Traumatic adrenal haemorrhage secondary to blunt injury
Received: 12-Jun-2018 Accepted Date: Jul 06, 2018; Published: 11-Jul-2018
Citation: Hun CW. Traumatic adrenal haemorrhage secondary to blunt injury. Surg Case Rep. 2017;2(2):24-5.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Adrenal gland injury secondary to blunt abdominal trauma is relatively uncommon. The estimated incidence rate of the injury is approximately 2–3%. The non-specific clinical manifestations and lack of specific biochemical markers make its diagnosis difficult. Contrast-enhanced CT remains the gold standard for detecting this injury and its associated complications. Patient with bilateral adrenal injury should be carefully monitored as they are prone to develop life-threatening adrenal insufficiency and its complications. Majority of these patients are managed conservatively and surgery is only required in cases of active bleeding. However follow-up is required to ensure complete resolution of the haemorrhage and to rule out a true adrenal mass. We report a case of unilateral adrenal haemorrhage secondary to motor vehicle accident.
Keywords
Adrenal gland; Injury; Haemorrhage; CT scan
Adrenal hemorrhage is a relatively uncommon condition with a variable and nonspecific presentation that may lead to acute adrenal crisis, shock, and death unless it is recognized promptly and treated appropriately.
Case Presentation
A 59-year-old male motorcyclist was involved in a motor vehicle accident while riding at speed of 40 km/hr. He sustained right side chest pain and was brought to the emergency department immediately.
On arrival to hospital, the patient was alert with of GCS 15/15. His vital signs were stable. He was unable to lift up his right shoulder with tenderness over the right shoulder joint and right sided ribs. Lung auscultations were normal. There was tenderness at right hypochondrium with bedside focused assessment with sonography for trauma (FAST) scan revealed free fluid in the Morison’s pouch. Chest and right shoulder X-rays showed right 4th & 5th ribs and right scapular body fractures.
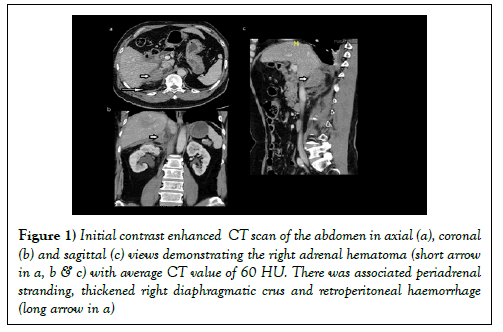
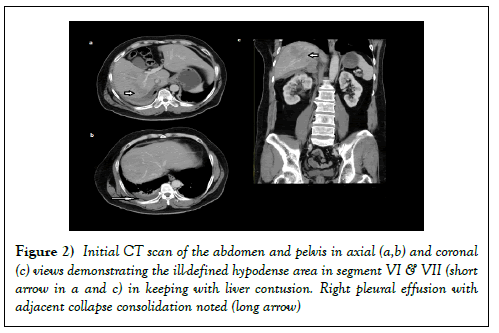
Contrast-enhanced CT scan (CECT) of thorax, abdomen and pelvis done to exclude internal injuries. CECT revealed an oval hyperdense lesion involving the right adrenal gland and extending posterior to it. There was associated peri-adrenal stranding, retroperitoneal haemorrhage and crural thickening (Figure 1). The left adrenal gland was normal. There were also ill-defined hypodense areas in segment VII and VI of liver in keeping with liver contusion (Figure 2). Other findings seen on CT included right pleural effusion with adjacent collapse consolidation (Figure 2).
