Profunda Femoris Variant Within the Sciatic Sheath
2 Department of Physiology and Anatomy, University of North Texas Health Science Center, TX, USA
Received: 02-Aug-2023, Manuscript No. ijav-23-6679; Editor assigned: 04-Aug-2023, Pre QC No. ijav-23-6679; Accepted Date: Aug 31, 2023; Reviewed: 18-Aug-2023 QC No. ijav-23-6679; Revised: 23-Aug-2023, Manuscript No. ijav-23-6679; Published: 31-Aug-2023, DOI: 10.37532/1308-4038.16(8).293
Citation: Flowers R. Profunda Femoris Variant within the Sciatic Sheath. Int J Anat Var. 2023;16(8):363-364.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
The profunda femoris artery (PFA) provides four perforating branches to supply blood to the deep thigh. During the dissection of a 64-year-old male cadaver, an enlarged perforating branch of the PFA was found piercing through the adductor magnus muscle while supplying the posterior compartment of the thigh. Perforating branches of the PFA commonly terminate in the posterior thigh, but this variant artery continues through the posterior leg and popliteal fossa after entering the sciatic sheath, terminating distal to the knee as muscular branches for both heads of the gastrocnemius and soleus muscles. The lower extremity has well-documented arterial variations; however, finding an artery within the sciatic sheath and providing muscular branches to the proximal leg is a notable variant. Knowledge of potential variations of branching of the PFA is clinically relevant in order to avoid possible surgical and radiological operative complications.
Keywords
Anatomical variant; Sciatic sheath; Posterior leg; Profunda femoris; Perforating artery
INTRODUCTION
During development, variations in the formation of arteries and veins are not uncommon. There are many signaling factors and cascades that orchestrate angiogenesis [1]. Alterations in these angiogenesis signaling cascades tend to follow similar paths and develop into variants of a typical developmental pattern, with some variants being more common than others [2]. In typical development, the profunda artery generally develops as a branch of the femoral artery in the proximal lower limb. The profunda artery develops branches to supply the anastomosing arterial network around the hip joints as well as the deep perforating branches that pierce the adductor magnus muscle which terminates in the posterior thigh and supplies the hamstring muscles with blood [2]. The PFA typically begins in the anterior compartment of the leg, passing through the adductor sheath to the posterior leg to become the popliteal artery, found in the popliteal fossa; branches of the popliteal artery then supply both heads of the gastrocnemius muscle before the popliteal artery bifurcates into the tibial and fibular arteries [3]. Upon review of the literature, no documentation of perforating branches of the PFA continuing beyond the posterior compartment of the thigh was shown.
Presented in this report is a case of a perforating artery arising from the profunda femoris artery extending beyond the posterior thigh and supplying blood to muscles of the lower limb.
CASE REPORT
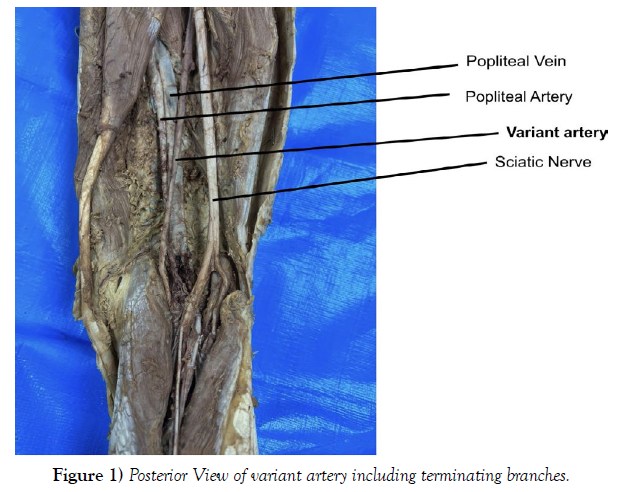
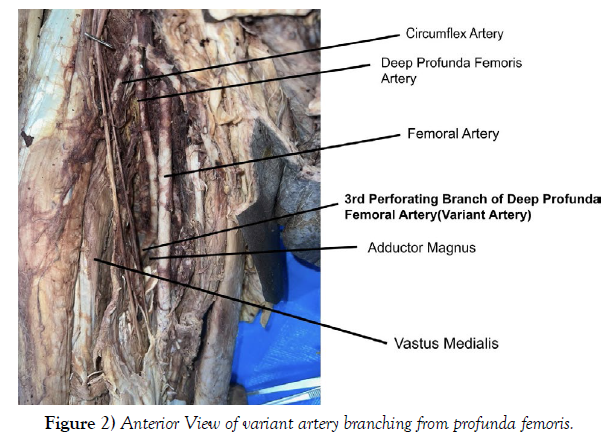
During the dissection of the lower extremity of a 64-year-old male, a variant of the 3rd perforating branch of the profunda femoris artery was identified. In the femoral triangle the profunda femoral artery branch of the femoral artery produced three perforating branches passes through the adductor magnus to supply the posterior muscles of the thigh (Figure 2). The first two perforating branches gave muscular branches of the posterior compartment. The Variant 3rd perforating branch was found running together with the sciatic nerve within the sciatic sheath (Figure 1).
