Ultrasound diagnosis of ovarian ectopic pregnancy after in vitro fertilization with salpingectomy and literature review
2 Department of Pathology, Hospital Universitari Dexeus, Barcelona, Spain, Email: francesc.tresserra@quironsalud.es
Received: 12-Aug-2017 Accepted Date: Aug 13, 2017; Published: 21-Aug-2017
Citation: Pascual MA, Hereter L, Graupera B, et al. Ultrasound diagnosis of ovarian ectopic pregnancy after in vitro fertilization with salpingectomy and literature review. J Reprod Biol Endocrinol. 2017;1(1):5-8.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Among ectopic pregnancies, ovarian ones are extremely rare and much less frequent with previous history of salpingectomy. Ultrasonographic diagnosis is feasible although differential diagnosis from the corpus luteum is difficult. The diagnosis includes medical history, physical examination, transvaginal ultrasonography with color and/or power Doppler and serum quantitative β-hCG levels. Monitoring of β-hCG levels and the accuracy of ultrasound diagnosis allowed conservative therapeutic strategy and proper postoperative course. This paper reports one case of right OEP with ipsilateral salpingectomy, and reviews the current concepts and the options for managing these rare types of ectopic pregnancies so to preserve the woman’s potential fertility.
Keywords
Ovarian pregnancy; Salpingectomy; Transvaginal ultrasonography; in vitro fertilization; Intra-cytoplasmatic sperm injection
Ovarian ectopic pregnancy (OEP) is an uncommon type of ectopic gestation that is difficult to diagnose, may even present as a complex adnexal mass mimicking an ovarian tumor [1,2] and is often discovered during surgery. OEP occurs naturally, but its incidence following in vitro fertilization and embryo transfer (IVF-ET) increases. Marcus and Brinsden [3] reported an incidence of 6% of OEP conceived after IVF-ET.
Primary OEP with previous ipsi or bilateral salpingectomy is extremely rare [4-9] and its pathophysiology is not sufficiently known. On the other hand, OEP after ICSI-ET is even rarer and just a few cases have been reported in literature [10-13].
The diagnosis of OEP includes medical history, physical examination, transvaginal ultrasonography (TUS) with color and/or power Doppler and serum quantitative β-hCG levels.
The following sonographic diagnostic criteria for the presence of an OEP have been suggested: a wide echogenic ring with an internal hypoechoic central area on the ovarian surface; the presence of ovarian cortex, including corpus luteum or follicles around the mass; and the echogenicity of the ring usually greater than that of the ovary itself [14].
This paper reports one case of right OEP after IVF and ICSI-ET with ipsilateral salpingectomy, and reviews the current concepts of their pathogenesis as well as the options for managing these rare types of ectopic pregnancy in order to preserve the woman’s potential fertility.
Case
A 31 year old woman, with previous right salpingectomy 1 year before, for right tubal pregnancy, was referred to our Reproduction Unit due to 3 years of primary infertility. The first IVF treatment was performed 12 months after salpingectomy. The patient underwent treatment for ovarian stimulation with antagonist of GnRH protocol, and 8 oocytes being obtained by transvaginal ultrasound; 4 of them were inseminated by conventional method and 4 by ICSI technique. Two embryos, one from ICSI and the other one from the conventional procedure were transferred back to the uterine cavity under guidance of transabdominal ultrasound following a technique previously published by us [15].
On the 24th day after ET, the patient went to the emergency room, relating pain and blood loss after 9 days of ET; TUS did not reveal an intrauterine or extrauterine gestational sac and the β-hCG level was 1,029 IU/L and the patient was referred to her gynecologist.