Figure 1: Initial contrast enhanced CT scan of the abdomen in axial (a), coronal (b) and sagittal (c) views demonstrating the right adrenal hematoma (short arrow in a, b & c) with average CT value of 60 HU. There was associated periadrenal stranding, thickened right diaphragmatic crus and retroperitoneal haemorrhage (long arrow in a)
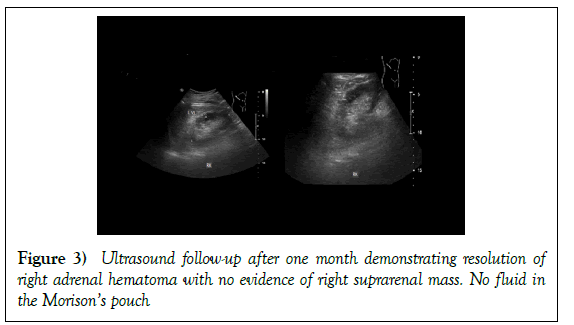
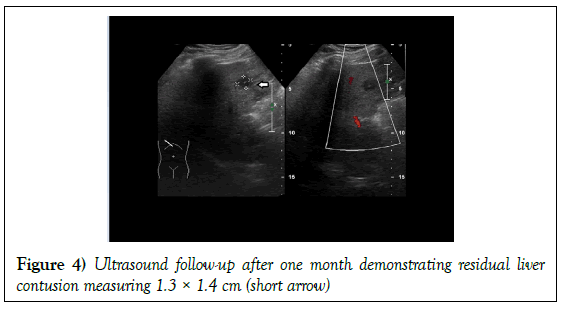
Patient was then admitted to orthopedic ward for conservative management of fractured right scapular body, right sided ribs, liver contusion and right adrenal haemorrhage. Daily monitoring of liver function and haemoglobin level was done and was normal. He also did not show signs of adrenal insufficiency. He was discharge well after one week. Follow-up ultrasound abdomen at one-month post injury (Figure 3) showed complete resolution of right adrenal haemorrhage, right retroperitoneal haemorrhage and residual liver contusion (Figure 4). No definite adrenal lesion was seen.
Discussion
Adrenal glands are bilateral small inverted V or Y shaped glands situated deep in the retroperitoneum. This organ is well cushioned by surrounding organs such as kidneys, liver, spleen, stomach and spine and therefore traumatic adrenal haemorrhage is relatively uncommon. The estimated incidence rate of adrenal gland injury after abdominal trauma is approximately 2–3% (1,2). In the past, before the advent of computed tomography (CT), diagnosis was difficult and was often made only at surgery or post-mortem. Today, the diagnosis of adrenal injuries can be quickly and accurately established by CT.
Mechanism of injury is postulated as direct compression between the spine and the other abdominal organs such as liver. Adrenal injuries are almost always associated with adjacent organ injuries, most commonly the liver, spleen or kidney. Liver trauma is the most commonly associated injury (43%), followed by ipsilateral renal injury (18%) (3). Ipsilateral rib fractures (39%) are also common.
Adrenal haemorrhage can be either unilateral or bilateral. In 75%–90% of cases, haemorrhage is unilateral and the most affected gland is the right adrenal (4). An isolated adrenal injury is even rarer, occurring in less than 5%. Possible explanations for this include the position of right adrenal gland in relatively tight quarters between the spine and the liver. Right adrenal gland is also expose to higher venous pressure than the left adrenal gland when increased abdominal pressure occurs during injury whereas on the left side, the high venous pressure are filtered by the left renal vein before reaching the left adrenal gland.
Majority of patients who sustain unilateral adrenal haemorrhage are clinically silent without obvious signs. Therefore diagnosis is usually made incidentally at imaging performed for another reason. Most frequent presenting symptom include abdominal pain and other rare presentation complains include flank pain, vomiting, nausea, hypotension, hypertension, a palpable flank mass, agitation, mental status change, and low-grade fever.
However bilateral adrenal haemorrhage often results in an adrenal insufficiency/ crisis, with coma and death if steroid replacement therapy is not administered promptly. Despite treatment, overall there is approximately 15% mortality, and about 50% if there is associated (5).
An abdominal CT is preferred to an ultrasound for assessment of the adrenals. The CT findings of adrenal trauma were focal hematoma appearing a round or ovoid nodules replacing the normal adrenal gland (30%), indistinct (27%) or enlarged (18%) adrenal gland, gross (15%) or focal (7%) adrenal haemorrhage, and adrenal mass (11%). Associated CT findings included periadrenal fat stranding (93%), retroperitoneal haemorrhage (22%), and thickened diaphragmatic crus (10%). Active adrenal bleeding was seen in 1.4% (6).
It is important to distinguish adrenal hematomas from incidental adrenal nodules, which are commonly seen incidentally. Measuring the Hounsfield units (HU) is useful because hematomas have high attenuation value than 50 HUs whereas other adrenal lesions such as adenoma often have attenuation measurement of less than 10 HUs. The age of hematoma also determine the HU unit in which acute to subacute haematomas contain areas of high attenuation that usually range from 50-90 HU. Over time as the hematoma resolving, the size and its HU units will be reduced.
