In hospital outcomes of primary percutaneous intervention in patients presenting with acute myocardial infarction in Saudi Arabia – A single center study
2 Cardiology Fellow, King Faisal Cardiac Centre, King Saud Bin Abdulaziz Medical City, Jeddah, Saudi Arabia, Email: Bogamisa@ngha.med.sa
3 Consultant Nephrologist, King Faisal Cardiac Centre, King Saud Bin Abdulaziz Medical City, Jeddah, Saudi Arabia, Email: Bogamisa@ngha.med.sa
4 Consultant Adult Cardiology, King Faisal Cardiac Centre, King Saud Bin Abdulaziz Medical City, Jeddah, Saudi Arabia
5 Consultant Interventional Cardiologist, King Faisal Cardiac Centre, King Saud Bin Abdulaziz Medical City, Jeddah, Saudi Arabia, Email: Bogamisa@ngha.med.sa
Received: 23-Jan-2018 Accepted Date: Feb 06, 2018; Published: 12-Feb-2018, DOI: 10.4172/2368-0512.1000102
Citation: Bugami SA, Niaz A, Alabbadi M, et al. In hospital outcomes of primary percutaneous intervention in patients presenting with acute myocardial infarction in Saudi Arabia – A single center study. Curr Res Cardiol 2018;5(1):9-12.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
OBJECTIVE: To study the presentation, response to treatment, complication and prognosis of patients with acute ST-Elevation myocardial infarction (STEMI) who were treated with primary percutaneous coronary intervention (PPCI) at King Faisal Cardiac Center (KFCC) in the period from January 2015 till December 2016.
METHODS: Data of 77 patients with STEMI who were treated with primary PCI as a mode of reperfusion who presented to KFCC were collected retrospectively from January 2015 till December 2016. The primary end point was in hospital mortality.
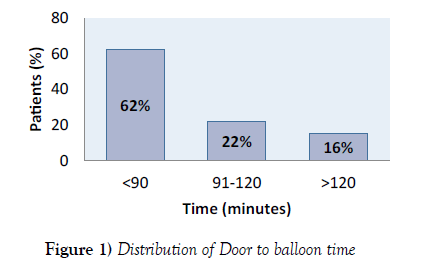
RESULTS: 77 patients with STEMI received PPCI. These were predominantly male (86%, no=66). The mean age was 57.9 (SD ± 11.8). History of Diabetes was present in (64.7%, no=49), hypertension (49% no=38) dyslipidemia (51% no=39) and smoking (41.6%, no=32). Chest pain was the most common presenting symptoms (97%, no=75). Only 5 patients (6%) presented to emergency department within 1 hour from chest pain onset. While 7 (8%) of patients presented beyond 12 hours the majority of patients arrived within 6 hours 29 patients (38%) and 37 patients (48%) arrived after 6 hours but within 12 hours from pain onset. The median door to balloon time was 84 minutes (IQR: 63.5- 111.5 minutes). Door to balloon time of less than 90 minutes was achieved in (62%, no=46) while D2B time of more than 90 minutes but within 120 minutes was seen in (22 %,) while (16%) had D2B time of more than 120 minutes. The left anterior descending artery was the culprit in 37 patients (48%) Femoral artery access was used in 48 patients (62%).The success of delivering the stent was 97% (no =75). The Median length of hospital stay was 3 days (IQR: 2-4). The primary endpoint of inhospital death was 5.1%.
CONCLUSION: Our findings suggest favorable outcomes of STEMI patients treated with PPCI, matching the international data. D2B time remains below acceptable standers. Regardless of logistic limitations Primary PCI should be the preferred method of reperfusion. Strategies towards increasing patient’s access and improving D2B time should be adopted.
