Momentary visual hypotensive impact of liquor
Received: 10-Jan-2022, Manuscript No. PULOCTJ-22-4255; Editor assigned: 12-Jan-2022, Pre QC No. PULOCTJ-22-4255(PQ); Accepted Date: Jan 12, 2022; Reviewed: 18-Jan-2022 QC No. PULOCTJ-22-4255; Revised: 21-Jan-2022, Manuscript No. PULOCTJ-22-4255(R); Published: 11-Feb-2022, DOI: DOI:10.37532/puloctj.22.6.1.1
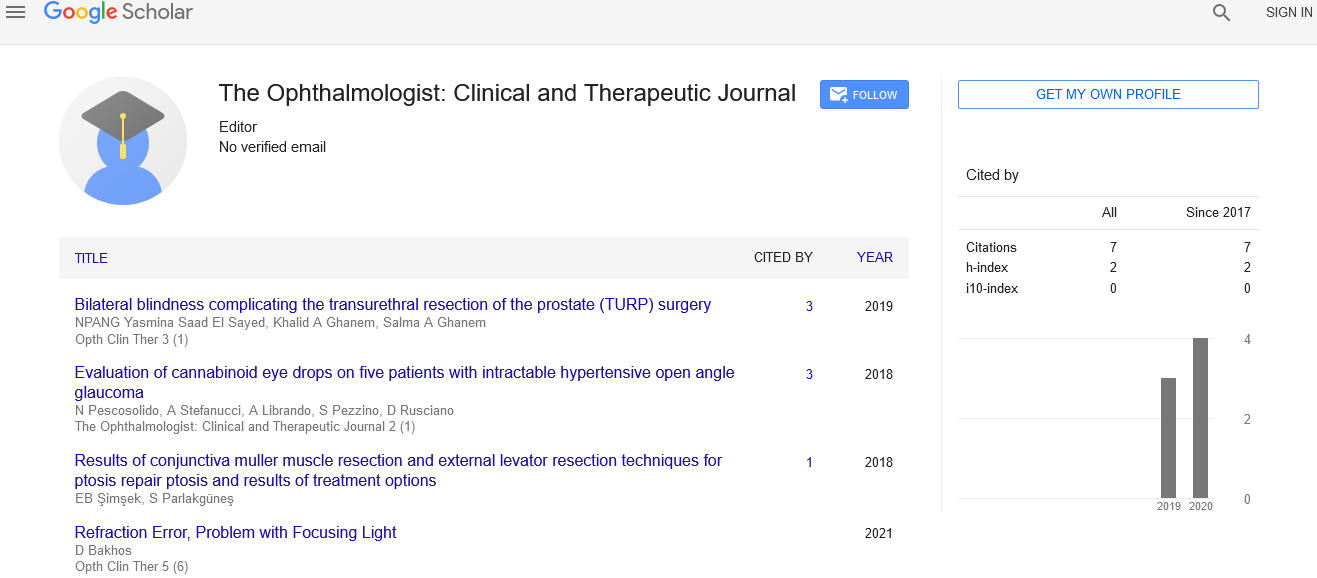
Citation: Mertens O. Momentary visual hypotensive impact of liquor. Opth Clin Ther. 2022;6(1):1.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
This orderly audit and meta-investigation sums up the current proof for the relationship of liquor use with Intraocular Pressure (IOP) and Open-Point Glaucoma (OAG). Understanding and evaluating these affiliations might help clinical rules or treatment methodologies and shed light on illness pathogenesis. The job of liquor, a modifiable variable, in deciding IOP and OAG hazard may likewise be of interest from an individual or general wellbeing point of view. Glaucoma contains a heterogeneous gathering of illnesses described by moderate optic neuropathy and visual field misfortune and is the main source of irreversible visual deficiency worldwide. Global predominance is assessed at 76 million and is projected to increment to 112 million by 2040. The exact Pathogenesis of Essential Open-Point Glaucoma (POAG), the most well-known type of the sickness, isn’t completely seen however the last infection pathway is set apart by retinal ganglion cell apoptosis and optic nerve fiber loss. Prevailing speculations embroil Intraocular Pressure (IOP)- intervened mechanical pressure, as well as different visual vascular danger factors, as go between of this process. It is possible that proximal determinants of POAG address a complicated interaction of hereditary, ecological, physical and physiological factors.
Key Words
Intraocular pressure, open point glaucoma, pathogenesis, optic nerve head
Introduction
Liquor use is involved in a huge number of persistent illnesses across different organ frameworks and is the seventh driving reason for death and handicap worldwide. The intense impacts of liquor on the natural eye incorporate a transient, apparently portion subordinate decrease in IOP and expansion in blood stream to the Optic Nerve Head (ONH), hypothetically giving a defensive advantage against the improvement of glaucoma. Ongoing liquor use, in any case, is related with a large group of neurodegenerative, cardiovascular and endocrine problems, as well as foundational biochemical and physiological confusions, and the long haul or circuitous jobs these may play in glaucoma are unclear. As opposed to the momentary visual hypotensive impacts of liquor, various epidemiological examinations have revealed crosssectional relationship between liquor use and higher IOP or Predominance of Visual Hypertension (OHT), yet this isn’t generally a predictable finding. There is likewise proof to recommend that any relationship with IOP might be interceded by both sex and glaucoma status. Additionally, most observational investigations investigating the relationship between liquor use and glaucoma have yielded non-huge outcomes, with both cross-sectional and longitudinal studies neglecting to show a steady affiliation. A superior comprehension of these affiliations might offer understanding into likely instruments of glaucomatous optic neuropathy, direct future examination and illuminate clinical exhortation or rules. It might likewise hold any importance with people wishing to figure out how modifiable way of life factors, like liquor utilization, may impact IOP or the danger for glaucoma.
Result
34 examinations were remembered for the efficient survey. Proof from 10 examinations revealing a relationship with IOP recommend that routine liquor use is related with higher IOP and predominance of visual hypertension (IOP>21mmHg), albeit outright impact sizes were little. 11 of 26 investigations, containing 173 058 members, that tried for a relationship with OAG met incorporation standards for meta-examination. Pooled impact gauges showed a positive relationship between any utilization of liquor and OAG (1.18; 95% CI, 1.02-1.36; p=0.03; I2=40.5%), with comparable assessments for both common and episode OAG. The general GRADE sureness of proof was extremely low. Liquor use was decidedly connected with IOP in 2 studies, albeit the outright contrast among consumers and non-consumers (0.1 mmHg in the two examinations) was little. A further 2 investigations tracked down certain direct relationship between liquor admission and IOP in men, however not ladies, without glaucoma (IOP distinction of 0.7-1.4 mmHg between most noteworthy admission bunch and no admission group). In one of these examinations, utilization of liquor >4 times/week in ladies with glaucoma was related with higher IOP (+2.8 mmHg) contrasted with non-consumers, yet without any proof of straight trend. Alcohol admission was not related with IOP in study and adversely related (IOP distinction <0.1 mmHg) in past, yet not current, consumers in another. While this meta-investigation proposes a destructive relationship between liquor use and OAG, our outcomes should be deciphered mindfully given the shortcoming and heterogeneity of the fundamental proof base, the little outright impact size and the fringe measurable importance. Regardless, these discoveries might be clinically significant and future exploration should zero in on working on the nature of proof.