Multiple stage tissue expansion for reconstruction of scalp nevocellular nevus in pediatric age group: A case report
Citation: Al-Bassam A, Al-Burshaid H, Al-Jehani R, et al. Management of Multiple stage tissue expansion for reconstruction of scalp nevocellular nevus in pediatric age group: A case report. Surg Case Rep. 2018;2(2):32-4.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
OBJECTIVE: To present a rare case of giant congenital nevocellular nevus ina 7-year-old girl scalp and to highlight our management steps and outcomes.
CASE REPRESENTATION: An otherwise healthy 7-year-old girl presentedto plastic surgery clinic with agiant congenital nevus (GCN) that coveredalmost her entire scalp that was treated successfully with tissue expanderthree times over a period of 14 months. A total of 38 cm width of skin,which comprised 78% of the patient scalp, was removed. The patient wasreassessed five years later with a great cosmetic outcome represented by a remarkable hair growth and near normal scalp appearance.
CONCLUSION: We concluded that giant scalp nevocellular nevi in pediatric age group could be treated completely with tissue expanders more than twice to achieve near normal outcomes.
Keywords
Plastic surgery; Nevocellular nevus; Giant nevus; Tissue expander; Nevi; Pediatrics; Cosmetic
Introduction
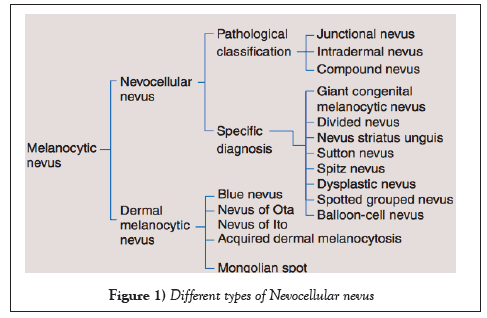
Nevocellular nevi are benign melanocytic tumors that originate in the skin. They are usually congenital and a result of proliferation of melanocyte in the skin. One type of congenital nevi is giant congenital nevus (GCN) (Figure 1), which covers a large area of the body due to over pigmentation and causes a great cosmetic concern to the patient (1,2). In general, congenital nevi affect 1% of newborns in terms of small size nevi. However this is not the case with GCN, the incidence of it is far less than the incidence of large congenital nevi, which occur to 1 in 200,000 babies (3). Not only it causes a cosmetic concern, but also it places the patient at a risk of 5-7% to develop melanoma. In addition to the cosmetic issues that it already causes, negative psychological effect to the parents is another distressing issue (2). Therefore, necessitates early excision and reconstruction by plastic surgeons.
For such cases, surgical treatment is performed to remove the lesion. It can range from resection, graft and usage of tissue expanders (TE) (4).
In this report we’d like to present a case of a 7-year-old patient with a GCN occupying her scalp; in which, three tissue expanders were used.
Clinical Presentation
A 7-year-old girl with no significant past medical, surgical or family history was referred to our plastic surgery clinic as a case of a pigmented nevus that involved most of the scalp since birth. The nevus was associated with pruritus and serous discharge. Local examination revealed a pigmented, thick and corrugated lesion that involved almost her entire scalp leaving a strip of normal skin with a width of 10 cm. (Figure 2).
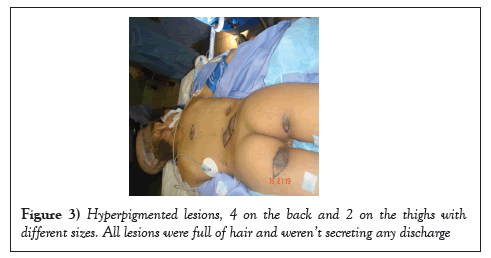
On full body examination, she was found to have scattered, hyper-pigmented lesions fully covered with hair on lower back and upper thighs with estimated sizes ranging from 2 × 2 to 6 × 6 cm (Figure 3). The case was discussed with the family as the need for multi-staged tissue expansion and serial skin excisions.
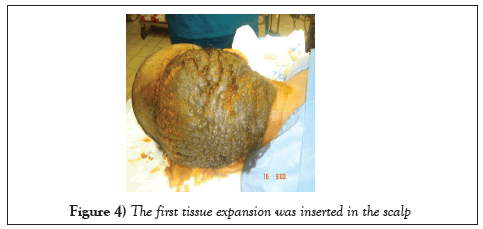
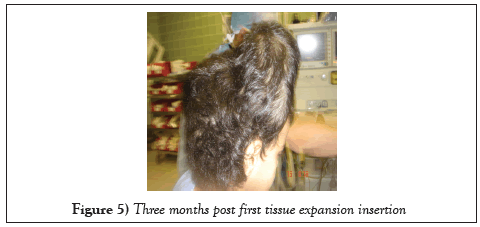
The first stage was done by inserting a crescent-shaped TE with a capacity of 500 mL underneath the normal skin above the hairline. Two weeks later, a 40- 50 mL of normal saline was injected through the expander valve. Injection was done twice a week as the optimal skin expansion was noted after injecting the expander beyond its capacity and up to 700 mL (Figures 4 and 5).