Keywords
ST elevation myocardial infarction; Primary percutaneous coronary intervention; Door to balloon time
Introduction
The aim of acute treatment of ST elevation myocardial infarction (STEMI) is restoration of myocardial perfusion by recanalization of the occluded infarct related vessel. Early reperfusion is associated with better outcomes. Thrombolytic therapy and primary percutaneous coronary intervention (PPCI) are used as reperfusion strategies (1). Several randomized trials and meta-analyses have shown that primary angioplasty is superior to thrombolysis in the treatment of STEMI in terms of death, re infarction, and stroke (2-10). Although Primary percutaneous coronary intervention (PPCI) has been recognized as the treatment of choice for patients with (STEMI) widespread availability and access remains limited in Saudi Arabia. The Gulf Registry of Acute Coronary Events (Gulf RACE 2) from 6 Gulf countries including Saudi Arabia showed only 198 patients (10.8 %) treated with PPCI in a STEMI cohort of 1832 patients. The in-hospital mortality was 2.8% in 108 (54.5%) patients who were treated within 90 minutes of medical contacts (11). Optimal results of primary PCI are obtained if the procedure is performed in a timely manner (within 90 minutes from medical contact) at a high-volume center by expert operators (12).
King Faisal Cardiac Center (KFCC) is one of the primary centers which perform primary PCI as treatment for STEMI 24 hours 7 days a week in Jeddah, Saudi Arabia. To the best of our knowledge local outcome data in this group of patients are limited. The objective of this study is to ascertain the mode of presentation, describe patient’s clinical and angiographic characteristics and determine in hospital outcomes of patients presenting to KFCC with ST elevation MI who were treated with PPCI.
Patients and Methods
This is a cross sectional retrospective study. Data of consecutive patients above the age of 18 years hospitalized or presenting to emergency department with acute cardiac chest pain within 24 hours with ECG changes demonstrating ST-segment elevation of more than 1mm in more than 2 contiguous leads or new left bundle branch block who were treated with PPCI and had final discharge diagnosis of STEMI during the period from January 2015 till December 2016 were analyzed.
Patient who were transferred from other hospitals, those who received thrombolytics prior to percutaneous intervention in addition to those who died prior to intervention and Patients who had other causes of ST segment elevation who were taken to the catheterization laboratory for possible PPCI and had other diagnosis and finally post CABG patients were all excluded.
Information collected included, age, gender, history of diabetes (defined as a fasting glucose >126 mg/dl or on treatment), hyperlipidemia (fasting cholesterol >200 mg/dl or on treatment), hypertension (systolic blood pressure >140/90 mmHg or on treatment), smoking, left ventricular function (using echocardiography), presence of cardiogenic shock (defined as a systolic blood pressure of < 90 mmHg or requirement of inotropes to maintain a SBP > 90 mmHg). Angiographic and procedural details (culprit vessel, number of diseased vessels and use of stents). Hospital charts reviewed for further information including need of intubation, electrocardiogram (ECG) ST segment analysis and laboratory data includes hemoglobin, serum creatinine and cardiac enzymes etc. Timing variables have been ascertained including time to presentation which is defined as the time from symptom onset until arrival at the hospital. Door to balloon time (the time from arrival at the hospital until balloon inflation in cardiac catheterization laboratory).
PCI success is defined as achievement of vessel patency to a residual of <30%. Significant groin hematoma is defined as a hematoma > 10 cm in diameter or requiring blood transfusion. The primary end point was In-hospital mortality.
Statistical analysis
All the variables were entered into the Statistical Package for Social Sciences software, version 21 (SPSS Inc.) for data analysis. Descriptive statistics were computed and presented as means and standard deviations were calculated.
For continuous variables like age, LVEF and median for onset of pain to ER, door to balloon time in minutes. Categorical variables reported in percentages for the gender, hypertension, diabetes mellitus, Dyslipidemia, cardiogenic shock, left ventricular failure, multivessel diseases, procedural success and mortality.
Ethical Approval
All procedures performed in this study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments. Only patients’ medical records were reviewed (informed consent was not required). Patients’ files were approached in the Medical Record Department. The study met all institutional ethical board requirements.