This variant of the 3rd perforating branch of the profunda femoral artery was found superficial to the popliteal artery and vein within the popliteal fossa and terminated as muscular branches for the soleus muscle and both heads of the gastrocnemius (Figure 1).
The small saphenous vein was found running adjacent to the variant artery before it joined the popliteal vein as expected (not shown).
The sciatic nerve was traced from the gluteal region to its bifurcation as the tibial and common fibular nerves. Within the sciatic sheath, the variant artery followed the branches of the tibial nerve terminating along the sural nerve path (not shown).
DISCUSSION
Deep to the rectus femoris muscle and between the vastus medialis muscle and adductor magnus muscle, the profunda femoris artery provides perforating branches that give off cutaneous, anastomotic, and muscular branches to the flexor aspect of the thigh. There are typically three perforating arteries given off by the PFA, all of which pierce the adductor magnus to terminate as osseous and muscular branches for the flexor compartment of the thigh [4, 5]. The discovered variant artery was found in a location with two possible distinct embryological backgrounds - one within the sciatic sheath and one exiting off the profunda femoris artery. In the fetal lower extremities, the sciatic artery accompanies the sciatic nerve within its sheath during development [6]. In the fetus, the sciatic artery is a continuation of the internal iliac artery, supplying the lower limb buds with blood [7]. As the fetus develops, the lower axial artery and its derivatives - one being the sciatic artery - obliterate and in the process, the rete femorale develops to form the femoral artery and its derivatives6. From the rete femorale, the superficial and profunda femoris arteries begin to supply the leg, with the perforating branches of the profunda femoris supplying the posterior leg6. The third perforating branch is found below the adductor longus and supplies the adductor muscles, semitendinosus, semimembranosus, and biceps femoris [6]. The variant artery presented in this case maintains physiological properties and anatomical features of both the sciatic artery [7] and the third perforating branch of the profunda femoris artery [7].
In a review of sciatic artery variants found in literature, five types have been identified, some with subtypes, of different sciatic artery anomalies found in nature [8]. In this review, a description of a “Type 4” variant presents itself with an incomplete sciatic artery and completely developed femoral arteries [8]; within this type, only the lower half of the sciatic artery persists. The sciatic artery is an embryological branch of the lower axial artery that runs within the sciatic sheath and supplies the distal thigh and proximal leg in fetal development. The sciatic artery is found as a branch of the internal iliac artery and continues down the thigh to anastomose with the popliteal artery. Commonly, the sciatic artery regresses as the femoral artery and its branches develop to supply the distal thigh and proximal leg. In 0.05% of the population, a persistent sciatic artery (PSA) is found in the posterior thigh encased in the sciatic sheath [9]. While PSA is often asymptomatic, it can lead to aneurysms, thrombosis, or ischemia. As a major blood supplier of the lower extremity, recognizing this variant is of surgical importance to avoid undesired blood bypass [10]. It should be noted that in a separate study conducted on the thighs of 57 cadavers, a persistent sciatic artery found within the sciatic sheath [10] exhibiting similar characteristics to those in this case was reported.
However, the variant artery does not originate within the sciatic sheath and only enters the sheath in the posterior compartment. Additionally, the origin of the artery is from the profunda femoris, rather than the internal iliac artery [6]. While our variant is not a PSA, it has similar termination and muscular branches in the posterior thigh. Recognizing the continued third perforating branch will have similar surgical significance to the PSA.
