Radial artery mycotic aneurysm due to infective endocarditis: A case report and review of literature
2 Department of Surgery, University of North Carolina School of Medicine, Chapel Hill, NC 27599, United States, Email: aitranmer@carilionclinic.org
Received: 23-Jul-2018 Accepted Date: Sep 05, 2018; Published: 12-Sep-2018
Citation: Tranmer AI, Kalmar CL, Applebaum MA, et al. Radial artery mycotic aneurysm due to infective endocarditis: A case report and review of literature. J Vas Dis Treat. 2018;2(3):1-3.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Mycotic aneurysms of the peripheral arteries are rare but significant complications of infective endocarditis. We report the case of a 51-year-old right hand dominant male with a history of infective endocarditis who presented with an enlarging, pulsatile mass in the left hand. Work up revealed a mycotic aneurysm in the dorsal branch of the left radial artery. The patient was treated with resection of the aneurysm and revascularization using a reverse interposition sa-phenous vein graft. The patient had a successful recovery without lasting neurologic deficits, signs of vascular insufficiency, or recurrence.
Keywords
Mycotic aneurysm; Infective endocarditis; Radial artery; Saphenous vein graft
Sir William Osler initially coined the term mycotic aneurysm in 1885 when treating a patient with bacterial endocarditis [1]. Mycotic aneurysm formation in the setting of infective endocarditis is a known complication with an incidence ranging from 27-54% [2]. In 1887, Eppinger successfully identified the same pathogen present on a valvular heart vegetation as at a mycotic aneurysm. Cerebral arteries are the most commonly affected, followed by the aorta. Peripheral arteries account for less than 10% of mycotic aneurysms [3]. Peripheral mycotic aneurysms can lead to a myriad of complications including hemorrhage, limb loss, or death. The original surgical treatment of radial artery mycotic aneurysms was surgical ligation due to the risk of downstream emboli. Initially performed by Clutton and Dudgeon in 1907, ligation remained the gold standard for decades. Advancements in vascular and microvascular surgery have allowed for excision with revascularization in the appropriate clinical setting. We present a case of successful treatment of a mycotic aneurysm in the dorsal branch of the radial artery, as well as a literature review, that was encountered in a tertiary referral center.
Case Presentation
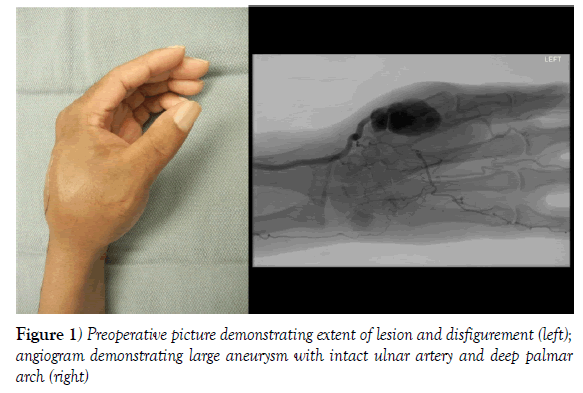
A 51-year-old right hand dominant male presented to the hand surgery team with a history of intracranial and thoracic mycotic aneurysms caused by infective endocarditis. His cardiac procedure was performed and the patient was referred to hand surgery with the chief complaint of an enlarging, pulsatile mass in the first web space of his left hand. This was first noted several months earlier and had slowly grown in size. The mass was painful and enlarging prompting the referral to hand surgery. Angiogram revealed a 3.5 x 2.5 cm pseudoaneurysm of the radial artery at the origin of the dorsal branch entering the first web space (Figure 1). The flow to the hand appeared to be radially dominant with an incomplete superficial arch. His hand was neurovascularly intact, therefore, surgery was performed after an interval to allow recovery from his thoracic aorta repair, to allow completion of IV antibiotic therapy, and to allow a suitable interval where the cardiothoracic surgery team felt comfortable holding therapeutic anticoagulation in the immediate perioperative period.
Figure 1) Preoperative picture demonstrating extent of lesion and disfigurement (left); angiogram demonstrating large aneurysm with intact ulnar artery and deep palmar arch (right)
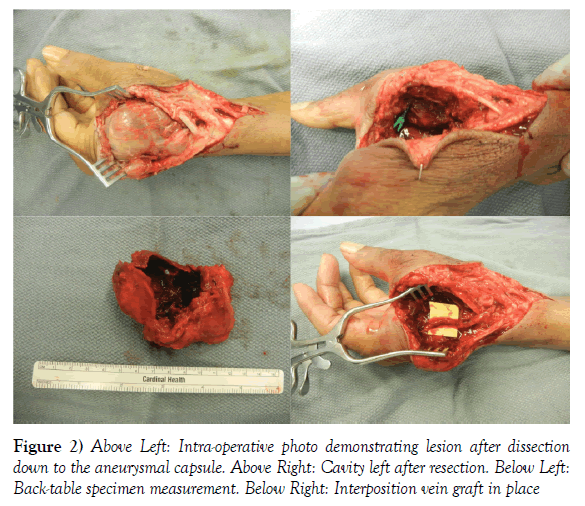
The patient was taken to the operative suite for aneurysm resection and vascular reconstruction with a reverse interposition saphenous vein graft. The decision for revascularization was based on preoperative Allen’s test with doppler exam of each digit, which revealed radial dominant blood flow; it was therefore felt that revascularization was the best option for the patient. Intraoperatively, the capsule of the aneurysm was noted to be much larger than the estimated, with the final pathology specimen measuring 7.2 x 5.8 x 3.6 cm (Figure 2). The patient left the operating room with good capillary refill and audible Doppler signals in all digits. Postoperatively, his ongoing anticoagulation requirements contributed to a post-operative hematoma in the cavity created by excision of the large mycotic aneurysm. The hematoma was treated non-operatively and resolved spontaneously. The patient progressed well over the next several months with sensation intact and adequate vascular supply to all digits (Figure 3).
