Is Mexican policy " Peritoneal dialysis first for all " the best strategy for elderly end stage renal disease patients?
2 Department of Nephrology, University of Guadalajara, CUCS, Mexico
3 Department of Nephrology, PiSA Farmacéutica, Sanefro, Mexico
Received: 10-Jul-2024, Manuscript No. PULCNR-22-4118; Editor assigned: 12-Jul-2024, Pre QC No. PULCNR-22-4118(PQ); Accepted Date: Jul 20, 2024; Reviewed: 16-Jul-2024 QC No. PULCNR-22-4118(Q); Revised: 17-Jul-2024, Manuscript No. PULCNR-22-4118(R); Published: 30-Jul-2024, DOI: 10.37532/pulcnr.22.6(1).10-12
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
BACKGROUND: The Mexican population is ageing. The average age for patients on dialysis in Mexico is 63 years (range 1-90), with the higher prevalence in the group from 60 to 69 (24.5%). Mexico has had the policy of “peritoneal dialysis first for all” for all incident ESRD patients, but Peritoneal Dialysis (PD) prescription has decreased 1% per year in a sustained manner for the last 10 years. A sub-analysis on mortality in prevalent HD patients >60 years old has not been reported.
OBJECTIVE: To evaluate survival in HD elderly patients and determine risk factors for mortality.
METHODS: We prospectively analyzed hemodialysis prevalent patient’s ≥ 60 y/o. All patients were receiving 3 hemodialysis treatments per week. Database Excel and SPSS for statistics were used. We describe mortality, survival, vascular access, kt/v, hemoglobin, and socio-demographic data (T student, Kaplan Meier when appropriate).
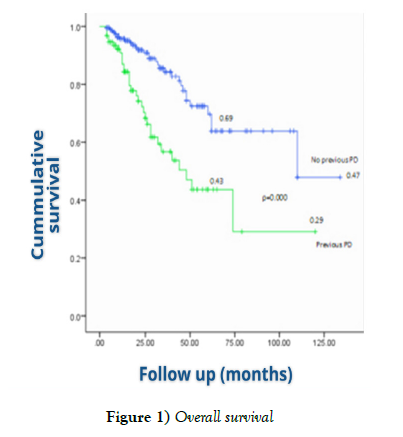
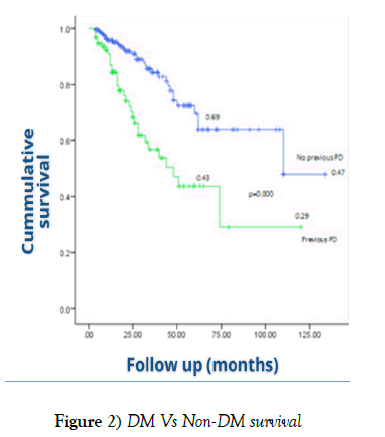
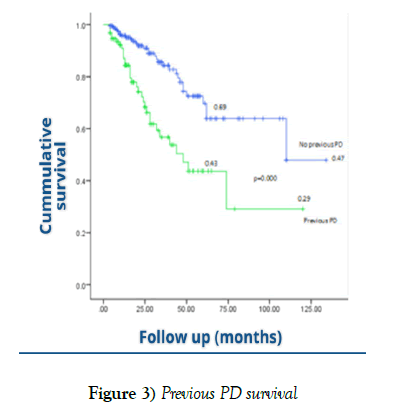
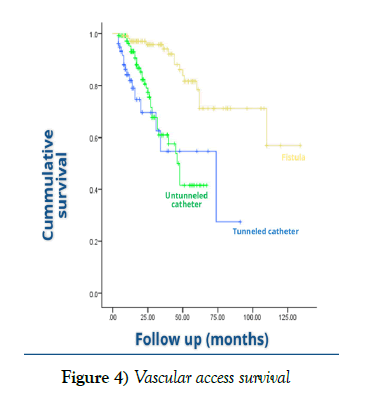
RESULTS: We reviewed the records of 1418 patients. Thirty-two-point six % were ≥ 60 years old, 64% had diabetes. Hemoglobin and kt/v values were like those reached in younger patients. One out of every three patients had previous peritoneal dialysis. The main cause of exit from the peritoneal dialysis program was peritonitis (52%). For patients >60y/o, overall cumulative survival at 12, 24, 36, 48 and 60 months was 0.93, 0.84, 0.75, 0.65, 0.61 respectively. Worst outcomes were identified for patients with any kind of catheter (p=0.000), diabetes (p=0.036) and), previous PD (p=0.000). Once renal replacement therapy is initiated, the range of the expected remaining life span in the USRDS report is approx. 54 months for those patients 60 to 64 years of age, compared with 26.3 months in our patients (range 4-110).
CONCLUSION: One out of three prevalent hemodialysis patients in Mexico are ≥ 60 years of age. Hemoglobin and kt/v values were like those reached in younger patients. Worst survival was observed for those with any catheter and diabetes mellitus.