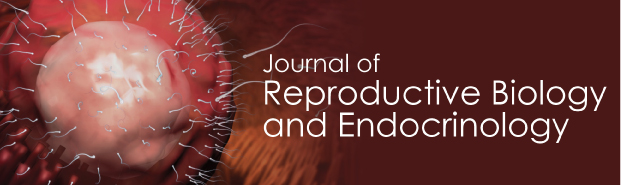
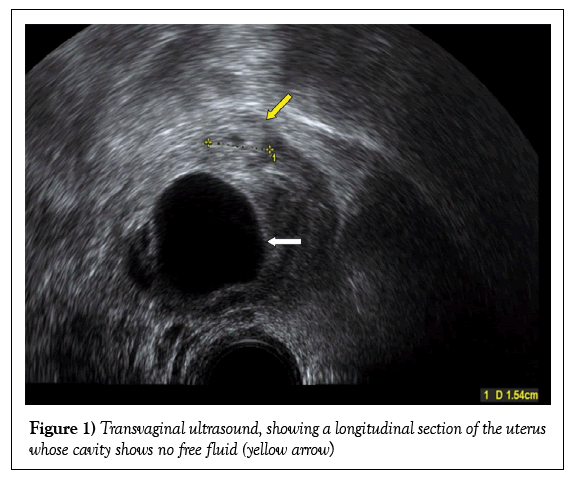
On the 26th day after ET, she presented pain in right iliac fosae. TUS examination was performed using a GE Voluson E8 machine (GE Medical Systems, Zipf, Austria); a thin endometrial lining with no intrauterine gestational sac was observed. No free fluid was observed in the uterine cavity, neither type A nor B [16] (Figure 1). The left ovary appeared normal with no suspicious mass in the ipsilateral tube. The right ovary was enlarged owing to a 29 mm unilocular anechoic cyst and a 15 mm thick echogenic wall surrounding a central hypoechoic structure clearly seen within the ovary (Figure 2). Serum β-hCG level was 1,163 IU/L.
Figure 2: Transvaginal ultrasound, which shows an enlarged right ovary, owing to a 29 mm unilocular anechoic cyst (white arrow) and a 15 mm thick echogenic wall surrounding a central hypoechoic structure clearly seen within the ovary (yellow arrow). This image suggests an ectopic pregnancy in the ovary
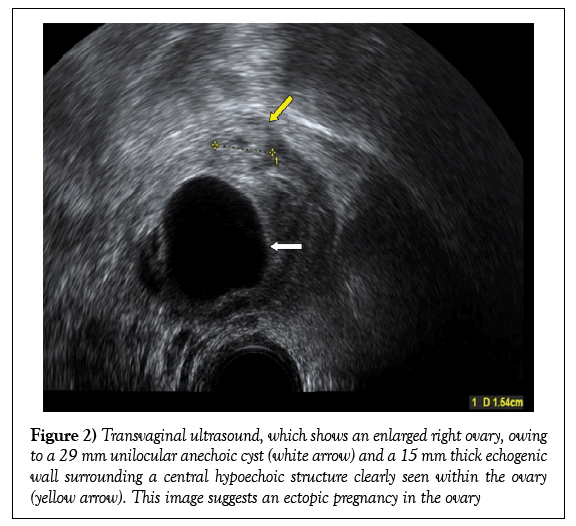
Two days later (28th day after ET) β-hCG level was 1,928 IU/L and TUS imaging of the ovary grew, measuring 19 mm and power Doppler study showed peripheral vascularity as a ring of fire (Figure 3), suspecting possible OEP. No free fluid was displayed in the pouch of Douglas. The patient previously gave informed consent for a laparoscopy, which was performed on the same day with the suspicion of ectopic pregnancy intimately attached to the right ovary or part thereof. Intraoperative laparoscopic evaluation revealed absence of right fallopian tube and the normal left fallopian tube; the uterus and left ovary were also normal. The enlarged right ovary contained the hemorrhagic corpus luteum and OEP. The OEP was identified and removed preserving the ovary. The postoperative period was uneventful and β-hCG returned to normal levels in a few days. The patient left the hospital the next day.
