Giant cervical ependymoma, an infrequent presentation: Case report and review of the literature
Received: 05-May-2022, Manuscript No. PULNJ-22-489; Editor assigned: 05-May-2022, Pre QC No. PULNJ-22-4897(PQ); Accepted Date: May 27, 2022; Reviewed: 10-May-2022 QC No. PULNJ-22-4897; Revised: 19-May-2022, Manuscript No. PULNJ-22-4897 ; Published: 01-Jun-2022, DOI: 10.37532/pulnj.22.5(3).24-28
Citation: Vásquez M, Saavedra LJ, Aguilar WWL et al. Giant cervical ependymoma, an infrequent presentation: Case report and review of the literature. Neurosurg J. 2022; 5(3):24-28.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Ependymomas are tumors that develop from ependymal cells, and represent the most frequent primary spinal cord tumors in adults. The cervical spinal cord segment is the most frequently affected. Giant ependymomas (greater than 4 cm) are rare, although their real incidence is not known. The treatment of choice is surgical resection, total if possible, or subtotal associated with radiotherapy. We present two cases of giant cervical ependymomas, who consulted due to progressive limb weakness. Complete resection of the lesion was achieved in both cases, one of them received complementary radiotherapy. There was no evidence of recurrence after one and five years of follow up, respectively. Neurological improvement was achieved in both cases (modified Mc Kormick Scale I). Complete resection of Ependymomas Giant (EG) in our cases was safe and with good functional results.
Keywords
Giant ependymoma; Cervical spine; McKormick scale
Introduction
Since Ependymomas are tumours that arise from ependymal cells that line the ventricles and central canal of the spinal [1,2]. The World Health Organization (WHO) classifies ependymomas as grade I (myxopapillary and subependymoma), grade II (cellular, papillary, clear cell, and tanycytic), and grade III (anaplastic) [3-5]. Intradural spinal tumours represent up to 20% of primary Central Nervous System (CNS) tumours in adults and up to 35% in children and young adults. Ependymomas are the most common intramedullary tumours in adults, accounting for up to 60% of all primary neoplasms of the spinal cord and filum terminale.
The cervical segment is the most frequent location, with approximately two-thirds of the cases. Primary spinal ependymomas are usually solitary lesions. Giant ependymomas are conventionally defined as those measuring more than 4 cm. Surgical resection is the treatment of choice, total if possible, without generating more injury and subtotal associated with complementary radiotherapy. We present 2 cases of giant ependymoma, and the cases presented in the literature [6-9].
CASE SERIES
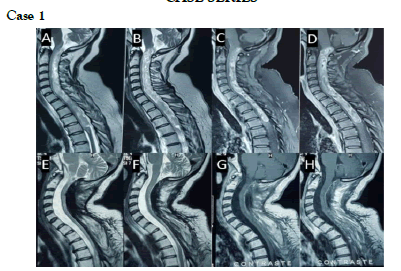
A 43-year-old woman, with no prior medical history, consulted with a 16-month illness, referring to pain, decreased strength and numbness in the lower limbs, as well as difficulty urinating in the last two months. On neurological examination she had quadriparesis with a femoral predominance (right upper limb 4/5, left upper limb 3/5, right lower limb 1/5, left lower limb 2/5); Left hemihypoesthesia, bilateral Babinski, muscular atrophy in the lower limbs and urinary retention. MRI of the cervical spine demonstrated a giant intradural extramedullary lesion with heterogeneous contrast enhancement, without cystic components, with a well-defined upper border at the level of C1 and lower borders at D4, without evidence of syringomyelia, which displaced and compressed the spinal cord toward the anterior border of the spinal canal (Figure 1).
Surgery
A laminectomy was performed from C1 to D4. After opening the dura mater, a semi-rigid violaceous tumour was observed that had well-defined and differentiated planes with the spinal cord throughout its course, which facilitated complete resection without complications during surgery. The postoperative course had no complications, with the improvement of strength in extremities on the fourth day. The pathology result confirmed the diagnosis of ependymoma (WHO grade II, (Figure 2). After surgery, she received 25 sessions of radiotherapy.
Results
Within five years of follow-up, the patient fully recovered her strength, and sphincter control, carried out her usual activities without any limitation (modified Mc Kormick Scale I), and the control MRI (Figure 1) showed no signs of recurrence (Table 1). She presents an asymptomatic increase in cervical lordosis and continues in periodic evaluation.
