Pharmacokinetics and safety of nanodrugs
Received: 03-Jan-2022, Manuscript No. PULJNN-22-4499; Editor assigned: 05-Jan-2022, Pre QC No. PULJNN-22-4499 (PQ); Reviewed: 19-Jan-2022 QC No. PULJNN-22-4499 (Q); Revised: 21-Jan-2022, Manuscript No. PULJNN-22-4499 (R); Published: 27-Jan-2022, DOI: 10.37532/puljnn.22.6(1).02-04
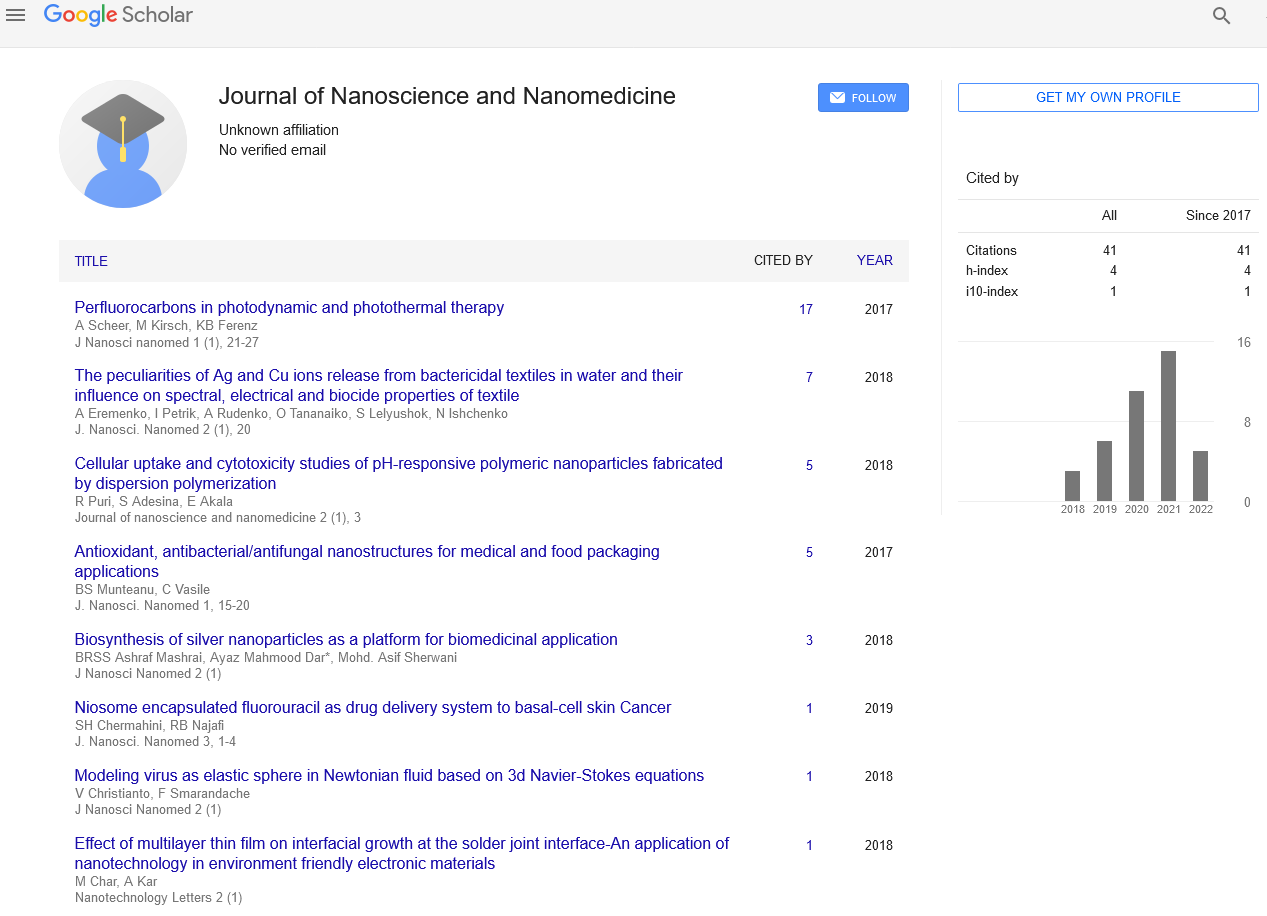
Citation: Collins S. Pharmacokinetics and safety of nanodrugs. J Nanosci Nanomed. 2022;6(1):2-4
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Dendrimers, nanocrystals, emulsions, liposomes, solid lipid nanoparticles, micelles, and polymeric nanoparticles are only a few of the nanodrug systems that have been produced so far for diverse routes of administration. Pharmaceutical compounds' effectiveness, safety, physicochemical qualities, and pharmacokinetic/ pharmacodynamic profile have all been improved using nanodrug systems. Functionalized nanodrug systems, in example, can improve the bioavailability of orally administered medications, extend the half-life of injectable pharmaceuticals (by lowering immunogenicity), and deliver drugs to specific tissues. As a result, nanodrug systems might reduce the frequency of administration while maximising pharmacological benefits and minimising systemic adverse effects, thereby improving treatment compliance and clinical results. Despite these appealing pharmacokinetic benefits, nanodrugs' hazardous potential has recently been highlighted, since they frequently demonstrate cytotoxicity, oxidative stress, inflammation, and genotoxicity in vitro and in vivo Red Blood Cells (RBCs) have recently inspired a new technique for producing biomimetic nanoparticles. Using membrane components produced directly from RBCs, this approach disguises drug nanocarriers as self. This approach has been shown to extend the half-life of particles in the systemic circulation beyond that of PEGylated systems. For the creation of effective nanodrugs with high therapeutic potential and a large safety margin, a greater knowledge of the pharmacokinetic and safety features of nanodrugs, as well as the constraints of each delivery strategy, is required. This study discusses current advances in nanodrug system development, with an emphasis on pharmacokinetic benefits and safety concern
Keywords
Nanodrug; Genotoxicity; Biocompatibility; Pharmaceutic; Pharmacodynamics
INTRODUCTION