Figure 3: Transvaginal ultrasound with power Doppler that shows the same ovary two days later. We can see the image of ectopic pregnancy has grown (19 mm) (yellow arrow) and the mapping of color power shows peripheral vascularization (white arrows)
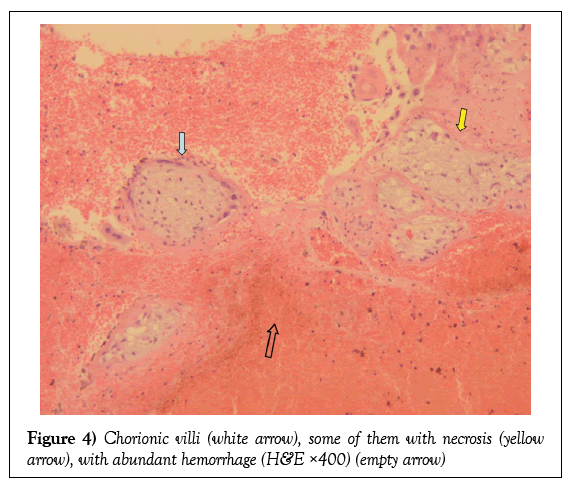
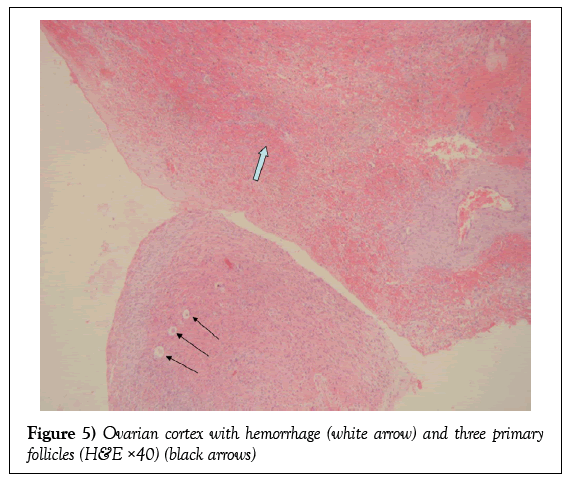
The histopathologic report showed hemorrhage and fibrin deposits including scant necrotic chorionic villi (Figure 4) and low amounts of extravillous trophoblast. No embryonic tissues were detected. The fibrinohematic material was attached to cortical ovarian fragments in which some primary follicles were seen (Figure 5).
Discussion
Ectopic pregnancy is one of the most frequent complications in patients undergoing assisted reproduction treatment, reaching an incidence of 4.5% [3].
We searched literature for articles reporting OEP published from 1990 through July, 2012. We investigated if it was a common pathology, if there was surgical history of salpingectomy, and whether assisted reproductive techniques were used. We also looked for diagnostic methodology and the types of treatments.
Joseph and Irvine [17], reviewing English language literature, found 250 reported cases, most of them case reports (1 to 3). But we have also identified longer series that set the rates as a percentage of OEP among total ectopic pregnancies, and the surgical procedure by which the treatment has been established [3,18-20]. Table 1 shows the series reported, including the number of cases and its rate as a percentage of OEP and their management.
| Authors | Cases | Management | OEP rate (%) |
|---|---|---|---|
| Marcus and Brinsden (3) | 7 | Laparoscopy | 6.0 |
| Seinera (21) | 8 | Laparoscopy | 2.6 |
| Bouyer (18) | 54 | Conservative | 3.2 |
| Raziel (20) | 19 | 10 laparoscopy 8 laparotomy 1 MTX |
2.7 |
| Odejinmi (19) | 12 | Laparoscopy | 2.9 |
Table 1: A review of the series, listing management and the ovarian ectopic pregnancy rates
Among the published papers, five cases of OEP were found in patients with a history of bilateral salpingectomy [4-6,8,9,21] and ipsilateral salpingectomy for the ovary affected by the OEP in one case [7]. In a patient with bilateral salpingectomy, ectopic pregnancy is an unexpected finding. In our case the patient had left tube patency; it may be considered that the transferred embryo migrated through the left tube to the right ovary. Another possibility would be that the placement of embryos into the uterine cavity through the catheter caused an iatrogenic perforation and consequent migration of the embryo; this possibility, in our case, is unlikely because the transfer was done under the ultrasound guidance technique according to that previously described by us [15], which allows us to precisely control the placement of the embryo and the path of the catheter. Also, migration of the embryo from the uterine cavity to the ovary through the fistulous tract in the intramyometrial portion of the tube has been suggested [7,8,22].
The mechanism of OEP after ICSI-ET is not sufficiently known, but there might be an association with prolonged in vitro culture in women who had undergone ICSI10. To our knowledge, only five previous cases of OEP have also been reported after the ICSI-ET [10-13]. These authors suggest that increased volume of culture medium and the injection pressure at the time of transfer would result in reverse migration. In our case transvaginal ultrasound-guided aspiration yielded 8 oocytes, of which 4 were injected. The resulting embryos were cultured until day 3 and two of them, one from ICSI technique and the other from the conventional technique were transferred on day 3. The two remaining embryos were cryopreserved.
The diagnosis of OEP requires medical history, physical examination, TUS with color and/or power Doppler and serum quantitative β-hCG levels. Symptoms often present with abdominal pain and vaginal bleeding [3,4,19], but can also be asymptomatic [3] or present symptomatology when there is advanced gestation [1,2].
In 1878, Spiegelberg [23] suggested four criteria to distinguish a primary ovarian pregnancy, and these criteria are still used today:
1) The Fallopian tube with its fimbria should be intact and separate from the ovary.
2) The gestational sac should occupy the normal position of the ovary.
3) The gestational sac should be connected to the uterus by the ovary ligament.
4) Ovarian tissue must be present in the specimen attached to the gestational sac.
However, these criteria probably misdiagnosed many OEPs, more often from patients with assisted reproduction treatments [24]; on the other hand, unfortunately, these are surgical criteria; none of these criteria can be established by ultrasonography.
The progress made in recent years with the availability of a highly specific radioimmunoassay for HCG, the improvement of TUS and widespread use of laparoscopy, have allowed early diagnosis of OEP. The sensitivity of diagnosing ectopic pregnancy using quantitative β-hCG in combination with TUS detection of an adnexal mass can be as high as 96% and the specificity 100% [25].
Ultrasound diagnosis of OEP shows the empty uterine cavity, the thickened endometrium and free fluid. It is difficult to make the differential diagnosis with a corpus luteum as both structures are located in the ovary. Some studies have showed that in stimulated ovaries, despite large size and vascularization, it is also possible to diagnose OEP with TUS and with serum quantitative β-hCG [26,27]. Comstock et al. [4] described the ultrasonic appearances suggestive of OEP as a wide echogenic ring surrounding a central hypoechoic structure; these findings have been documented in other case report [28,29]. In evaluation of the walls of the corpus luteum and the ectopics, Stein et al. [14] found that tubal ectopic rings were more echogenic than the corpus luteum. With respect to color Doppler, the results are controversial because there is an overlap distinguishing a corpus luteum from OEP. If a yolk sac or embryo can be seen, the diagnosis is established, but this is infrequent. The following sonographic diagnostic criteria for the presence of an OEP have been suggested: a wide echogenic ring with an internal hypoechoic central area on the ovarian surface; the presence of ovarian cortex, including corpus luteum or follicles around the mass; and the echogenicity of the ring usually greater than that of the ovary itself [14]. In our case imaging of the ovary showed a thick echogenic wall surrounding a central hypoechoic structure, clearly seen within the ovary, measuring 19 mm and power Doppler study showed peripheral vascularity as a ring of fire, suspecting possible OEP.