TABLE 1 Modified McCormick Scale for grading neurological function in spinal cord conditions.
| Functional grade | Explanation |
| I | Neurologically intact, ambulates normally, may have minimal dysesthesia |
| II | Mild motor or sensory deficit; patient maintains functional independence |
| III | Moderate deficit, limitation of function, independent w/ external aid |
| IV | Severe motor or sensory deficit, the limit of function w/ a dependent patient |
| V | Paraplegic or quadriplegic, even if there is flickering movement |
Case 2
A 21-year-old male presented with 7 months of evolution, referring to a progressive decrease in strength in the extremities, which began in the lower limbs, finally not being able to grasp objects and inability to walk due to the decrease in strength and the persistent "dizziness" that began two weeks before his hospitalization, in addition to decreased sensitivity in some regions of his body. He did not refer to sphincter alterations. On neurological examination, he presented quadriparesis 4/5, predominantly in the right upper limbs where he had strength 3/5, patellar and bicipital hyperreflexia, bilateral Babinski and C7 sensory level, ataxic gait, with normal sphincter control.
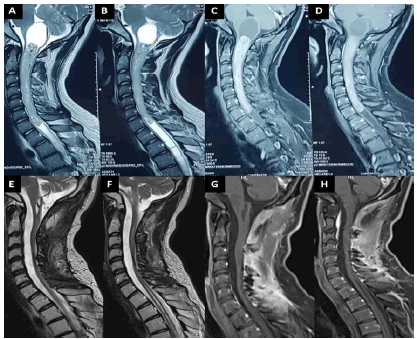
MRI of the spine showed an extensive cervical intramedullary tumour, without cystic component, with homogeneous contrast enhancement, the tumour had well-defined margins extending from C1 to C7. Satellite “syringomyelic cavities'' extending in the upper part towards the medulla and the lower part towards the dorsal medullary segment were evident in T2 sequences (Figure 3).
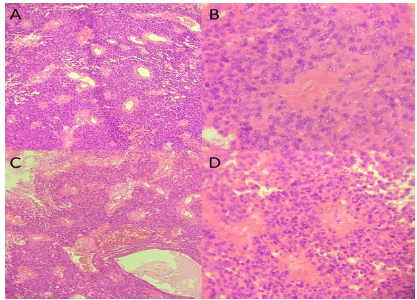
Figure 3: Tumours are composed of cells with regular, round to oval nuclei (Spindle-shaped cells with oval to elongated nuclei and delicate fibrillary cytoplasm with occasional intracytoplasmic lumina). There are perivascular pseudorosettes and microvascular proliferation; A,B) patient 1; C,D) patient 2; (A and C shows Hematoxylin-Eosin stain at 10x, B and D shows Hematoxylin-Eosin stain at 40x)
Surgery
A C1-C7 laminectomy was performed, with C2-C4 laminoplasty. The syringomyelic cavities favoured the identification of the superior and inferior borders and clearly defined the plane between the tumour and the spinal cord. After myelotomy, a firm tumour was identified, violaceous in colour with well-defined margins compared to normal spinal tissue. Surgery was performed with neurophysiological monitoring (sensory evoked potentials) without changes during surgery. Total resection was finally achieved without complications. The pathological anatomy results confirmed the diagnosis of ependymoma (WHO grade II).
Results
The impaired strength in both lower extremities recovered within 3 days, and the rest of the neurological examination was normal. Along a 12-month follow-up period, the patient presents right distal brachial monoparesis 4+/5, with no other neurological deficit (modified Mc Kormick Scale I) (Table 1). Control MRI (Figure 2) showed no signs of tumour recurrence, with minimal residual dorsal syringomyelia compared to the preoperative images.
Discussion
A literature search in PubMed, using the words "giant", "Ependymoma", "cervical", "large", and "Spine" identified only 8 case reports (Table 1). The clinical presentation of spinal ependymomas is highly variable. They can present with benign mechanical pain as well as inflammatory disease or spinal metastases reported in up to 60%-70% of cases [10]. Some authors reported that 10% of patients had radicular pain or dysesthesias and around 50% had long tract deficits. Touch and pain sensations are usually affected first, due to the central topography of these tumours. Except in cone or cauda equina tumours, sphincter dysfunction is not common. Acute neurological deterioration is rare but can occur after tumour bleeding, especially those of the papillary histological type due to their greater vascularization. A particular case presented with abnormal sweating on the left side of the neck, upper extremity and chest that improved after surgery. Spinal cord injuries are complex to treat due to the potential for neurological sequelae, even more so if they are giant tumours. The development of microsurgical techniques and medical technology have made it possible to obtain better functional results [11-12].
The diagnosis is confirmed with magnetic resonance imaging (MRI) with contrast media, which is currently more widely available. The cervical segment is the most frequently affected region, in approximately 75% of cases. Syringomyelia is an associated lesion, which was reported in 3 of the 8 cases mentioned, two of the proximal and distal, and one of the distal only. One of our patients developed syringomyelia proximal to the bulbomedullary junction and distal to the dorsal medullary segment. In all reported cases, including ours, syringomyelia resolved after surgery. In 3 of the cases in the literature, the lesions had a dorsal component, as in one of our cases.