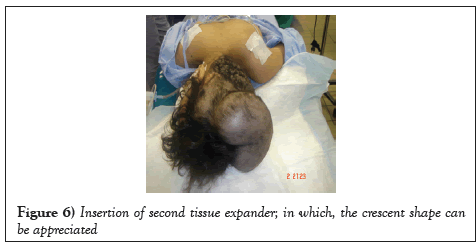
The second procedure took place three months after the first one; in which, T.E. was removed. A 12 cm width of the nevus was excised and the newly expanded skin covered the excised part of the scalp thoroughly. Two months post TE removal; a second expander was implanted and inflated into the scalp (Figure 6).
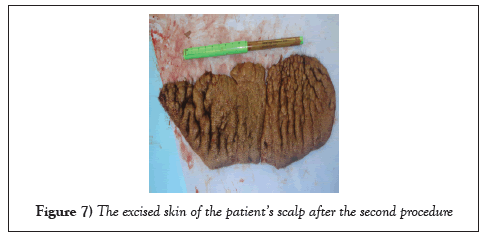
The patient returned to the OR three months after, for the removal of the second T.E., and a 10 cm width of the lesion was excised; the area was covered with the new expanded skin (Figure 7).
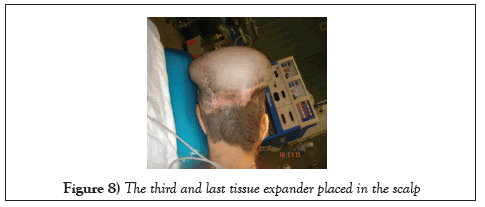
The fifth procedure was perfromed to the patient; in that, a third T.E was inserted into the scalp (Figure 8). Finally, removing the last tissue expander was done through the final procedure, and the expanded skin was stretched down to the nape. The last remaining part of the nevus with a width of 12 cm was completely excised and the raw area of scalp was covered with the expanded skin.
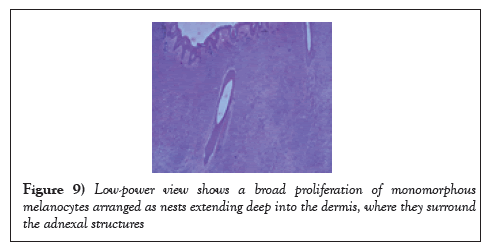
All the specimens collected were sent to the histopathology lab and the report revealed that the specimens had nests and diffusely cellular sheets of benign melanocyte with superficial focal pigmentation and deep dermal maturation. Lateral margins and deeper margins were involved. Overall, there was no malignancy reported (Figures 9-11) (Table 1)
| Phases | Procedure | Time | |
|---|---|---|---|
| Stage 1 | Phase 1 (procedure 1) | Insertion the 1st TE | - |
| Phase 2 (procedure 2) | 1st TE was removed and a 12 cm width of skin was excised | 3 month after the first phase | |
| Stage 2 | Phase 1 (procedure 3) | Insertion of 2nd TE | 2 months after phase 2 of stage 1 i.e., 5 months after procedure (1) |
| Phase 2 (procedure 4) | Removal of 2nd TE and excision of a 10 cm width of skin | 3 months after phase 1 of stage 2 i.e., 8 months after procedure (1) | |
| Stage 3 | Phase 1 (procedure 5) | Insertion of 3rd TE | 3 months after phase 2 of stage 2 i.e., 11 months after procedure (1) |
| Phase 2 (procedure 6) | Removal of 3rd TE and excision of a skin with a width of 12 cm | 3 months after phase 1 of stage 3 i.e., 14 months after procedure (1) |
Table 1: A time table that summarizes the main 3 stages of the surgery and each phase with a brief description of the procedures done along with their time with reference to the previous procedure
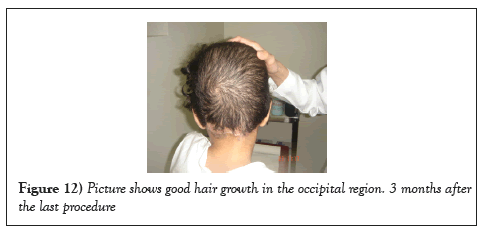
Five years later and at the age of 13, she was seen with her parents in the clinic doing fine with a normally growing long hair and no complications (Figures 12 and 13).
Discussion
In the late 1950s, Neumann used TE for covering subauricular defects. However, TE did not get popularized until 1977 when Radovan used it and became a pioneer in tissue expansion (5). It’s not until then, plastic surgeons adopted this technique for reconstruction of other parts of the body; one would be for scalp reconstruction (6).