Discussion
Mycotic aneurysms are abnormal irreversible focal arterial dilations associated with infection. William Osler termed this pathology in 1885 noting an association of mycotic aneurysms with emboli from infective endocarditis [1]. Pathogens gaining access to the arterial wall promote destruction and consequently compromise the integrity of the wall, resulting in focal dilation. Arteries can become infected through endogenous (embolism, septicemia) and exogenous (trauma, iatrogenic) sources. Previously existing aneurysms may also become secondarily infected. Any aneurysm associated with infection is termed a mycotic aneurysm and have poorer outcomes compared to non-infected aneurysms [4].
The intima is strongly resistant to inoculation, however any disruption this layer can predispose to infection. Intimal disruption is most often at areas of atherosclerosis, arteriovenous fistulas, bifurcations, and coarctations [3]. Four mechanisms can lead to mycotic aneurysms [1] septic emboli from infective endocarditis, [2] contiguous spread from local infection such as an abscess, [3] previously existent aneurysms due to another process such as atherosclerosis can become secondarily infected from a distant source in the context of bacteremia, and [4] direct inoculation due to trauma [3]. Most cases of infected upper extremity aneurysms are secondary to direct inoculation via intravenous drug abuse and endocarditis [3]. These two pathologies often occur hand in hand.
Staphylococcus aureus is the most commonly isolated bacterium responsible for peripheral mycotic aneurysms and, specifically, infected upper extremity aneurysms [3,5]. However, microorganisms are only recovered from wounds in approximately 25% of cases of clinically diagnosed mycotic aneurysms [3]. Moreover, blood cultures are positive in only 50-85% of patients with mycotic aneurysms [6]. Therefore, negative blood cultures do not exclude infected aneurysms.
Systemic embolization occurs in approximately 27-54% of patients with infective endocarditis, most often to the intracranial arteries [7,8]. Peripheral mycotic aneurysms as most often seen at the aorta. Upper extremity mycotic aneurysms occur in 10% of patients with infective endocarditis. The most common location in the upper extremity is noted to be the left brachial artery, suggested to be due to intravenous drug administration by a predominantly right-hand dominant population [9]. Hand mycotic aneurysms are only seen in 4-5% of patient with infective endocarditis [3,10].
Historically, mycotic aneurysms were generally only found on postmortem examination where they were discovered within the thoracic or abdominal cavities [11]. Modern imaging modalities have made intracranial, intrathoracic, and intra-abdominal aneurysms more readily diagnosable. Mycotic aneurysms in the periphery present as a pulsatile, tender mass often with overlying warmth and erythema. Systemic signs of infection such as fever are variably present. Physical exam and history are sufficient for the diagnosis, but arteriography is required for preoperative planning given individual arterial variation [4,12]. CT angiography can be an useful imaging modality and will often demonstrate saccular aneurysm or pseudoaneurysm.
All mycotic aneurysms require surgical ligation, excision, and debridement of all infected and devitalized tissue. Revascularization can be challenging given the infected operative field. Revascularization has been debated, but is often unnecessary in the upper extremity given the extensive collateral circulation and low metabolic demands of upper extremity muscle [4,9]. Upper extremity aneurysms are more likely to remain without need for revascularization than lower extremities. If there is concern for distal ischemia or vascular insufficiency to the digits, revascularization with saphenous vein graft may be necessary in uninfected tissue planes.
Preoperative and postoperative antibiotics are necessary for all mycotic aneurysms. Empiric antibiotics prior to the availability of wound cultures should include broad-spectrum gram-positive and gram-negative enteric coverage [3]. Once cultures and sensitivities are available, antibiotics should be tailored appropriately. Antibiotics are recommended for at least six weeks, however there is no consensus on the exact duration. Much of the decision-making requires consideration of current immunologic status and other comorbidities. For patients with comorbidities precluding operative intervention, antibiotic treatment alone might be adequate. There is evidence in the literature that small aneurysms (less than 10 mm) have regressed spontaneously with intravenous antibiotics alone, although it is emphasized that this this is not recommended in operative candidates [3].