The treatment of choice for cervical ependymomas is total resection, ideally with intraoperative neurophysiological monitoring, usually Somatosensory Evoked Potentials (SSEP). Ependymomas can be approached in different ways, in 4 of the reported cases, cervical laminectomy was performed to resect the lesion, and hemilaminectomy, hemilaminoplasty, and cervical laminoplasty were used in one case respectively. In one of our cases a wide C1 cervical laminectomy was performed - D4, and in the other, laminectomy C1 - C7 with laminoplasty from C2 to C4. In four of the cases in the literature, neurophysiological monitoring (PESS) was used, without alterations during surgery, as in one of our cases (logistical problems on the day of surgery precluded its use in the other case). In patients undergoing cervical laminectomy of 3 or more levels, with motor symptoms, bone fragility and in children, concomitant instrumentation and fusion must be considered [13].
Undoubtedly, total resection is the final objective, and it was obtained in 7 of the 8 reported cases and in both of our cases Only 90% resection was achieved in the remaining case because they did not find a clear plane between the tumour and the bone marrow. Ependymomas have a well-differentiated plane with respect to normal nervous tissue, which facilitates their total resection. The most frequently reported complication is a cerebrospinal fluid fistula, with two cases reported, one of them associated with meningitis and the other with surgical wound infection [14]. The typical presentation (in all the reported cases, including ours) involves the transitory deterioration of strength, in different degrees and extensions, in one of our cases he presents as transitory paraparesis. Only one of the aforementioned patients remained with quadriparesis and pain in the lower limbs. This reaffirms that complete resection of the lesion should always be our goal. It has been (Table 2) that the preoperative result correlated significantly with the postoperative result (p<0.001) [15,16]. All the postoperative deficits of the mentioned patients reverted during follow-up.
TABLE 2 Summary of cases of giant cervical ependymomas reported in the literature.
Author/Year |
n |
Age |
Sex |
IT |
Clinical presentation |
Location |
Surgery |
PES |
Degree resection |
Complications |
Follow up/Months |
MMS |
Recurrence |
RT |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Fourney, D-2004 |
1 |
22 |
M |
2 y |
Quadriparesis, |
C1 - C7 |
Laminectomy |
yes |
total |
CSF fistula, |
9 |
I |
No |
No |
hyperreflexia in ll, |
SRM |
C1-C7 |
meningitis |
|||||||||||
bilateral Babinski |
Upper - lower |
|||||||||||||
Barbagallo, G-2009 |
1 |
25 |
F |
7 m |
Quadriparesis, ataxic gait, |
C2 - C5 |
Laminotomy |
No |
total |
No |
18 |
I |
No |
No |
C4 sensory level, |
SRM lower T2 |
C2 -C5 |
||||||||||||
bilateral Babinski |
||||||||||||||
Trivedi, P-2011 |
1 |
47 |
M |
3 y |
Left hemiparesis |
C1 - C5 |
Laminectomy |
No |
total |
No |
16 |
I |
No |
No |
C1-C5 |
||||||||||||||
Arrifin, A-2012 |
1 |
30 |
F |
1 y |
Muscle atrophy ul, |
C2 - T3 |
Laminoplasty |
yes |
total |
CSF fistula, |
3 |
II |
No |
No |
areflexia, |
SRM |
C2 - T3 |
surgical site infection |
|||||||||||
paraparesis 2/5 |
Upper - lower |
|||||||||||||
Cikla, U-2014 |
1 |
29 |
M |
nd |
Left monoparesis, faecal and bladder incontinence, right Hoffman, C5 sensory level |
C3 - C6 |
Laminectomy |
yes |
total |
No |
nd |
I |
No |
nd |
C2 -C7 |
||||||||||||||
Haddadi, K-2016 |
1 |
35 |
M |
4 y |
Right C5-T6 dermatome hiperhidrosis, |
C1 - T2 |
Laminectomy |
yes |
subtotal |
No |
12 |
I |
No |
yes |
left monoparesis ul |
C1 - T1 |
0.9 |
||||||||||||
hypoesthesia left ll |
||||||||||||||
Hernando, R-2016 |
1 |
42 |
M |
7 y |
Quadriparesis, |
C2 -T5 |
Hemi- |
No |
total |
No |
56 |
III |
No |
yes |
patellar hyperreflexia, |
laminectomy |
|||||||||||||
right Babinski |
C3 -T6 |
|||||||||||||
Oral, S-2018 |
1 |
47 |
F |
10 y |
Hypoaesthesia left dermatomes C4-C7, |
C3 -C7 |
Hemi- |
No |
total |
No |
nd |
I |
No |
nd |
patellar hyperreflexia |
laminoplasty |
|||||||||||||
bilateral Hoffman's reflex |
C3 -C7 |
|||||||||||||
IT: illness time, PES: potentiels évoqués somesthésiques, MMS: modified McCormick score, RT: Radioterapy, SRM: Siryngomyelia, ll: lower limb, ul: upper limb, nd: no data |
||||||||||||||
In none of the cases mentioned were recurrences reported in the respective follow-up time, which was an average of 19 months with a range (3m-56m). In our cases, they were controlled at 12 months and 5 years, with no evidence of recurrence. Two of the reported cases and one of ours were referred for complementary radiotherapy. Our experience supports the option of total macroscopic resection of the tumour [17-19].
