Perfluorocarbons in photodynamic and photothermal therapy
Received: 26-Oct-2017 Accepted Date: Nov 22, 2017; Published: 30-Nov-2017
Citation: Scheer A, Kirsch M, Ferenz KB. Perfluorocarbons in photodynamic and photothermal therapy J Nanosci Nanomed. November-2017;1(1):21-27.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Photodynamic therapy (PDT) and photothermal therapy (PTT) belong to the category of phototherapy and are based on the photophysical generation of either noxious reactive oxygen species, thereby inducing oxidative stress, or rather cell-hostile environmental conditions (local hyperthermia) with the general aim to destroy abnormal tissues. A great advantage of both strategies is the fact that they are minimally invasive by low toxicity for the surrounding healthy tissue. In both cases, photosensitizers and light are inevitable. Furthermore, in PDT oxygen is a mandatory component for generating reactive oxygen species such as singlet oxygen. Perfluorocarbons (PFCs) can donate molecular oxygen tension in the target tissue of interest (tumor tissue) thereby improving PDT outcome in such a hypoxic region. Because applied PFCs can at the same monitored via both, ultrasonic and magnetic resonance imaging techniques, they increase the selectivity of PDT and PTT to target tissue while sparing healthy cells in the surroundings. This selectivity is especially important in tissues such as eye, brain or gastro-intestinal tract. During the last few years a lot of interesting approaches (clinical and preclinical) were developed to improve PDT and PTT with the aid of PFCs. This review informs the astute reader about actual approaches on the use of PFCs in PDT and PTT, respectively. The literature indicates that the use of PFCs can increase the efficiency of PDT and PTT thereby contributing to a more effective therapy of tumors and other diseases.
Keywords
Perfluorocarbons, photothermal therapy, photodynamic therapy, perfluorohexane, perfluoropropane, perfluorodecalin, perfluoro octylbromide
Introduction
Photodynamic therapy
Photodynamic therapy (PDT) is a kind of treatment by using photosensitizers, light, and oxygen to locally generate reactive oxygen species as scalpel. PDT has gained importance in the curative treatment of pre-cancer and superficial tumors therapy [1]. Furthermore, the PDT is firmly established in various disorders of dermatology and has importance in other medical disciplines [2]. The growing prominence of PDT is underlined by a comparison with conventional chemotherapy and irradiation therapies. Their effects depend on the cell division rate and challenge also the healthy cells and the body's immune system to a great extent. In contrast, the therapeutic efficacy of PDT is based on the ability of photosensitizers (i) to absorb light energy and (ii) to transfer it to oxygen molecules thereby forming singlet oxygen and other noxious reactive oxygen species derived from it [3]. The antitumor effect of PDT is due to a direct cytotoxic effect on tumor cells, damage to the tumor vasculature and induction of a robust inflammatory response that can lead to the development of systemic immunity [4]. The extent of this effect depends on the type and dose of photosensitizer used, time between administration and exposure to light, dose of light, the quantum yield of the photosensitizer as well as tumor oxygen concentration. Because of its highly localized effect, treatment against metastatic lesions is ineffective [4]. Ongoing research is focused on finding optimal PDT conditions to induce systemic immunity which might, at least to some extent, obviate this limitation of missing target-oriented therapy of metastasis in the future. An ideal photosensitizer should have a prominent resonance between 600 and 800 nm, since the absorption of photons with wavelengths greater than 800 nm does not provide enough energy to excite oxygen to its singlet state [4]. Particularly photosensitizers from the class of hematoporphyrins and its derivatives are used so far in the therapeutic area [5]. Mainly hematoporphyrin derivatives (HpD) such as Photosan 3®, Photofrin II® and δ-aminolevulinic acid (5-ALA), a precursor of protoporphyrin IX, were recently investigated for their response rates [3,6,7]. ALA-PDT induced morphological changes and leads to changes in the expression of 112 proteins, of those up to 30% involved in the epigenetic regulation [8]. HpD belong to the "first generation" of photosensitizers. Because of their persistent noxious side-effects less harmful second generation photosensitizers like chlorines or purpurines are presently preferred [3]. Blue light penetrates the tissue least efficiently compared to red light and infrared radiation. The range between 600 and 1200 nm is often referred to as the optical window of tissue [9]. No light source is ideal for all PDT indications, even with the same photosensitizer. The choice of light source should therefore be based on photosensitizer absorption, disease, cost and size of the target tissue [4]. In general PDT is strongly oxygen-dependent. The activated oxygen species are converted into "type I" reaction products e.g. hydroxyl and superoxide radicals, and the non-radical "type II" reaction product singlet oxygen (1O2) [10-12]. In a type II photooxidative reaction, the energy is transferred to oxygen molecules, generating reactive oxygen species (ROS), primarily 1O2 [13]. 1O2 reacts with lipids and proteins of the cellular membranes, resulting in degradation of the plasma membrane and damage to various organelles such as mitochondria, endoplasmic reticulum and lysosomes. As secondary effects, thrombosis and narrowing of blood vessels, edema and the recruitment of immune cells can be observed [14,15]. While the radicals of type I reactions are generated by electron transfer processes 1O2 is formed by energy transfer [3]. A photosensitizer transfers its energy to triplet oxygen (3O2) thereby generating 1O2 following equations eqn. (1) and (2). As the energy (hʋ) needed for this process corresponds to about 94 kJ/mol near-infrared light is ideally suited to induce the reaction described in eqn. (1) [10,11]. The stability of the triplet state (3photosensitizer) is longer compared to the singlet state of the same molecule (1photosensitizer). Because of this physical fact quenching of the 3photosensitizer state by 3O2 is most efficient [11].