Nanoscience has recently received a lot of attention, and there have been a lot of attempts in both academic and industry organisations to create and commercialise novel nanotechnology. Nanoscience is the study of phenomena and manipulation of materials at atomic, molecular, and macromolecular scales, where the properties differ significantly from those at a larger scale; and nanotechnologies is the design, characterization, production, and application of structures, devices, and systems by controlling shape and size at the nanometer scale, according to the Royal Society and Royal Academy of Engineering. Nanoscience and nanotechnology have revolutionised several industries, including breakthroughs in biology, electronics, cosmetics, food sciences, and pharmaceutics. Nanotechnologies, in particular, have a strategic application.
Nanodrug programmes are at the forefront of research into the rational delivery and targeting of pharmacological, therapeutic, and diagnostic substances. Early nanodrug efforts concentrated on enhancing the molecular characteristics of previously accessible therapeutic and diagnostic agents, but more recently, proponents of nanotechnology have sought to use novel therapeutic and diagnostic modalities to improve developability. precise drug targeting and distribution; increased safety and biocompatibility; speedier creation of novel medicine with a large safety margin; and enhanced pharmacokinetic behaviour are the main goals in the development of nanodrugs. Nanodrugs, in theory, can readily pass through tiny capillary blood capillaries and lymphatic endothelium, resulting in longer blood circulation durations or increased binding capacity and accumulation at some target areas. Nanotechnologies have been employed in the development of site-specific therapeutic targeting for the treatment of brain illnesses in particular. Nanodrugs may also cause a lower inflammatory and immunological response in tissues than larger-sized drugs [1]. Nanodrugs, despite their appealing properties, can cause oxidative stress, genetic damage, and the suppression of cell division and cell death, depending on their physicochemical properties (such as particle surface, size, and chemical composition). Because of the rising hazardous effects of nanodrugs and nanomaterials on living creatures, nanotoxicology is becoming an important subdiscipline of nanoscience and nanotechnology. The toxicity of nanoparticles, on the other hand, is poorly known due to a lack of adequate methodologies for assessing their safety. A greater knowledge of nanotoxicity and its processes would be extremely beneficial in the development of novel nanodrugs with a large safety margin. We examine current breakthroughs in nanodrug research as well as the pharmacokinetic/safety features of nanodrugs in this paper.