While a continued third perforating branch has a surgical significance, it is also worth noting its importance in radiology and its use in nerve blocks. In 2021, a physician performed a Doppler ultrasound on a patient with a PSA. The physician noted that the artery was found within the sciatic sheath in the distal thigh near the bifurcation of the tibial nerve and common peroneal nerve [11]; this finding is similar in location to the presented variant artery of the cadaver in this case. In the 2021 study, the variant artery was avoided in a popliteal sciatic nerve block before left total knee replacement [11].
The physician’s ability to identify the anomaly on the ultrasound before injecting the nerve block prevented any detriment to the patient.
The variant artery in this case was concluded to be a congenital anomaly presenting as a continuation of the third perforating branch of the profunda femoris artery. The artery enters the sciatic sheath in the posterior thigh and continues to the posterior leg accompanying the sciatic nerve. The artery supplies the posterior compartment of the thigh and both heads of the gastrocnemius muscle as well as the soleus. Initially, this variant was thought to be a persistent sciatic artery because it was found within the sciatic sheath6. However, as presented in the case, this artery likely persisted from early development and entered the sciatic sheath just superior to the popliteal fossa. This finding would be surgically relevant in knee and femoral surgeries [9] and radiologically relevant in nerve-blocking treatment [11].
ACKNOWLEDGEMENTS
The authors would like to acknowledge the cadaveric donor and their family for their contribution to medical research and education.
REFERENCES
- Wang H, Chen ZF, Anderson D. Molecular Distinction and Angiogenic Interaction between Embryonic Arteries and Veins Revealed by Ephrin-B2 and Its Receptor Eph-B4. Cell. 1998; 93(5): 741–753.
- Massoud T, Fletcher EWL. Anatomical Variants of the Profunda Femoris Artery: An Angiographic Study. Surg Radiol Anat. 1997; 19(2): 99–103.
- Lamprecht D, Geldenhuys EM, Witbooi LR, Baatjes K. Popliteal Artery Anatomy: An Angiographic Description of Variants. Transl Res Anat. 2021; (24): 100127.
- Levin S, Baumeister, S. Flaps and Reconstructive Surgery. W.B. Saunders. 2009; 63–70.
- Kawasaki Y, Kinose S, Kato K, Sakai T, Ichimura K. Anatomic Characterization of the Femoral Nutrient Artery: Application to Fracture and Surgery of the Femur. Clin Anat. 2020; 33(4): 479–487.
- Khmara T. Anatomic Variability of Branches of Iliac and Femoral Arteries in Human Fetuses. ABMU. 2019. 54(1): 78–88.
- Brantley SK, Rigdon EE, Raju S. Persistent sciatic artery: embryology, pathology, and treatment. J Vasc Surg. 1993; 18(2): 242–248.
- Van-Hooft IM, Zeebregts CJ, Van Sterkenburg SMM, De Vries WR, Reijnen MMPJ. The Persistent Sciatic Artery. Eur J Vasc Endvasc Surg. 2009; 37(5): 585–591.
- Marincola BC, Napol A, Anzide Mi, Marotta E, Boni F et al. An Aneurysm at the Back of a Thigh: A Rare Presentation of a Congenitally Persistent Sciatic Artery. Eur J of Vasc and Endvasc Surg. 2000; 19(1): 99–100.
- Brantley SK, Rigdon EE, Raju S. Persistent Sciatic Artery: Embryology, Pathology, and Treatment. J Vasc Surg. 1993; 18(2): 242–248.
- Ogami-Takamura K, Murata H, Hara T. Persistent Sciatic Artery within the Paraneural Sheath of the Sciatic Nerve at Popliteal Fossa. JA Clin Rep. 2021: 7(74).
Indexed at , Google Scholar , Cross Ref
Indexed at , Google Scholar , Cross Ref
Indexed at , Google Scholar , Cross Ref
Indexed at , Google Scholar , Cross Ref
Indexed at , Google Scholar , Cross Ref
Indexed at , Google Scholar , Cross Ref
Indexed at , Google Scholar , Cross Ref
Indexed at , Google Scholar , Cross Ref
Indexed at , Google Scholar , Cross Ref