Lower survival was found in patients with previous peritoneal dialysis. The Mexican policy of “peritoneal dialysis first for all” should be reconsidered in diabetic ESRD patients aged >60.
Keywords
Elderly; Hemodialysis; Peritoneal dialysis; Mortality
Introduction
The Mexican population is ageing, and it is estimated that the number of persons older than >60 years will duplicate by the year 2050. In year 2000, there was 21.3 older adults (>60 years of age) for every 100 children and youth; in 2015, this proportion increased to 38 [1]. The average hemodialysis patient’s age in the US is 62 years old [2]. Mendez-Duran et al reported in 2018 that the average age for patients on dialysis in Mexico was 63 years (range 1-90), with the higher prevalence in the group from 60 to 69 (24.5%) [3]. As the population ages, the burden of chronic non-communicable diseases increases. End Stage Renal Disease (ESRD) is recognized worldwide as a major health issue. Its incidence and prevalence in Mexico are constantly rising. Diabetes mellitus and hypertension are reported as the main cause of Chronic Kidney Disease (CKD) among Mexicans. Thus, more and more patients initiated on dialysis are either diabetic and/or hypertensive [3].
Due to budget constraints for health, Mexico has had the policy of “peritoneal dialysis first for all” for all incident ESRD patients. Nevertheless, Peritoneal Dialysis (PD) prescription has decreased 1% per year in a sustained manner for the last 10 years. Back in year 2010, only 33% of patients were on Hemodialysis (HD). This has changed gradually. Nowadays, there are 44% of patients on HD and the remain 57% on PD [3]. We do not have data to elucidate if this switch is due to more patients that are initiated on hemodialysis, or if this proportion has changed because of the number of patients that failed on PD and migrated to HD.
Anyway, more and more ageing patients are on HD. Anemic syndrome (45%), vascular access infection (34%), uncontrolled hypertension (28%), fluid overload (12%), heart failure (9%) and severe hyperphosphatemia (7%) are reported as mayor causes of morbidity in hemodialysis in Mexico [3]. A sub-analysis on mortality in patients >60 years old has not been reported.
Our objective was to evaluate survival in HD elderly patients and determine risk factors for mortality.
Method
We prospectively analyzed hemodialysis prevalent patient’s ≥ 60 y/o, in 7 nonhospital basis hemodialysis facilities. All patients were receiving 3 hemodialysis treatments per week. The observational period was from Jan 2014 through Feb 2018. We included all prevalent patients in this period. We used a database from Excel and SPSS for statistics. We describe mortality, survival, vascular access, kt/v, hemoglobin, and socio-demographic data (T student, Kaplan Meier when appropriate).
Results
We reviewed the records of 1418 patients. Thirty-two-point six % were ≥ 60 years old, 63% were male (male: female proportion 1.7:1) and had diabetes (64%). Hemoglobin and kt/v values were like those reached in younger patients. One out of every three patients had previous peritoneal dialysis. The main cause of exit from the peritoneal dialysis program was peritonitis (52%) (Table 1). For patients >60 y/o, overall cumulative survival at 12, 24, 36, 48 and 60 months was 0.93, 0.84, 0.75, 0.65, 0.61 respectively. Worst outcomes were identified for patients with any kind of catheter (p=0.000), diabetes (p=0.036) and), previous PD (p=0.000) (Figures 1-4) Once renal replacement therapy is initiated, the range of the expected remaining life span in the USRDS report is approx. 54 months for those patients 60 to 64 years of age, compared with 26.3 months in our patients (range 4-110).
| Characteristics | All patients n=1418 | ≥ 60 y/a n=463 | p |
|---|---|---|---|
| Age | 46.7 5 ± 19.6 | 70.27 ± 6.82 | -- |
| Male, n (%) | 907 (64) | 291 (63) | NS |
| M, n (%) | 483 (34) | 296 (64) | 0.000001 |
| Previous PD, n (%) | 44 | 148 (32) | 0.000002 |
| Average Hb, gr/dl | 9.9 | 10.4 | NS |
| % Patients with Hb 10-12 gr/dl | 37 | 42 | 0.14 |
| Average kt/v | 1.16 | 1.16 | NS |
| % Patients with ktv ≥ 1.2 | 47 | 44 | 0.12 |
| Untunneled catheter, n (%) | 454 (32) | 111(24) | 0.0005 |
| Tunneled catheter, n (%) | 510 (36) | 186 (40) | 0.06 |
| Native AV fistula, n (%) | 454 (32) | 166 (36) | 0.06 |
TABLE 1 Clinical and sociodemographic characteristics
Discussion
Patients aged 60 and older face different challenges than younger patients. Unsurprisingly, mortality is considerably higher for elderly patients on dialysis than for elderly patients who are not. It is important to note that survival is influenced strongly by comorbidities such as diabetes, vascular and cardiac disease [4]. Once these are considered, the age of elderly patients is not an independent risk factor for increased mortality [5,6].