Results
Total of 77 patients were included in this study. Table 1 shows the demographic and clinical characteristics of the studied cohort. The mean age was just over 57.9 (±11.8) years. There were 66 (86 %) males and 11 (14%) female, with 49 (64%) patients having diabetes, 38 (49%) hypertension, 39 (51%) dyslipidemia and 32 (41.6 %) were active smokers. Chest pain was the major presenting symptom in 75 (97 %) of the cohort followed by shortness of breath in 15 (19 %) patients. 2 patients had syncope and 3 had atypical presentation, one had low back pain and 2 had epigastric pain and vomiting. only 5 patients (6 %) presented within the first hour. The majority of patients 37 (48 %) presented unfortunately beyond 6 hours from symptoms onset.
| Variables | Statistics |
|---|---|
| Age, mean (SD) | 57.9 (±11.8) |
| Male | 66 (86%) |
| DM | 49 (64%) |
| HTN | 38 (49%) |
| Dyslipidaemia | 39 (51%) |
| FH of Premature IHD | 1 (1%) |
| Prior ASA use | 22 (29%) |
| CKD | 6 (8%) |
| Smoking | 32 (41.6%) |
| Presenting Complaints, n (%) | |
| Chest pain | 75 (97%) |
| SOB | 15 (19%) |
| Syncope | 2 (3%) |
| Cardiac arrest | 1 (1%) |
| Atypical | 3 (4%) |
| Time from pain Onset to presentation, n (%) | |
| Within 1 Hour | 5 (6%) |
| >1 to 6 Hours | 29 (38%) |
| >6 to 12 Hours | 37 (48%) |
| >12 Hours | 6 (8%) |
| Other findings | |
| Haemoglobin, Median (IQR) | 14.5 (IQR: 13.1, 15.5) |
| Haematocrit, Median (IQR) | 43.9 (IQR: 41.2,47,4) |
| Serum Creatinine, Median (IQR) | 82 (IQR: 70,97) |
| LVEF, Median (IQR) | 0.45 (IQR: 0.39,0.5) |
| Door-to-Balloon Time, Median (IQR) | 84min (IQR:63.5,111.5) |
| Length of stay Median (IQR) | 3 days (IQR: 2- 4) |
Table 1: Characteristics of patients undergoing PPCI for STEMI
The mean left ventricular ejection fraction was 45%.
The mean door to balloon time was 84 min. Door to balloon time of 90 minutes or less was achieved in 62% of the patients (Figure 1).
Table 2 shows the angiographic and procedural details. Left anterior descending artery (LAD) was the most commonly identified culprit vessel 37 (48 %) followed by right coronary artery 21 (27 %) and 9 (12%) left circumflex artery respectively. Majority 37 (48.1 %) patients had single vessel disease. Successful stent deployment achieved in 96 %. Procedure was successful in 75 (97 %) patients. Twenty-one (27 %) patients required thrombectomy. Six (7.7 %) patients needed intra-aortic balloon counter pulsation support. None required urgent surgery. Groin haematoma occurred in 4 patients (5%), acute stent thrombosis occurred in 1 (1.29 %) patient and four (5.1%) patients had contrast induced nephropathy. Four patients died in hospital (5.1%). Two patients died due to cardiogenic shock, one due Ventricular septal rupture and one due to acute stent thrombosis.
| Variables | n (%) |
|---|---|
| Extent of CAD | |
| 1VD | 37 (48.1%) |
| 2VD | 24 (31.2%) |
| 3VD | 16 (20.8%) |
| Culprit Artery | |
| LAD | 37 (48%) |
| RCA | 21 (27%) |
| LCX | 9 (12%) |
| OM | 7 (9%) |
| Others** | 3 (4%) |
| Radial Approach | 27 (35%) |
| Femoral Approach | 48 (62%) |
| Switch (from radial to femoral) | 2 (3%) |
| Stent | 74 (96%) |
| Drug eluting stent | 67 (87%) |
| Baremetal stents | 7 (9%) |
| Balloon only | 2 (3%) |
| Thrombectomy | 21 (27%) |
| Number of Stents, Median (IQR) | 1 (IQR: 1- 2) |
| 2b3a inhibitor | 34 (44.1%) |
| Complications | |
| No Reflow | 10 (13%) |
| Hematoma | 4 (5%) |
| Acute stent thrombosis | 1 (1.29%) |
| Cardiogenic Shock | 3 (3.8%) |
| VT/VF | 6 (7.7%) |
| Failed PCI | 1 (1.29%) |
| Contrast Nephropathy | 4 (5.1%) |
| Dialysis | 1 (1.29%) |
| Coronary Dissection | 1 (1.29%) |
| Balloon Pump | 6 (7.7%) |
| Temporary Pacemaker | 1 (1.29%) |
| Ventilation | 2 (2.5%) |
| Inotropes | 7 (9%) |
| In hospital Mortality | 4 (5.1%) |
|  (95% CI 0.12 to 10.3%) | |
**Others: PDA (n=1), Diagonal (n=1) and Ramus (n=1)
IABP (Intra-aortic balloon pump)
Table 2: Angiographic and procedural characteristics
Discussion
The study aimed to ascertain the clinical profile of STEMI cohort presenting to KFCC, a tertiary center in Jeddah Saudi Arabia and describe their outcomes.
