Unraveling the Intricacies of Neuroanatomy in Clinical Practice: A Case Report
Received: 04-Jul-2023, Manuscript No. ijav-23-6605; Editor assigned: 05-Jul-2023, Pre QC No. ijav-23-6605 (PQ); Accepted Date: Jul 24, 2023; Reviewed: 19-Jul-2023 QC No. ijav-23-6605; Revised: 24-Jul-2023, Manuscript No. ijav-23-6605 (R); Published: 31-Jul-2023, DOI: 10.37532/1308-4038.16(7).285
Citation: Jassel P. Unraveling the Intricacies of Neuroanatomy in Clinical Practice: A Case Report. Int J Anat Var. 2023;16(7):345-346.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Neuroanatomy plays a crucial role in clinical practice, aiding healthcare professionals in diagnosing and managing neurological disorders. This case report highlights the significance of neuroanatomical knowledge in diagnosing a patient with a rare neurological condition. The case involves a 45-year-old male presenting with progressive gait disturbance and muscle weakness. A comprehensive neurological examination and diagnostic workup revealed a lesion in the corticospinal tract, emphasizing the importance of neuroanatomy in clinical decision-making and patient care.
Keywords
Neuroanatomy; Clinical practice; Corticospinal tract; Neurological examination; Diagnosis
INTRODUCTION
Neuroanatomy is the foundation of clinical neuroscience, enabling healthcare professionals to understand the intricate organization and functions of the nervous system. Accurate anatomical knowledge is essential in diagnosing and managing neurological conditions. This case report demonstrates the importance of neuroanatomy in clinical practice through the evaluation and management of a patient with a rare neurological disorder affecting the corticospinal tract [1-2].
CASE REPORT
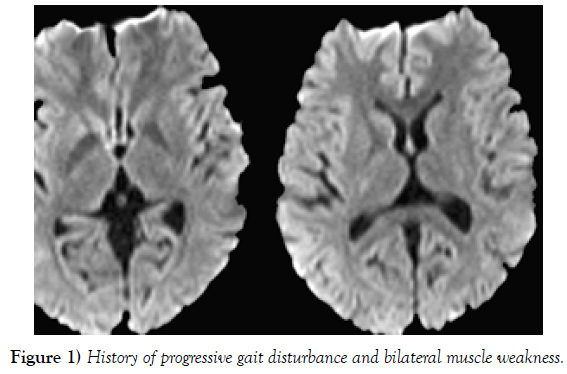
A 45-year-old male presented to the neurology clinic with a three-month history of progressive gait disturbance and bilateral muscle weakness. He reported stumbling frequently and difficulty lifting objects with his hands. Additionally, the patient complained of mild sensory changes in both lower limbs, primarily in the form of decreased vibratory sensation [3] (Figure 1).
Figure 1) History of progressive gait disturbance and bilateral muscle weakness.
Neurological Examination: Upon examination, the patient demonstrated spasticity in both lower limbs and exaggerated deep tendon reflexes. Babinski reflex was elicited bilaterally. The upper limbs exhibited no abnormalities, and cranial nerve examination was unremarkable [4]. Motor and sensory examination of the upper limbs did not reveal any deficits. However, the patient had difficulty performing heel-to-shin and finger-to-nose tests. Coordination appeared to be impaired [5].
DIAGNOSTIC WORKUP
Magnetic Resonance Imaging (MRI): Brain and spinal cord MRI with contrast revealed a well-defined, hyperintense lesion in the left corticospinal tract at the level of the internal capsule. The lesion extended from the internal capsule to the medullary pyramid. The rest of the brain and spinal cord appeared normal on imaging. Electromyography (EMG) and Nerve Conduction Studies (NCS): EMG and NCS were performed to assess the integrity of the peripheral nerves and muscles. The studies showed evidence of lower motor neuron involvement in the lower limbs, indicating the presence of a lesion affecting the corticospinal tract DISCUSSION The neurological examination and diagnostic workup pointed towards a lesion affecting the corticospinal tract, resulting in the patient’s clinical presentation. The corticospinal tract, also known as the pyramidal tract, is a crucial component of the motor system responsible for voluntary movement. It originates from the primary motor cortex and descends through the brainstem before crossing over to the contralateral side at the level of the medullary pyramids. The corticospinal tract continues its course in the spinal cord, influencing motor neurons that innervate skeletal muscles throughout the body [6].
Anatomy of the Corticospinal Tract: The corticospinal tract comprises two main divisions: the lateral corticospinal tract and the anterior corticospinal tract. The majority of fibers travel in the lateral corticospinal tract, which crosses over in the medullary pyramids and descends contralaterally in the spinal cord. These fibers synapse with motor neurons in the ventral horn of the spinal cord at various levels [7]. The anterior corticospinal tract, on the other hand, remains ipsilateral for a few spinal segments before crossing over and synapsing with lower motor neurons.