According to USRDS data from 2019, nearly one half of incident dialysis patients in the US are senior citizens, with the median age at dialysis initiation of 64.4 years. The most prevalent age group on dialysis in Mexico is 60 to 69 years. The mean survival in our HD patients >60 y/o is significantly lower than that reported in USRD, and yet, we do not have sub-analyses on mortality or morbidity in this population [2,3].
As expected, we found that diabetes mellitus is a risk factor for decreased survival on hemodialysis in patients >60 y/o. Unfortunately, 6 out of 10 patients >60 y/o in Mexico on Renal Replacement Therapy (RRT) have diabetes. Diabetic nephropathy is and will continue to be the main cause of ESRD in Mexico, and, with the aging of our population more and more patients on dialysis therapy will have diabetes mellitus as a risk factor for lower survival.
On the other hand, as in younger patients, the observation remains that catheters are associated with higher mortality than other types of vascular access [7]. It is well known that the arterio-venous fistula (AVF) is the ideal vascular access for HD. When comparing with the US prevalent HD patients aged 65+, we observed a higher catheter use in our population (20% vs 64% respectively) [2]. We must focus our efforts on modifying the risk factors that reduce survival in HD patients >60 years of age, such as avoiding the use of catheters as definitive vascular access.
We identified that patients with a history of peritoneal dialysis had significantly lower survival on HD than those who had not been on a PD program. In this analysis, we found that one in 3 hemodialysis patients aged 60+ had a history of peritoneal dialysis, and that one in two failed therapies due to peritonitis. In the US, less than 7% of patients >65 y/o use PD [2]. Several studies reported that long-term survival seemed to be the same in HD and PD in patients >60 y/o, but other authors have reported that, when adding diabetes, patients do better on HD than on PD [8]. Vonesh, et al. reviewed a US database and found that death rates for nondiabetic patients over 65 y/o without other comorbidities were slightly lower on PD than on HD, whereas the reverse was true for diabetics with or without comorbidities in the same age group [9].
Worldwide, PD is an underused modality, but in Mexico, PD is the RRT of choice for nearly all incident patients, regardless their age, comorbidities, family support and overall sociodemographic conditions. Until a few years ago, in Mexico, only those patients who had failed peritoneal dialysis were admitted to the HD program or those with absolute contraindications for PD.
Mexican policy of “peritoneal dialysis first for all” responds to a need to optimize the budget allocated to medical care for a disease as expensive as ESRD, and not to medical needs. We strongly suggest that it is important to reconsider whether ESRD diabetic patients >60 years of age are good candidates for “peritoneal dialysis modality first”.
Conclusion
One out of three prevalent hemodialysis patients in Mexico is ≥ 60 years of age. Hemoglobin and kt/v values were like those reached in younger patients.
As expected, the worst survival was observed for those with any catheter and diabetes mellitus. The rate of catheter use in our population over 60 years of age is significantly higher than that reported in other countries. It is important to focus efforts on improving the transition from the catheter to fistula.
Lower survival was found in patients with previous peritoneal dialysis.
Optimal management of diabetic ESRD in elderly patients may involve heightened risks and must consider their increased mortality rates, thus, the Mexican policy of “peritoneal dialysis first for all” should be reconsidered in diabetic ESRD patients aged >60.
REFERENCES
- Databases of Population Projections of Mexico and the Federal Entities, 2016-2050. National Population Council. 2018.
- US Renal Data System 2019 Annual Data Report: Epidemiology of kidney disease in the United States. Am J Kidney Dis. 2019:S0272-6386(19).
- Méndez-Durán A, Ignorosa-Luna MH, Pérez-Aguilar G, et al. Current status of alternative therapies renal function at the Instituto Mexicano del Seguro Social. Rev Méd Inst Mex Seguro Soc. 2016;54(5):588-593.
- Méndez-Durán A. Evolution of renal replacement therapy in Mexico in the last 10 years. Nefrol (Engl Ed). 2021;41(1):82-83.
- Williams Mark E., Robert C. Stanton. Kidney disease in elderly diabetic patients. American Society of Nephrology, editor. Geriatr Nephrol Curric, Wash: ASN. 2009.
- Couchoud C, Labeeuw M, Moranne O, et al. A clinical score to predict 6-month prognosis in elderly patients starting dialysis for end-stage renal disease. Nephrol Dial Transplant. 2009;24(5):1553-15561.
- O'Hare AM, Bertenthal D, Walter LC, et al. When to refer patients with chronic kidney disease for vascular access surgery: should age be a consideration? Kidney Int 2007;71(6):555-561.
- Winkelmayer WC, Glynn RJ, Mittleman MA, et al. Comparing mortality of elderly patients on hemodialysis versus peritoneal dialysis: a propensity score approach. J Am Soc Nephrol. 2002;13(9):2353-2362.
- Vonesh EF, Snyder JO, Foley RN, et al. The differential impact of risk factors on mortality in hemodialysis and peritoneal dialysis. Kidney Int. 2004;66(6):2389-2401.