Organised chronic adrenal haematoma appears as a mass with a hypoattenuating centre, with or without calcifications (also known as adrenal pseudocyst). Some adrenal haematomas may calcify after one year.
Adrenal trauma should not be considered an incidental finding because it can lead to severe bleeding, which may require a blood transfusion. Complication of adrenal gland injury includes adrenal vein rupture with haemorrhage both into the adrenal gland and in the retroperitoneum. Other potential complications that are infrequently encountered include adrenal infarction, adrenal vein thrombosis, hypertensive crisis and adrenal insufficiency although the exact incidence of these complications is not well known.
On the other hand, bilateral adrenal haemorrhage often results in an adrenal crisis, with coma and death resulting if steroid replacement therapy is not administered promptly. Despite treatment, overall mortality is approximately 15%. Bilateral adrenal haemorrhage with sepsis has a mortality rate of more than 90% (7).
Management of adrenal gland injury depends on the patient’s haemodynamic status, severity of the gland damage, bilateral gland involvement, and extent of bleeding within the gland. Majority of the patient (75%) were treated conservatively.
There are also rare reports of active adrenal haemorrhage requiring transarterial embolization to control bleeding.
There isn’t a standard protocol for the follow up of adrenal lesion in traumatic patient. When a definitive diagnosis is not possible on the initial CT scan, follow-up imaging in 6-12 weeks is reasonable (8). If the hematoma does not resolve or decrease in size over several weeks, another disorder should be considered. It must be considered that the distinction between tumoral from non-tumoral haemorrhage is really hard in acute phase, especially when a neoplastic mass is not well appreciable. For example, studies showed that 7-44% of adrenal pseudocyst (in which initially interpreted as chronic non-tumoral haemorrhage) was found to be neoplastic at surgery. Imaging findings suspicious of tumoral bleed are: intralesional calcifications (better seen at baseline CT), intralesional enhancement, and hypermetabolic activity at PET. According to the radioprotection criteria, if it is possible, MRI may be the first method of choice for follow-up because MRI manages to correctly evaluate the haemoglobin degradation and visualised the evolution of hematoma.
Conclusion
Adrenal injury due to blunt abdominal trauma is rare with prevalence of approximately 2% in patients undergoing CT scan post trauma. The frequency of adrenal injury increases with increasing severity of trauma. Adrenal gland injury is usually a result of massive trauma force associated with multiple injuries in blunt thoraco-abdominal trauma. Adrenal injuries are almost always associated with other injuries. It is important to recognise as mortality is twice as high in blunt trauma patients with adrenal gland injury than without. It may be potentially fatal if not correctly monitored and managed.
Most cases involve the right side and can be treated successfully using conservative management. Surgery is required only in cases of active bleeding.
REFERENCES
- Lin YH, Wu T. Isolated adrenal hemorrhage after blunt trauma: Case report and literature review. Urol Sci 2013;24(1):27-9.
- Chen KT, Lin TY, Foo NP, et al. Traumatic adrenal haematoma: A condition rarely recognised in the emergency department. Injury. 2007;38(5):584-7.
- Gabal-Shehab L, Alagiri M. Traumatic adrenal injuries. J Urol 2005;173(4):1330-1.
- Sayit AT, Sayit E, Gunbey HP, et al. Imaging of unilateral adrenal hemorrhages in patients after blunt abdominal trauma: Report of two cases. Chin J Traumatol 2017;20(1):52-5.
- Vella A, Nippoldt TB, Morris JC. Adrenal hemorrhage: A 25-year experience at the Mayo Clinic. Mayo Clinic Proceedings. 2001;76(2):161-8.
- Sinelnikov AO, Abujudeh HH, Chan D, et al. CT manifestations of adrenal trauma: experience with 73 cases. Emerg Radiol 2007;13(6):313-8.
- Xarli VP, Steele AA, Davis PJ, et al. Adrenal hemorrhage in the adult. Medicine. 1978;57(3):211-22.
- Terzolo M, Stigliano A, Chiodini I, et al. AME position statement on adrenal incidentaloma. Eur J Endocrinol 2011;164(6):851-70.