Clinical Implications: Lesions affecting the corticospinal tract can result from various etiologies, including vascular events, infections, demyelinating diseases, and neoplasms. In this case, the patient’s MRI revealed a well-defined lesion in the left corticospinal tract, which likely resulted in the observed spasticity, hyperreflexia, and weakness in the lower limbs.
The presence of a Babinski reflex is indicative of an upper motor neuron lesion, which aligns with the involvement of the corticospinal tract. The diminished coordination observed during the neurological examination suggests additional damage to the cerebellar pathways, potentially due to the close proximity of the lesion to other motor pathways in the internal capsule [8].
MANAGEMENT
The management of corticospinal tract lesions depends on the underlying cause. In this case, further investigations were initiated to identify the etiology. The patient’s medical history and laboratory tests ruled out infectious and inflammatory causes. Due to the lesion’s location and appearance, a neoplastic origin was suspected [9-10].
Surgical Intervention: Given the size and location of the lesion, surgical intervention was considered for tissue biopsy and potential resection. A neurosurgical consultation was sought, and the patient underwent stereotactic biopsy of the lesion. Histopathological examination confirmed the presence of an intracranial tumor classified as a low-grade glioma.
Postoperative Management: After surgical intervention, the patient received rehabilitation therapy to manage spasticity, improve motor function, and address coordination deficits. Physiotherapy, occupational therapy, and speech therapy were tailored to the patient’s specific needs.
Follow-up: The patient’s postoperative course was uneventful. Followup MRI showed a reduction in the size of the lesion, indicating a positive response to the surgical intervention. His gait improved significantly, and muscle strength gradually improved over time. However, mild residual spasticity remained.
CONCLUSION
This case report highlights the critical role of neuroanatomy in clinical practice, specifically in diagnosing and managing patients with neurological disorders. In this case, a lesion in the corticospinal tract was responsible for the patient’s progressive gait disturbance and muscle weakness. Accurate anatomical knowledge facilitated the precise localization of the lesion, leading to appropriate diagnostic and therapeutic decisions.
Understanding neuroanatomy aids clinicians in localizing neurological lesions, determining the type of deficits likely to be observed, and devising targeted treatment strategies. As technology and imaging techniques advance, neuroanatomy remains the cornerstone of neurological diagnosis and management, ensuring optimal patient care and outcomes.
ACKNOWLEDGEMENT
The authors would like to acknowledge the cadaveric donor and their family for their valuable contribution to medical education and research.
CONFLICT OF INTEREST
The authors declare no conflicts of interest related to this case report.
REFERENCES
- Krause DA, Youdas JW. Bilateral presence of a variant subscapularis muscle. Int J Anat Var. 2017; 10(4):79-80.
- Mann MR, Plutecki D, Janda P, Pękala J, Malinowski K, et al. The subscapularis muscle‐a meta‐analysis of its variations, prevalence, and anatomy. Clin Anat. 2023; 36(3):527-541.
- Pillay M, Jacob SM. Bilateral presence of axillary arch muscle passing through the posterior cord of the brachial plexus. Int. J. Morphol., 27(4):1047-1050, 2009.
- Pires LAS, Souza CFC, Teixeira AR, Leite TFO, Babinski MA, et al. Accessory subscapularis muscle–A forgotten variation?. Morphologie. 2017; 101(333):101-104.
- John C, Christian J. Commentary: Thoracic surgery residency: Not a spectator sport. J Thorac Cardiovasc Surg. 2020 Jun; 159(6):2345-2346.
- Anri S, Masayoshi O, Shigeru H. Glomerular Neovascularization in Nondiabetic Renal Allograft Is Associated with Calcineurin Inhibitor Toxicity. Nephron. 2020; 144 Suppl 1:37-42.
- Mamikonyan VR, Pivin EA, Krakhmaleva DA. Mechanisms of corneal neovascularization and modern options for its suppression. Vestn Oftalmo. 2016; 132(4):81-87.
- Gaigalaite V, Dementaviciene J, Vilimas A, Kalibatiene D. Association between the posterior part of the circle of Willis and vertebral artery hypoplasia. PLoS ONE. 2019; 14(9): e0213-226.
- Mujagic S, Kozic D, Huseinagic H, Smajlovic D. Symmetry, asymmetry and hypoplasia of intracranial internal carotid artery on magnetic resonance angiography. Acta Med Acad. 2016; 45:1- 9.
- Rusu MC, Vrapclu AD, Lazar M. A rare variant of accessory cerebral artery. Surg Radiol Anat. 2023; 45(5):523-526.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, , Google Scholar, Crossref
Indexed at, , Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref