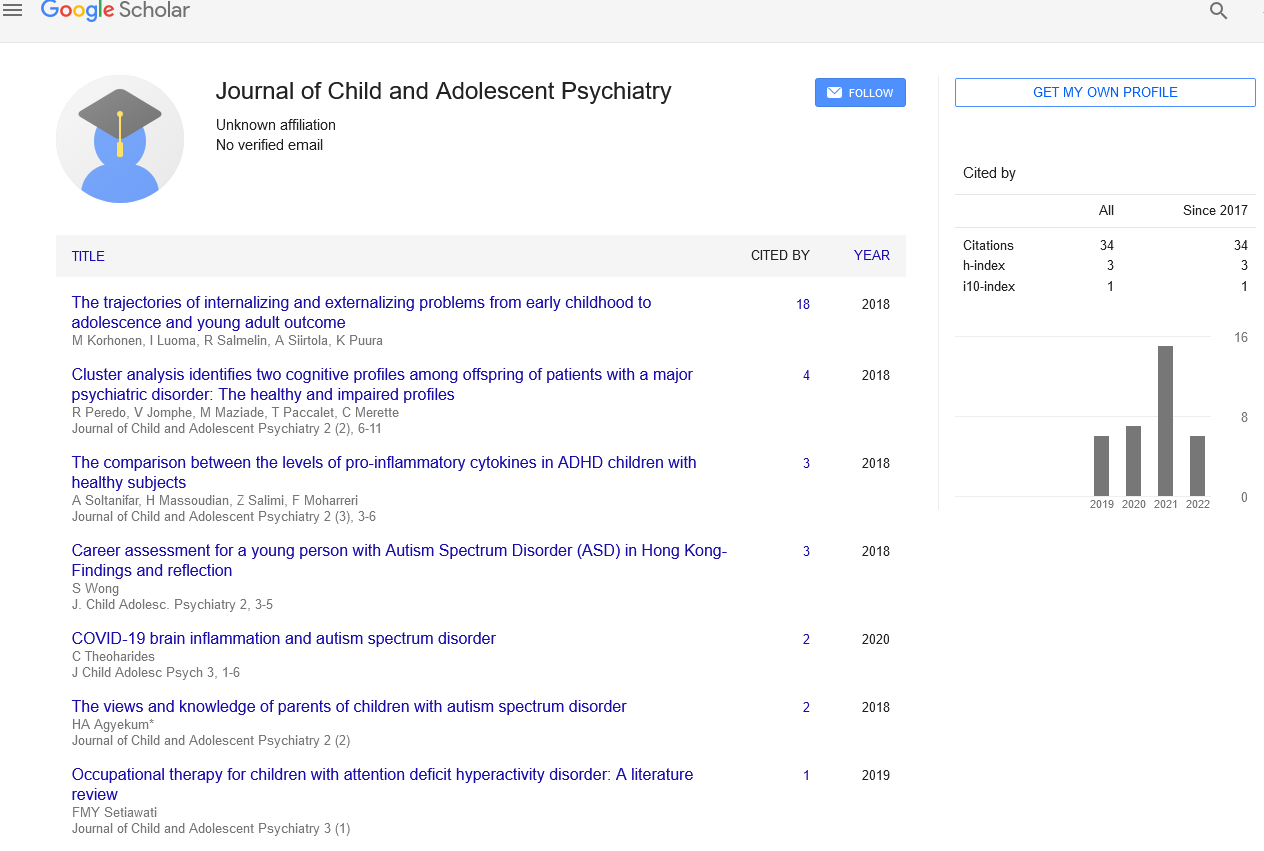
Citation: Comacchio C. Gender and service utilization in adolescents with drug abuse and suicidality – epidemiology and clinical considerations 2017;1(1):1-3.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Drug abuse and depression are common among adolescents and they can lead to several adverse consequences that range from school dropout and social isolation to suicide, which is the second leading cause of death among young people. Adolescents are reluctant to seek help for psychiatric problems and this may have fatal consequences. The present article explores gender differences in service utilization in adolescents with drug abuse and suicidality. An awareness of these differences may help clinicians and policymakers to develop and implement tailored-made strategies for adolescents in need of psychiatric help.
Keywords
Gender differences; Mental health service use; Drug abuse; Adolescents; Suicidality; Depression
Introduction
It has been estimated that nearly half of all psychiatric disorder onset before age 21 [1]. However, adolescents with mental disorders cannot seek help from specialized services without parental involvement and tend to be reluctant to attend regular visits once their problem is revealed [2- 5], which may lead to low rates of clinical counselling [6-8]. Furthermore, adolescents present difficulties in service engagement and are at more risk of an early treatment drop-out [9]. Despite the importance of detecting and engaging adolescents in need of psychiatric help in the early phases of their disturbances, literature on this field is scarce. For long time males and females affected by mental disorders have been seen as a homogeneous group, with similar characteristics, needs for care and outcomes [10]. However, males and females differ in relation to prevalence, impact of biological, psychological and social factors and course of illness [11] and these differences have to be carefully taken into account when planning patient-tailored interventions [12]. Gender-centred approaches emphasize the importance of social cultural and biological differences on health, thus ensuring the best outcomes for men and women with mental health problems [11]. In addition, they can improve detection and treatment of mental health problems in underreported groups; provide additional evidence in epidemiology and course of mental disorders; improve relevance of health services and increase patients’ participation in health [10]. Understanding gender differences in mental health services utilization appears thus crucial in the development of tailored policies, in the implementation of existing services and in the provision of more effective treatments for young people with psychiatric disorders.
Among adolescents substance abuse is common, with 22% of young people drinking alcohol weekly [13] and up to 33% having tried at least one illicit drug [14]. Female patients show lower rates of substance abuse problems than males [15,16] but they tend to develop dependence faster [17,18]. Despite lower levels of substance abuse, females with addictive behaviours present poorer general physical health [19], higher rates of victimization [20,21] and partner conflict [19], more stress-related substance abuse [22] and more psychiatric problems than males [15-29]. On the other hand, males with substance abuse show higher rates of criminal activities than females [19,21,28,30]. With regard to the type of drug used, female patients are more likely to use heroine [22,31,32] and more likely to share injecting equipment than males [22,30,31], whereas male patients are more likely to use cannabis and alcohol than females [22,33]. Emergency Departments are often the primary site for evaluation of adolescents with substance abuse problems [23, 34], particularly for male abusers [23,34,35], but the nature of the contact (acute intoxication, difficulties in bonding, issues of confidentiality) makes it difficult for clinicians to refer patients to adequate treatment programs [36]. Once the addiction is recognized, adolescents can be addressed to outpatient services, which can offer Mixed-Gender (MG) or Women Only (WO) programs. WO programs utilize a more supportive and less confrontational approach to treatment than MG programs [37], which is more suitable for females, who are more expressive verbally and behaviourally in singlesex group sessions [38]. The treatment of choice should rely on patient’s preference, taking into consideration that WO programs may provide a more adequate environment for female adolescents with substance abuse problems.
As previously stated, substance abuse in young people is often complicated by mental health problems [15,19-21,23-29], among which depression is the one of the most common [35,39]. However, depression in adolescents with or without substance abuse is frequently undetected and untreated by clinicians [8,40]. Depression is linked with suicide, which is the second leading cause of death among people between 15 and 18 years old and a major global public health problem [41,42]. Up to 90% of adolescents who commit suicide have at least one diagnosable mental disorder at the time of their death being depression and substance abuse the most common [43-45]. Female patients are more likely to suffer from depression and to attempt suicide than males, who, conversely, are four times more likely to complete suicide than females [46]. Male adolescents are also less likely to express suicidality prior to attempting suicide and more likely to use lethal means [46]. Despite the great concern about suicidality in adolescents, it has been estimated that only 15% of suicide completers had received psychiatric visits in the 90 days prior to suicide while 28% in the 12 months before suicide [47], but data are not entirely consistent and rates of psychiatric assessments in adolescents who completed suicide are likely to be lower [48,49]. Female patients with suicidality are more likely to be referred to specialized services by GPs [50] and they tend to have higher contacts with mental health services in the month prior to suicide [6,50].
Despite the body of evidence on the importance of gender differences in adolescents with drug abuse and suicidality, gender-sensitive mental health services are more of a chimera in the majority of EU countries [51,52]. Providing adequate mental health care to adolescents is challenging but a priority and the present study highlights an important gap in literature on gender and pathways to care in young people with mental health problems. Gender is a critical variable to be taken into consideration both by clinicians and policy makers when developing and implementing services for adolescents with mental health problems.
Disclosures
The author declare no conflicts of interest.
REFERENCES
- Kessler RC, Angermeyer M, Anthony JC, et al. Lifetime prevalence and age of onset distributions of mental disorders in the World Health Organization’s World Mental Health Surveys. World Psychiatry. 2007;6(3):168–76.
- Benjet C, Borges G, Mendez E, et al. Eight‑year incidence of psychiatric disorders and service use from adolescence to early adulthood: longitudinal followup of the Mexican Adolescent Mental Health Survey. Eur Child Adolesc Psychiatry. 2016;25(2):163–73.