GENERAL PHARMACOKINETIC CHARACTERISTICS OF NANODRUGS
Over the last few decades, numerous efforts have been undertaken to manufacture nanodrugs, and the notion of nanodrugs has progressed significantly. Nanodrug systems come in a variety of shapes and sizes, with the majority of them including the drug enclosed in a carrier (eg, dendrimers, liposomes, micelles, and polymeric nanoparticles). A nanodrug system can provide a number of pharmacokinetic benefits, including targeted drug administration, high metabolic stability, high membrane permeability, enhanced bioavailability, and a long duration of action. As a result, nanodrug systems might be a potential strategy to obtaining drug characteristics by modifying the biopharmaceutic and pharmacokinetic features of novel drug candidates. The size, surface charge, and hydrophobicity of nanodrugs alter their mucosal absorption characteristics, and smaller nanodrugs have a greater transcellular uptake via follicle-associated epithelia than bigger ones [2]. Nanoparticles can enter cells by endocytotic processes such as caveolar- and clathrin-mediated endocytosis, potocytosis, pinocytosis, and patocytosis. Larger particles, on the other hand, can be swiftly opsonized and ejected from the circulation by Reticuloendothelial Macrophages (RES). It is vital to reduce opsonization and extend the circulation of nanoparticles in therapeutic application while designing nanoparticle formulations. Surface coating of nanoparticles with hydrophilic polymers/surfactants and/or formulation of nanoparticles with biodegradable copolymers having hydrophilic segments, such as Polyethylene Glycol (PEG), polyethylene oxide, poloxamer, poloxamine, and polysorbate , can be used to accomplish this . Due to the abundance of sulphate, sialic acid, and sugar moieties in mucus, nanodrugs with a positive surface charge can interact with the negative charges of mucin, resulting in accelerated transportation across mucus and higher internalisation by epithelial cells. The use of membrane permeability enhancers or ligands for receptors expressed on the cellular membrane to improve the transcellular transport of entrapped medicines may also be beneficial. Nanodrugs containing bioadhesive polymers or chelators, in addition to transcellular transport, might improve the paracellular transport of entrapped drugs by regulating tight junctions. Surface modification of nanodrugs with specific proteins, antibodies, and other biomolecules can be utilised to create drugs that target certain tissues selectively and this method has been used to boost therapeutic potential and lessen adverse effects of various anticancer medications. In general, nanotechnology-based drug delivery systems are designed to be delivered through injection, transdermally, or orally, while recent research has shown that pulmonary administration of nanodrug systems has promising results. Inhaled particles are cleared by the lungs, including mucociliary clearance and macrophage clearance, resulting in a short duration of action [3]. Nanoparticles, on the other hand, have been lauded for their favourable drug delivery qualities to the lungs, such as avoiding mucociliary and macrophage clearance and allowing for extensive residence durations before breakdown or translocation by epithelial cells. As a result, the nanodrug method should improve the therapeutic potential of entrapped pharmaceuticals while also helping to speed up pharmaceutical development.
ENGINEERED NANOPARTICLES
Because the dissolving rate of a medication proportionately rises with increasing surface area of drug particles, a particle size reduction technique is commonly employed to boost solubility rate. Reduced particle size, as specified by the Prandtl boundary layer equation, would result in rapid dissolution due to a reduction in diffusion layer thickness, especially down to 5 m. Based on this, drug nanocrystal technology has been the focus of attention in the pharmaceutical industry, with the "bottom-up" (controlled precipitation) and "top-down" types of techniques being used to create drug nanosuspensions (wet-milling with beads, and high-pressure homogenization) [4]. The use of a hydrophilic polymer and surfactant to stabilise a nanosuspension is common in both bottom-up and top-down techniques. Following a drying process, drug nanoparticles are disseminated in inert carriers [5].
CONCLUSION AND FUTURE OUTLOOK
The important biopharmaceutical characteristics of drug candidates in pharmaceutical research and development are 1) solubility; 2) membrane permeability; 3) metabolic stability; and 4) systemic pharmacokinetics and pharmacodynamics; all of these factors have a significant impact on the drugability and developability of new pharmaceutical products. Nanodrug methods may be able to overcome biopharmaceutical issues such as inadequate drug release control, poor stability, restricted pharmacokinetic behaviour, and active component toxicity. In recent years, as many as 70% of novel drug candidates have demonstrated poor water solubility, and 40% of marketed oral medicines have been found to be effectively insoluble in aqueous solutions (100 g/mL). 38 Some nanodrug techniques have been proven to be effective in enhancing the dissolving behaviour of BCS medicines
REFERENCES
- Devalapally H, Chakilam A, Amiji MM. Role of nanotechnology in pharmaceutical product development. J Pharm Sci. 2007;96(10):2547–2565.
Google Scholar Cross Ref - Naahidi S, Jafari M, Edalat F, et al. Biocompatibility of engineered nanoparticles for drug delivery. J Control Release. 2013;166(2):182–194.
Google Scholar Cross Ref - Petros RA, DeSimone JM. Strategies in the design of nanoparticles for therapeutic applications. Nat Rev Drug Discov. 2010;9(8):615–627.
Google Scholar Cross Ref - Yang W, Peters JI, Williams RO. Inhaled nanoparticles – a current review. Int J Pharm. 2008;356(1–2):239–247.
Google Scholar Cross Ref - De Jong WH, Borm PJ. Drug delivery and nanoparticles: applications and hazards. Int J Nanomedicine. 2008;3(2):133–149.
Google Scholar Cross Ref