Our patients were predominantly males 86% with females constituting only 14%. This is similar to what was reported in literature (13,14).
The patients mean age was 57.9. Diabetes mellitus, hypertension and dyslipidemia were prevalent in this cohort of STEMI patients this is similar to what was reported by Alhabib of Saudi population in the space registry (15). Early presentation of STEMI patient remains a public health concern Only 6% of patients have arrived to Emergency department in the first hour while the majority 48% sought medical advice beyond 6 hours.
Lack of awareness of the seriousness of symptoms is a major factor of the delayed presentation other factors could include lack of methods of transportation, inaccurate initial diagnosis and lack of universal healthcare system.
The mean door to balloon time was 85 minutes. Only 62% of patients had door to balloon time within 90 minutes this was an improvement for our center from 54 % during the year 2015 (16). Yet there is a huge potential for improvement through driving certain quality metrics to meet the international standards and guidelines.
There was a low percentage of patient undergoing radial approach PCI. We think this is probably due to low comfort level of operators to adopt this approach in high risk patients another reason is being a low volume center (17). Angiographic success was achieved in 97% similar to recent trends of success. Drug eluting stents was used in 87% while only 7 patients received baremetal stents this was due to large culprit vessel and high bleeding risk. In hospital mortality was 5.1% comparable to international rates which showed in hospital mortality of 5.2% in second national registry of myocardial infarction (NRM-12) and 3% in ASSENT 4trial (18,19).
Four patients died out of 77 (two due to cardiogenic shock, one due ventricular septal rupture and one due stent thrombosis complicating spiral dissection). Our study albeit small yet it revealed major lessons These includes, poor public awareness of the importance of early presentation when suffering from chest pain, small number of patients undergoing PPCI. Low percentage of patient achieving door to balloon time less than 90 minutes. On the other hand, we have demonstrated an excellent safety and in hospital outcomes of PPCI When done in a timely fashion. KFCC performs on average 38 STEMI per year and according to a report based on the National Registry of Myocardial Infarction (NRMI) database, Magid et al. (20) reported that mortality at discharge of patients treated with primary PCI was 6.2% at hospitals performing a low volume of PCI (<16 cases per year), 4.5 % at intermediate-volume hospitals (17-48 cases per year), and 3.4 % at high-volume hospitals (>49 cases per year).
Limitations
Retrospective, observational and small number of patients is a clear limitation, yet this is a real-world data from a tertiary center that performs PPCI 24/7 reflecting the daily clinical practice. Another limitation is the study design of reporting only in hospital outcomes due to loss of follow up of many patients. Availability of long term follow up would have added to the significance of this single center study.
Conclusion
Despite being an intermediate volume center our data showed a comparable safety profile of PPCI to international data. Efforts to enhance public awareness and improve availability and access to PPCI should be adopted in Saudi Arabia.
Financial Disclosures
None of the authors have any declared conflicts of interest.
Acknowledgements
We would like to thank the quality department and the catheterization laboratory team for their help and special thanks to Mrs. Ymn yassir catheterization laboratory manager and Mrs. Intisar Abdallah and medical records department for extending their great help
REFERENCES
- De Luca G, Suryapranata H, Marino P. Reperfusion strategies in acute Elevation myocardial infarction: An overview of current status. Prog Cardiovasc Dis 2008;50:352-82.