Timing of surgical intervention is controversial. The risk of embolization is associated with the size of the cardiac vegetation, and the rate of embolization is known to decline over time following the initiation of antibiotics [13,14]. Given concomitant infective endocarditis along with a peripheral mycotic aneurysm, it is recommended to perform required operative procedures simultaneously, such as valve replacement and aneurysm resection [15]. Untreated mycotic aneurysms have the risk of rapid enlargement leading to rupture or thrombosis leading to showering of septic emboli downstream. Ischemia and limb lost due to compromised vasculature, neuropathy due to compression of local nerves, osteomyelitis due to local skeletal infection, and high output heart failure due to arteriovenous fistulae are serious complications from untreated mycotic aneurysms. Therefore, medical and surgical intervention is always indicated.
Prompt surgical management with continued antibiotic therapy generally results in favorable outcomes of the aneurysm and extremity. Hand aneurysms rarely have any neurologic sequela or limb loss when treated appropriately [3]. Most of the mortality of treated mycotic aneurysms is related to the underlying pathology, such as atherosclerosis, sepsis, or infective endocarditis [3].
Conclusion
Mycotic aneurysms of the upper extremities are a rare pathologic process that can have devastating consequences if not treated with appropriate surgical intervention. Careful history, physical exam, as shown in this case presentation by a judicious Allen’s test, and proper vascular imaging are required to determine the most suitable approach for each individual patient. Herein, we presented the successful management of a mycotic aneurysm of the dorsal branch of the left radial artery. Delayed referral after thoracic aorta aneurysm repair led to staged procedures. It was acknowledge that delayed repair of the peripheral mycotic aneurysm carried increased risk of hemorrhage, thrombosis, and distal emboli; however, it was felt to be in the patient’s best interest to allow further recovery from his aortic procedure. As discussed in both historic and recent literature, ligation and resection of mycotic aneurysms is often sufficient treatment in peripheral arteries. However, in this case, preoperative angiography and intra-operative findings demonstrated radial dominant blood supply to the hand and there was concern for subsequent digital ischemia if revascularization was not performed. Therefore, an interposition saphenous vein graft was used resulting in excellent reconstitution of flow to all digits.
REFERENCES
- Osler W. The Gulstonian Lectures on Malignant Endocarditis. Br Med J. 1885;1(1262):467-70.
- Kadowaki M, Hashimoto M, Nakashima M, et al. Radial Mycotic Aneurysm Complicated with Infective Endorcarditis Caused by Streptococcus Sanguinis. Intern Med. 2013;52(20):2361-65.
- Leon LR, Psalms SB, Labropoulos N, et al. Infected Upper Extremity Aneurysms: A Review. Eur J Vas Endovasc Surg. 2008; 35(3):320-31.
- Flanigan DP. Aneurysms of the Peripheral Arteries. In: Wesley S. Moore eds. Vascular and Endovascular Surgery: a Comprehensive Review. Elsevier/Saunders. 2013;708-720.
- Salzler G, Long B, Avgerinos ED, et al. Contemporary Results of Surgical Management of Peripheral Mycotic Aneurysms. Ann Vasc Surg. 2018;(18):30438-2.
- Johnson JR, Ledgerwood AM, Lucas CE. Mycotic aneurysm. New concepts in therapy. Arch Surg. 1983;118(5):577-82.
- Thuny F, Salvo GD, Belliard O, et al. Risk of embolism and death in infective endocarditis: prognostic value of echocardiography: a prospective multicenter study. Circulation. 2005;112(1):69-75.
- Hill EE, Herijgers P, Claus P, et al. Infective endocarditis: changing epidemiology and predictors of 6-month mortality: a prospective cohort study. Eur Heart J. 2007;28(2):196-203.
- Behera A, Menakuru SR, Jindal R. Vascular complications of drug abuse: an Indian experience. ANZ J Surg. 2003;73(12):1004-7.
- Brown SL, Busuttil RW, Baker JD, et al. Bacteriologic and surgical determinants of survival in patients with mycotic aneurysms. J Vasc Surg. 1984;1(4):541-7.
- Rogers L. Mycotic Aneurysms and Their Treatment. Annals of the Royal College of Surgeons of England. 1956;19(4):257-62.
- Niedenführ MR, Vázquez T, Nearn L, et al. Variations of the arterial pattern in the upper limb revisited: a morphological and statistical study, with a review of the literature. J Anat. 2001;199(5):547-66.
- Baddour LM, Wilson WR, Bayer AS, et al. Infective endocarditis: diagnosis, antimicrobial therapy, and management of complications: a statement for healthcare professionals from the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, and the Councils on Clinical Cardiology, Stroke, and Cardiovascular Surgery and Anesthesia, American Heart Association: endorsed by the Infectious Diseases Society of America. Circulation. 2005;111(23):e394-434.
- Steckelberg JM, Murphy JG, Ballard D, et al. Emboli in infective endocarditis: the prognostic value of echocardiography. Ann Intern Med. 1991;114(8):635-50.
- Kang DH, Kim YJ, Kim SH, et al. Early surgery versus conventional treatment for infective endocarditis. N Engl J Med. 2012;366(26): 2466-73.