- Wu P, Hoven CW, Bird HR, et al. Depressive and disruptive disorders and mental health service utilization in children and adolescents. J Am Acad Child Adolesc Psychiatry. 1999;38(9):1081–90.
- Rickwood DJ, Deane FP, Wilson CJ: When and how do young people seek professional help for mental health problems? Med J of Aust 2007;187(7):S35–S39.
- Linsley KR, Johnson N, Martin J: Police contact within 3 months of suicide and associated health service contact. Br J of Psychiatry 2007;190(2):170–1.
- Yu JW, Adams SH, Burns J, Brindis CD, Irwin CE Use of mental health counseling as adolescents become young adults. J Adolesc Health 2008;43(3):268–76.
- Kataoka SH, Zhang L, Wells KB. Unmet need for mental health care among us children: variation by ethnicity and insurance status. Am J Psychiatry. 2002;159(9):1548 –55.
- Kessler RC, Avenevoli S, Ries Merikangas K. Mood disorders in children and adolescents: an epidemiologic perspective. Biol Psychiatry 2001;49(12):1002–14.
- Johnson E, Mellor D, Brann P. Differences in dropout between diagnoses in child and adolescent mental health services. Clin Child Psychol Psychiatry. 2008;13(4):515-30.
- Vlassoff C, Garcia Moreno C. Placing gender at the centre of health programming: Challenges and limitations. Social Science & Medicine 2002;54(11):1713–23.
- Judd F, Armstrong S, Kulkarni J. Gender-sensitive mental health care. Australas Psychiatry. 2009;17(2):105-11.
- McCormack B, Karlsson B, Dewing J, et al. Exploring person-centredness: A qualitative metasynthesis of four studies. Scand J Caring Sci 2010;24(3):620–63.
- National Drug Strategy Household Survey: first results. Australian Institute of Health and Welfare. 2007 Drug Statistics Series number 20. Cat. no. PHE 98. Canberra: AIHW, 2008.
- White V, Hayman J. Australian secondary school students’ use of over-the-counter and illicit substances in 2005. Canberra: Drug Strategy Branch, Australian Government Department of Health and Ageing, 2006.
- Florsheim P, Moore DR. Observing differences between healthy and unhealthy adolescent romantic relationships: substance abuse and interpersonal process. J Adolesc. 2008;31(6):795–814.
- Teesson M, Baillie A, Lynskey M, et al. Substance use, dependence and treatment seeking in the United States and Australia: a cross-national comparison. Drug Alcohol Depend. 2006;81(2):149-55.
- Hser YI, Anglin MD, Booth MW. Sex differences in addict careers. 3. Addiction. Am J Drug Alcohol Abuse. 1987;13(3):231–51.
- Anglin MD, Hser YI, McGlothlin WH. Sex differences in addict careers. 2. Becoming addicted. Am J Drug Alcohol Abuse. 1987;13(1-2):59–71.
- Spooner C, Mattick RP, Noffs W. A study of the patterns and correlates of substance use among adolescents applying for drug treatment. Aust N Z J Public Health. 2000;24(5):492–502.
- Hussey DL, Drinkard AM, Falletta L, et al. Understanding clinical complexity in delinquent youth: comorbidities, service utilization, cost, and outcomes. J Psychoactive Drugs. 2008;40(1):85–95.
- Toray T, Coughlin C, Vuchinich S, et al. Gender differences associated with adolescent substance abuse: comparisons and implications for treatment. Fam Relat. 1991;40(3):338–44.
- Dean A, McBride M, McDonald E, et al. Gender differences in adolescents attending a drug and alcohol withdrawal service Drug. Alcohol Rev. 2010;29(3):278–85.
- Fahimi J, Aurrecoechea A, Anderson E, et al. Substance Abuse and Mental Health Visits Among Adolescents Presenting to US Emergency Departments. Pediatr Emer Care. 2015;31(5): 331–8.
- Brook JS, Richter L, Rubenstone E. Consequences of adolescent drug use on psychiatric disorders in early adulthood. Ann Med. 2000;32(6):401–7.
- Rodham K, Hawton K, Evans E, et al. Ethnic and gender differences in drinking, smoking and drug taking among adolescents in England: a self-report school-based survey of 15 and 16 year olds. J Adolesc. 2005;28(1):63–73.
- Milne B, Bell J, Lampropoulos B, et al. Alcohol, drugs and Australian young people. Int J Adolesc Med Health. 2007;19(3):245–53.
- Marsden J, Gossop M, Stewart D, et al. Psychiatric symptoms among clients seeking treatment for drug dependence. Intake data from the National Treatment Outcome Research Study. Br J Psychiatry. 2000;176(3):285–9.
