Strengths-based approaches toward disrupting “silent expectations
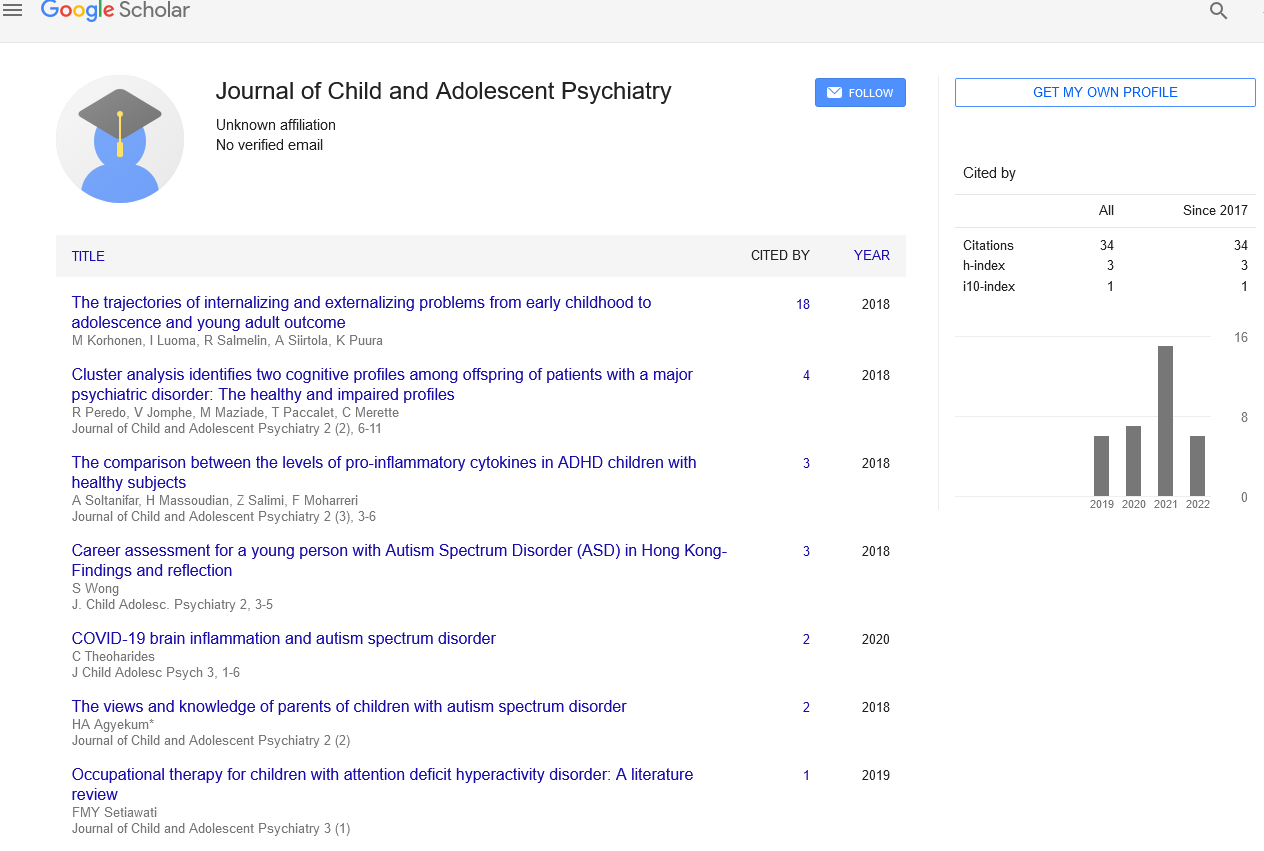
Received: 24-May-2022, Manuscript No. PULJCAP-22-5143; Editor assigned: 28-May-2022, Pre QC No. PULJCAP-22-5143(PQ); Accepted Date: Jul 03, 2022; Reviewed: 03-Jun-2022 QC No. PULJCAP-22-5143(Q); Revised: 10-Jun-2022, Manuscript No. PULJCAP-22-5143(R); Published: 05-Jul-2022, DOI: 10.37532/puljcap.2022.6(4)-44.
Citation: Hooper M. Strengths-based approaches towards disrupting �¢â�¬��silent expectationsâ�� Child Adolescent Psychiatry.2022; 6(4):44.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Usually, Personality disorders have their origins in infancy and adolescence; however, detecting BPD before eighteen years has been arguable. Many areas of the world are reluctant to detect BPD in youth because of the following fears: Firstly, Detection of BPD is not legal in teen years. Secondly, common characteristic of BPD; affective on consistency or disturb self-identity, are standard among youngsters. Thirdly, Personality growth is still in progress and this prevents diagnosis. Fourthly, BPD is a disapproving and negative word and clinicians try to protect patients from reprimanding and depressing behavior. The first three assumptions are proven wrong according to re- -search done in past few decades. Lot of evidence are available in support of both detecting and treating BPD in youth. It is found to be effective and consistent in youth as it is in adulthood similar consistency is observed in youth as with adulthood, it has additional rationality over other mental diseases diagnosis. Most importantly, disorder-specific therapy, especially early intervention, is effective. Thus, national treatment guidelines, Section 3 of the new DSM-5, and the proposed International Classification of Diseases, 11th Revision, personality disorder classification have all recently confirmed the legitimacy of the BPD diagnosis in adolescents. This highlights the need to communicate this new knowledge about BPD in adolescence to healthcare professionals.
Key Words
Personality disorders.
Introduction
Young folks' proclivity for rash and self-destructive behavior puts them at risk for negative health consequences. BPD is characterized by both repeated No Suicidal Self-Injury (NSSI) and suicide conduct, and most people with BPD have a lengthy history of repetitive self-behavior that dates back to infancy or youth. The utmost commonly satisfied BPD criteria among teenagers with BPD is "self-harm and suicidal behavior." This is in contrast to maturity when self-harm and suicidal behavior is on the wane. BPD traits best forecast sustained participation in NSSI over a year and repeat suicide attempts 6 months following hospitalization in young people. Patients with BPD account for 9% to 33% of all suicides, with an estimated lifetime suicide rate of 8%.
There is a dearth of precise information on suicide among teenagers with BPD, and one unsolved problem is the timing of suicide during BPD. Suicide rates are higher in studies with short follow-up periods, advising that the first few years after critical clinical treatment may be the most dangerous. The current evidence confirms the impact of BPD on the life of service users, their lifelong functioning, and the associated impact on health services because of the high occurrence of service use amongst the set. This highlights the importance of assessing the awareness amongst the medical community concerning diagnosing BPD in adolescents.
As we know, the new diagnostic manuals have affirmed the legality of BPD detection in youngsters, this systemically-informed review aimed to explore whether clinicians and researchers are using the available manual to diagnose BPD in adolescents and to see whether there are any studies published on this topic (of diagnosing the borderline personality disorder in adolescents) using the DSM-5 criteria. The hypothesis was that not many clinicians or researchers are aware of or using the opportunity to diagnose and thus manage BPD in adolescents, i.e., early in the course of this illness. This would also in turn highlight if there are not many studies, there is an urgent necessity to transfer this new information about BPD in youngsters to healthcare professionals as we know from evidence that early diagnosis and treatment are the keys to any lifelong disorder such as BPD.