The therapy of early ovarian pregnancy is surgical in the first line, and in the event that the patient desires a future pregnancy, ovarian wedge resection is preferred; the conservation of ovarian tissue is the clinical goal of the treatment. Medical management is rarely used; only a few case reports describe the successful medical management of OEP with methotrexate, either intramuscular [30,31] or by local injection into the sac [32]. On the other hand, laparoscopic treatment with systemic methotrexate was reported as a good result [33,34]. Considering the great improvements in laparoscopic techniques, medical treatment with methotrexate would be relegated to a secondary option for incomplete resection or trophoblast persistence [26,33]. In our case continuous monitoring of the patient with serum values of β-hCG levels, and the detailed and thorough description of ultrasound findings of the right ovary allowed for a conservative therapeutic strategy and proper postoperative course.
Conclusion
In conclusion, early diagnosis of OEP is essential and is currently possible with the development of TUS with color and/or power Doppler associated with serum β-hCG levels, in order to perform conservative treatment with laparoscopy, with the objective of preserving fertility.
Acknowledgement
This work was performed under the auspices of the “Cátedra de Investigación en Obstetricia y Ginecologia” of the Department of Obstetrics and Gynecology, Hosptital Universitari Dexeus. Universitat Autònoma de Barcelona.
REFERENCES
- Chiapponi C, Trifoglio O, Chiapponi R. Complex ovarian pregnancy. Obstet Gynecol. 2012;119:478-9.
- Samaila MO, Adesiyun AG, Yusufu LM. Ovarian pregnancy presenting as ovarian tumour: Report of 2 cases. Ann Afr Med. 2007;6:36-8.
- Marcus SF, Brinsden PR. Primary ovarian pregnancy after in vitro fertilization and embryo transfer: Report of seven cases. Fertil Steril. 1993;60:167-9.
- Comstock C, Huston K, Lee W. The ultrasonographic appearance of ovarian ectopic pregnancies. Obstet Gynecol 2005;105:42-5.
- Cruciani L, Gerli S, Baiocchi G, et al. Ovarian pregnancy after in vitro fertilisation in a woman with previous bilateral salpingectomy. J Obstet Gynaecol. 2011;31:270-1.
- Han M, Kim J, Kim H, et al. Bilateral ovarian pregnancy after in vitro fertilization and embryo transfer in a patient with tubal factor infertility. J Assist Reprod Genet. 2004;21:181-3.
- Hong SY, Kim DW, Shin JH, et al. A case of ovarian pregnancy after ipsilateral partial salpingectomy. J Minim Invasive Gynecol. 2010;17:397-8.
- Hsu CC, Yang TT, Hsu CT. Ovarian pregnancy resulting from cornual fistulae in a woman who had undergone bilateral salpingectomy Fertil Steril. 2005;83:205-7.
- Seshadri S, Shirley P, Jaiganesh T, et al. in vitro fertilisation and embryo transfer for bilateral salpingectomies results in a ruptured ovarian ectopic pregnancy due to a tubal stump fistula: A case report and review of the literature. BMJ Case Rep. 2010;pii:bcr0920092291.
- Atabekoglu CS, Berker B, Dunder I. Ovarian ectopic pregnancy after intracytoplasmic sperm injection. Eur J Obstet Gynecol Reprod Biol. 2004;112:104-66.
- Dursun P, Gultekin M, Zeyneloglu HB. Ovarian ectopic pregnancy after ICSI-ET: A case report and literature review. Arch Gynecol Obstet. 2008;278:191-3.
- Oliveira FG, Abdelmassih V, Costa AL, et al. Rare association of ovarian implantation site for patients with heterotopic and with primary ectopic pregnancies after ICSI and blastocyst transfer. Hum Reprod. 2010;16:2227-9.
- Ramachandran A, Sharma S, Pratap K, et al. Ovarian pregnancy following intracytoplasmic sperm injection and embryo transfer: A case report. Case Rep Obstet Gynecol. 2012;2012:389107.
- Stein MW, Ricci ZJ, Novak L, et al. Sonographic comparison of the tubal ring of ectopic pregnancy with the corpus luteum. J Ultrasound Med. 2004;23:57-62.