- Andersen HR, Rasmussen K, Thuesen L, et al. A comparison of coronary angioplasty with fibrinolytic therapy in acute myocardial infarction. N Engl J Med 2003;349:733-42.
- Boersma E. Does time matter? A pooled analysis of randomized clinical trials comparing primary percutaneous coronary intervention and in-hos. Eur Heart J 2006;27:779-88.
- Keeley EC, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: A quantitative review of 23 randomized trials. Lancet 2003;361:13-20.
- Khattab AA, Abdel-Wahab M, Rother C, et al. Multi-vessel stenting during primary percutaneous coronary intervention for acute myocardial infarction. A single-center experience. Clin Res Cardiol 2008;97:32-8.
- Boden WE, Eagle K, Granger CB. Reperfusion strategies in acute ST-segment elevation myocardial infarction: A comprehensive review of contemporary management options. J Am Coll Cardiol 2007;50:917-29.
- Xavier D, Pais P, Devereaux PJ, et al. Treatment and outcomes of acute coronary syndromes in India (CREATE): A prospective analysis of registry data. Lancet 2008;371:1435-42.
- Timmer JR, Ottervanger JP, De Boer MJ, et al. Primary percutaneous coronary intervention compared with fibrinolysis for myocardial infarction in diabetes mellitus: results from the primary coronary angioplasty vs. thrombolysis-2 trial. Arch Intern Med 2007;167:1353-9.
- O’Gara. ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction A Report of the American College of Cardiology Foundation American Heart Association Task Force on Practice Guideline. JACC 2013;61(4):e78-140.
- Cannon CP. Evolving management of ST-segment elevation myocardial infarction: An update on recent data. Am J Cardiol 2006;98:10Q-21Q.
- Shehab A, Al-Habib K, Hersi A, et al. Quality of care in primary percutaneous coronary intervention for acute ST-segment -elevation myocardial infarction: Gulf RACE 2 experience. Ann Saudi Med 2014;34(6):482-7.
- Dubey G. Primary percutaneous coronary intervention for acute ST elevation myocardial infarction: Outcomes and determinants of outcomes: A tertiary care center study from North India, Indian Heart J 2016.
- Xavier D, Pais P, Devereaux PJ, et al. Treatment and outcomes of acute coronary syndromes in India (CREATE): A prospective analysis of registry data. Lancet 2008;371:1435-42.
- Sadowski M, Gasior M, Gierlotka M, et al. Gender-related differences in mortality after ST-segment elevation myocardial infarction: A large multicentre National Registry. EuroIntervention 2011;6:1068-72.
- Alhabib KF. Baseline characteristics, management practices, and in-hospital outcomes of patients with acute coronary syndromes: Results of the Saudi project for assessment of coronary events (SPACE) registry. Journal of the Saudi Heart Association 2011;23(4):233-9.
- Al-Bugami S, Al-Rahimi J, Al-Malki A, et al. ST-segment elevation myocardial infarction: Door to balloon time improvement project. Cardiol Res 2016;7(4):152-6.
- Fanaroff AC, Zakroysky P, Dai D, et al. Outcomes of PCI in relation to procedural characteristics and operator volumes in the United States. JAAC 201:2913-24.
- Tiefenbrum AJ, Handra NC, French WJ, et al. Clinical experience with primary percutaneous transluminal coronary angioplasty compared with alteplase (recombinant tissue-type plasminogen activatory) in patients with acute myocardial infarction: a report from the Second National Registry of Myocardial Infarction (NRMI-2). J Am oll Cardiol 1998;31:1240-5.
- Assessment of the Safety and Efficacy of a New Treatment Strategy with Percutaneous Coronary Intervention (ASSENT-4 PCI) investigators. Primary Versus tettecteplase-facilitated percutaneous coronary intervention in patients with ST-segment elevation acute myocardial infarction (ASSENT-4 PCI): randomized trial. Lancet 2006;367:569-78.
- Magid DJ, Calonge BN, Rumsfeld JS, et al. National Registry of Myocardial Infarction 2 and 3 Investigators. Relation between hospital primary angioplasty volume and mortality for patients with acute MI treated with primary angioplasty vs. thrombolytic therapy. JAMA 2000;284:3131-8.