- Rowan-Szal GA, Chatham LR, Joe GW, et al. Services provided during methadone treatment. A gender comparison. J Subst Abuse Treat. 2000;19(1):7–14.
- Mills KL, Teesson M, Darke S, et al. Young people with heroin dependence: findings from the Australian Treatment Outcome Study (ATOS). J Subst Abuse Treat. 2004;27(1):67–73.
- Evans JL, Hahn JA, Page-Shafer K, et al. Gender differences in sexual and injection risk behavior among active young injection drug users in San Francisco (the UFO Study). J Urban Health 2003;80(1):137–46.
- Montgomery SB, Hyde J, De Rosa CJ, et al. Gender differences in HIV risk behaviors among young injectors and their social network members. Am J Drug Alcohol Abuse 2002;28(3):453–75.
- Copeland J, Howard J, Keogh T, et al. Patterns and correlates of substance use amongst juvenile detainees in New SouthWales 1989–99. Drug Alcohol Rev. 2003;22(1):15–20.
- Hser YI, Evans E, Huang YC. Treatment outcomes among women and men methamphetamine abusers in California. J Subst Abuse Treat. 2005;28(1):77–85.
- Case SD, Case BG, Olfson M, et al. Length of stay of pediatric mental health emergency department visits in the United States. J Am Acad Child Adolesc Psychiatry. 2011;50(11):1110–9.
- Sartor CE, Lynskey MT, Heath AC, et al. The role of childhood risk factors in initiation of alcohol use and progression to alcohol dependence. Addiction. 2007;102(2):216–25.
- Mabood N, Ali S, Dong KA, et al. Experiences of pediatric emergency physicians in providing alcohol-related care to adolescents in the emergency department. Pediatr Emerg Care. 2013;29(12):1260–5.
- Grella CE, Polinsky ML, Hser YI, et al. Characteristics of women-only and mixed-gender drug abuse treatment programs. J Subst Abuse Treat. 1999;17(1-2):37-44.
- Hodgins DC, el-Guebaly N, Addington J. Treatment of substance abusers: single or mixed gender programs? Addiction. 1997;92(7):805-12.
- Whitesell M, Bachand A, Peel J, et al. Familial, social, and Individual factors contributing to risk for adolescent substance use. J Addict. 2013;2013:579310.
- Wang PS, Berglund P, Kessler RC. Recent care of common mental disorders in the United States: Prevalence and conformance with evidence-based recommendations. J Gen Intern Med. 2002;15(5):284-92.
- Bridge JA, Goldstein TR, Brent DA. Adolescent suicide and suicidal behavior. J Child Psychol Psychiatry. 2006;47(3-4);372–94.
- Pelkonen M, Marttunen M. Child and adolescent suicide: epidemiology, risk factors, and approaches to prevention. Paediatr Drugs. 2003;5(40):243–65.
- Brent DA, Perper JA, Moritz G, et al. Psychiatric risk factors for adolescent suicide: a case-control study. J Am Acad Child Adolesc. Psych. 1993;32(3):521–29.
- Brent DA, Johnson BA, Perper J, et al. Personality disorder, personality traits, impulsive violence, and completed suicide in adolescents. J Am Acad Child Adolesc Psych. 1994;33(8):1080–6.
- Renaud J, Berlim MT, McGirr A, et al. Current psychiatric morbidity, aggression/impulsivity, and personality dimensions in child and adolescent suicide: a case-control study. J Affect Disord. 2008;105(1-3):221–8.
- Gould MS, Greenberg T, Velting DM, et al. Youth suicide risk and preventive interventions: A review of the past 10 years. J Am Acad Child Adolesc Psychiatry. 2003;42(4):1–20.
- Renaud J, Chagnon F, Balan B, et al. Psychiatric services utilization in completed suicides of a youth centres population. BMC Psychiatry. 2006;6(1):36.
- Moskos MA, Olson L, Halbern SR, et al. Utah youth suicide study: barriers to mental health treatment for adolescents. Suicide Life- Threat Behav. 2007;37(2):179–86.
- Farand L, Renaud J, Chagnon F, Adolescent suicide in Quebec and prior utilization of medical services. Can J Public Health 2004;95(5):357–60.
- Cheung AH, Dewa CS. Mental Health Service Use Among Adolescents and Young Adults With Major Depressive Disorder and Suicidality. Can J Psychiatry. 2007;52(4):228–32.
- Alexandre P. Mental health care for youth: predictors of use are not always the same as predictors of volume. Soc Sci J 2008;45(4):619–32.
- Comacchio C, Lasalvia A, Bonetto C, et al the PICOS Veneto Group Clinical and social course of FEP patients over 5 years: the role of gender differences. (unpublished).