- Coroleu B, Carreras O, Veiga A, et al. Embryo transfer under ultrasound guidance improves pregnancy rates after in vitro fertilization. Hum Reprod. 2000;15:616-20.
- Benson CB, Doubilet PM, Peters HE, et al. Intrauterine fluid with ectopic pregnancy. J Ultrasound Med. 2013;32:389-93.
- Joseph RJ, Irvine LM. Ovarian ectopic pregnancy: Aetiology, diagnosis and challenges in surgical management. J Obstet Gynaecol. 2012;32:472-4.
- Bouyer J, Coste J, Fernandez H, et al. Sites of ectopic pregnancy: A 10 year population-based study of 1800 cases. Hum Reprod. 2002;17:3224-30.
- Odejinmi F, Rizzuto MI, Macrae R, et al. Diagnosis and laparoscopic management of 12 consecutive cases of ovarian pregnancy and review of literature. J Minim Invasive Gynecol. 2009;16:354-9.
- Raziel A, Schachter M, Mordechai E, et al. Ovarian pregnancy - A 12 years’ experience of 19 cases in one institution. Eur J Obstet Gynecol Reprod Biol. 2004;114:92-6.
- Seinera P, Di Gregorio A, Arisio R, et al. Ovarian pregnancy and operative laparoscopy: Report of eight cases. Hum Reprod. 1997;12:608-10.
- Ben-Ami I, Panski M, Ushakov F, et al. Recurrent heterotopic pregnancy after bilateral salpingectomy in an IVF patient: Case report. J Assist Reprod Genet. 2006;23:333-5.
- Zur SO. Cuistik der ovarial schwangerschaft. Arch E Gynak. 1878;13:73-9.
- Sergent F, Mauger-Tinlot F, Gravier A, et al. Grossesses ovariennes: Reevaluation des critères diagnostiques. Gynecol Obstet Biol Reprod. 2002;31:741-6.
- Cacciatore B, Stenman UH, Ylöstalo P. Diagnosis of ectopic pregnancy by vaginal ultrasonography in combination with a discriminatory serum hCG level of 1000 IU/l (IRP). Br J Obstet Gynaecol. 1990;97:904-8.
- Einenkel J, Baier D, Horn LC, et al. Laparoscopic therapy of an intact primary ovarian pregnancy with ovarian hyperstimulation syndrome: Case report. Hum Reprod. 2000;15:2037-40.
- Riethmuller D, Sautière JL, Benoit S, et al. Diagnostic échographique et traitement laparoscopique d’une gossesse ovarienne. J Gynecol Obstet Biol Reprod. 1996;25:378-83.
- Atzori E. Transvaginal ultrasonography in the diagnosis of primary ovarian pregnancy: Case report. Ultrasound Obstet Gynecol. 1993;3:217-8.
- Ghi T, Banfi A, Marconi R, et al. Three-dimensional sonographic diagnosis of ovarian pregnancy. Ultrasound Obstet Gynecol. 2005;26:102-4.
- Kiran G, Guven AM, Köstü B. Systemic medical management of ovarian pregnancy. Int J Gynaecol Obstet. 2005;91:177-8.
- Shamma FN, Schwartz LB. Primary ovarian pregnancy successfully treated with methotrexate. Am J Obstet Gynecol. 1992;167:1307-8.
- Mittal S, Dadhwal V, Baurasi P. Successful medical management of ovarian pregnancy. Int J Gynaecol Obstet. 2003;80:309-10.
- Chelmow D, Gates E, Penzias AS. Laparoscopic diagnosis and methotrexate treatment of an ovarian pregnancy: A case report. Fertil Steril. 1994;62:879-81.
- Jourdain O, Fontanges M, Schiano A, et al. Management of other ectopic pregnancies (cornual, interstitial, angular, ovarian). J Gynecol Obstet Biol Reprod. 2003;32:S93-100.