It is a technique used for stretching the tissue to a certain amount for reconstruction. It involves using an expandable balloon filled with a fluid beneath the tissue to be expanded repeatedly (7,8).
It’s been observed that the complication rates increase with repeated usage of TE on the same tissue multiple times (9). Tissue expansion is considered to be the optimal method used to grow skin with the same characteristics of the surrounding normal skin in terms of color, texture and thickness, and create minimal scars possible and reduce the risk of rejection (10). Furthermore, for new skin to be created, a sequence of signaling pathway should be activated. This is only possible when the skin is put under tension to be stretched to a certain level with the help of TE (10). In general, it is considered to be a safe procedure; however, caution must be taken when used in pediatric age group due to possible negative effects on the craniofacial growth (8). In our case, T.E. was used thrice with no complications noted on the patient. In addition, according to Lo-Giudice et al. (9), in patients with hair loss more than 50%, using TE is not efficacious. However, in our case the patient’s hair loss was approximately 78%; yet TE was used successfully.
There are certain factors in our case that helped in accomplishing such successful outcome. To begin with, our patient had a great support system represented by her parents. Not to mention, the compliance of the patient and the close follow up were all factors that contributed to the successful outcome. Also, it has been noted that excision of nevus is optimally done at childhood due to the great risk it imposes for the nevus to be transformed into a malignant one (11). To clarify, 70% of patients with a giant congenital melanocyte experienced malignancy by the age of thirteen years. Also, those patients have a 51.4% greater risk to develop melanoma than the rest of the population. (11). Despite the fact that many options are available for excision of a nevus, surgical excision of a congenital nevus remains to be the most effective (12). There are several reconstructive methods used after the excision of the lesion including grafts, local and free flaps and expanders. However, in cases of giant lesions, multi-staged TE is the only option for treatment (13).
The disadvantages of multi-staged TE for treating this case include multiple hospital admissions and the complications that may arise from anesthesia and the surgery. Another disadvantage would be the long period it takes to see the final outcome. Thus, complete dedication and patience from the parents and the patient is a must.
Nonetheless, this technique provides excellent functional and cosmetic outcome for lesions that occupies ass large area of the body.
Conclusion
Tissue expander is widely used to construct areas of the body where grafts cannot be used. In general, it is considered to be a safe procedure; however, when used in pediatric age group, care must be taken into consideration. Due to its effect on the growth of the cranium, tissue expanders are usually not used more than twice in children in most cases. In our case, T.E. was used thrice with no complications noted on the patient. Thus, using it more than two times in certain conditions with children may result in favorable outcomes rather than disastrous ones.
Conflict of Interest
All authors state that they have no conflict of interests.
Data Availability
All data used to support the findings of this study are included within the article and the reference.
REFERENCES
- Shimizu H. Shimizu's textbook of dermatology. 1st ed. Hokkaido University, Japan, 2007.
- Krengel S, Reyes-Mugica M. Melanoma risk in congenital melanocytic naevi. Br J Dermatol. 2017;176(5):1114.
- Coran A, Adzick N. Pediatric surgery. 7th ed. Elsevier Mosby; 2012.
- Mutti L, Mascarenhas M, Paiva J, et al. Giant congenital melanocytic nevi: 40 years of experience with the serial excision technique. An Bras Dermatol. 2017;92(2):256-9.
- Bertozzi N, Pesce M, Santi P, et al. Tissue expansion for breast reconstruction: Methods and techniques. Ann Med Surg. 2017;21:34-4.
- Paletta C, Campbell E, Shehadi S. Tissue expanders in children. J Pediatr Surg. 1991;26(1):22-5.
- Neumann CG. The expansion of an area of skin by progressive distention of a subcutaneous balloon: Use of the method for securing skin for subtotal reconstruction of the ear. Plast Reconstr Surg. 1957;19(2):124-30.
- Williams NS, OConnell PR, McCaskie AW. Bailey & Loves short practice of surgery. Boca Raton: CRC Press - Taylor & Francis Group.2013.
- LoGiudice J, Gosain A. Pediatric tissue expansion: Indications and complications. J Craniofac Surg. 2003;14(6):866-72.
- Chen Y, Wang X, Lin G, et al. Successful treatment following early recognition of a case of Fournier’s scrotal gangrene after a perianal abscess debridement: a case report. 2018.
- Arneja J, Gosain A. Giant congenital melanocytic nevi. Plast Reconstr Surg.2009;124(Supplement):1e-13e.
- Gosain A, Santoro T, Larson D, et al. Giant congenital nevi: a 20-year experience and an algorithm for their management. Plast Reconstr Surg.2001;108(3):622-31.
- Kryger Z, Bauer B. Surgical management of large and giant congenital pigmented nevi of the lower extremity. Plast Reconstr Surg. 2008;121(5):1674-84.