Conclusion
In our cases, total resection of giant cervical ependymomas was possible without neurological sequelae or tumour recurrence. We did not observe problems secondary to wide laminectomies.
REFERENCES
- Marchesini N, Soda C, Ricci UM, et al. Giant intradural extramedullary spinal ependymoma, a rare arachnoiditis-mimicking condition: case report and literature review. Br J Neurosurg. 2019:1-6.
Google Scholar CrossRef - Arrifin A, Kaliaperumal C, Keohane C, et al. ‘Serpent in the spine’: a case of giant spinal ependymoma of cervicothoracic spine. Case Rep. 2012.
Google Scholar CrossRef - Fourney DR, Siadati A, Bruner JM, et al. Giant cell ependymoma of the spinal cord: case report and review of the literature. J Neurosurg: Spine. 2004;100(1):75-9.
Google Scholar CrossRef - Ottenhausen M, Ntoulias G, Bodhinayake I, et al. Intradural spinal tumours in adults—update on management and outcome. Neurosurg Rev. 2019;42(2):371-88.
Google Scholar CrossRef - Samartzis D, Gillis CC, Shih P, et al. Intramedullary spinal cord tumours: part I—epidemiology, pathophysiology, and diagnosis. Glob Spine J. 2015;5(5):425-35.
Google Scholar CrossRef - McCormick PC, Torres R, Post KD, et al. Intramedullary ependymoma of the spinal cord. J Neurosurg. 1990;72(4):523-32.
Google Scholar CrossRef - Cooper PR. Outcome after operative treatment of intramedullary spinal cord tumours in adults: intermediate and long-term results in 51 patients. Neurosurgery. 1989;25(6):855-9.
Google Scholar CrossRef - Hanbali F, Fourney DR, Marmor E, et al. Spinal cord ependymoma: radical surgical resection and outcome. Neurosurgery. 2002;51(5):1162-74.
Google Scholar CrossRef - Shamji MF, Benoit BG, Perry A, Jansen GH. Giant cell ependymoma of the thoracic spine: pathology case report. Neurosurgery. 2009;64(3):E566-E567.
Google Scholar CrossRef - Joaquim AF. Abordagem inicial do paciente com mielopatia aguda não compressiva. RBM Rev Bras Med. 2007:164-9.
Google Scholar CrossRef - Epstein FJ, Farmer JP, Freed D. Adult intramedullary spinal cord ependymomas: the result of surgery in 38 patients. J Neurosurg. 1993;79(2):204-9.
Google Scholar CrossRef - Haddadi K. A huge ependymoma of the cervical spinal cord with subtle atypical manifestations and hyperhidrosis: Case report. Int J Surg Case Rep. 2016;19:100-2.
Google Scholar CrossRef - Sgouros S, Malluci CL, Jackowski A. Spinal ependymomas-the value of postoperative radiotherapy for residual disease control. Br J Neurosurg. 1996;10(6):559-67.
Google Scholar CrossRef - Kucia EJ, Bambakidis NC, Chang SW, et al. Surgical technique and outcomes in the treatment of spinal cord ependymomas, part 1: intramedullary ependymomas. Oper Neurosurg. 2011;68:57-63.
Google Scholar CrossRef - Hoshimaru M, Koyama T, Hashimoto N, et al. Results of microsurgical treatment for intramedullary spinal, cord ependymomas: analysis of 36 cases. Neurosurgery. 1999;44(2):264-9.
Google Scholar CrossRef - Cooper PR. Outcome after operative treatment of intramedullary spinal cord tumours in adults: intermediate and long-term results in 51 patients. Neurosurgery. 1989;25(6):855-9.
Google Scholar CrossRef - Chamberlain MC, Tredway TL. Adult primary intradural spinal cord tumours: a review. Curr Neurol Neurosci Rep. 2011;11(3):320-8.
Google Scholar CrossRef - Boström A, von Lehe M, Hartmann W, et al. Surgery for spinal cord ependymomas: outcome and prognostic factors. Neurosurgery. 2011;68(2):302-9.
Google Scholar CrossRef - Rafael H. Functional tolerance of the cervical cord in giant ependymoma. J Brain Tumors Neurooncol. 2016;1(109):2.
Google Scholar CrossRef