eqn. (1): 1photosensitizer + hʋ → 3photosensitizer
eqn. (2): 3photosensitizer + 3O2 → 1photosensitizer + 1O2
From eqn. (1) and (2) it can be concluded that 1O2 is the virtually active species in phase 1 and 2 of PDT. The PDT can be divided into three phases. The photooxidation reaction in the first phase results in a dynamic, reversible depletion of ambient oxygen proportional to the fluorescence decay rate. In the second phase, the oxygen-induced pathological changes lead to the occlusion of blood vessels and hypoxia. If only a low light dose was applied this hypoxic phase would also be reversible. The third phase is characterized by the cumulative effects of phases 1 and 2. These lead to irreversible vascular collapse, irreversible oxygen depletion and tissue/ tumor necrosis [3]. The particular electronic configuration of oxygen principally permits quenching of singlet and triplet states of photosensitizers and such quenching reaction does not require additional energy; furthermore, oxygen diffusion is very rapid in most biological media [10]. However, as the life-time of 1O2 within a cell is very short, 1O2 molecules diffuse only over short distances [11]. It is therefore important to originate 1O2 molecules selectively in the vicinity of target cells/ cell organelles and this is where combination of PDT with imaging methods such as ultrasonic and magnetic resonance imaging comes into place (see below). PDT leads to the three most important cell death pathways, apoptosis, necrosis and autophagy-associated cell death [16]. Apoptosis is an important type of cell death. Following photodynamic damage, the mitochondrial outer membrane (MOMP) permeability is controlled by the Bcl-2 family and is largely independent of p53 [17]. Mitochondria-associated photosensitizers induce a permissive signal for the MOMP as a result of the light damage of membrane-bound Bcl-2 [18-20] and subsequently lead to a release of caspase activators. These include cytochrome c and smac / DIABLO as well as pro-apoptotic molecules and apoptosis-induced molecules (AIF) [17]. Anyhow, PDT is not perfectly efficient today. The limited penetration of light into tissue and the bottle-neck like dependence on oxygen open possibilities to further optimize the therapeutic efficacy of PDT. One approach is to improve the oxygen supply of target tissue during the PDT accomplished by perfluorocarbons.
Photothermal therapy
Photothermal therapy (PTT) also uses light-absorbing molecules to selectively damage cells or tissues. Due to its high specificity, minimal invasiveness and precise spatial-temporal selectivity, PTT has unique advantages in the treatment of cancer for destruction and removal of malignant tumors [21,22]. Another benefit of PTT is that it can be applied just with multimodal imaging or in addition to currently used therapies [23-25]. PTT is capable of killing cancer cells in the primary tumor or in local metastases in the early stage of metastasis, inhibiting cell migration and invasive activities, and also killing cancer cells in more distant metastases (if trackable) [26,27]. The compounds used can be either chromophores occurring naturally in the tissue or externally applied dyes. An example is indocyanine green (ICG). The electrons are raised to an excited state by the absorption of the laser light. If these excited electrons fall back, the kinetic energy of surrounding water molecules will be increased. Because of this effect, there is an overheating of the direct environment of the light-absorbing substance and this can be used for a local cell or tissue destruction without causing systemic effects. Depending on the temperature reached in the target tissue PTT just causes minor destructive local hyperthermia (42-46°C) or even photothermal ablation (>43°C for 240 min or >54°C for 1 s) leading to irreversible necrosis of the tissue [28]. Because the conversion of NIR into thermal energy is generally non-specific, exact targeting of e.g. tumor tissue and a reasonable choice of photothermal compound and irradiation time are very important to prevent healthy surrounding tissue from irreversible damage [28]. The choice of photothermally active compounds is dependent (i) on their absorption capacity and (ii) on their efficiency in the conversion rate of light to heat [29]. These characteristics help to reduce the amount of laser energy required to damage either tumor cells or tissue and thus reduce side-effects. Regarding laser radiation parameters, typical power densities 10-106 W/cm2 and exposition time 1 μs-1 min are used [30]. To further improve tissue targeting, photothermally active compounds are encapsulated into nanoparticles (e.g. hollow gold nanospheres) designed to specifically reach the tissue of concern and thus ensuring enrichment of PTT compounds only in abnormal tissue [28]. In regard to PDT PTT does not depend on oxygen. In fact, in the context of PTT perfluorocarbons are used to enhance the identification of malign tissue via ultrasound (US) imaging to further protect healthy tissue from damage. This supports selective targeting of e.g. tumor tissue while reducing unwanted sideeffects and allows for longer irradiation times, thus improving the efficacy of PTT. For more general information about PTT, see Zou, 2016 [31].
Perfluorocarbons
Perfluorocarbons are pure synthetic carbon compounds which are completely fluorinated (or substituted by other halogens, e.g. bromine). The large number of fluorine atoms causes weak intermolecular interactions with strong intramolecular bonds. The carbon backbone is stabilized by the strong carbon-fluorine bonds and the electron-attracting effects of the fluorine atoms [32]. Fluorine is the element in the periodic system with the highest electronegativity, resulting in a much denser electron packing and larger electron cloud compared to hydrogen. This electron density leads to a shielding of the carbon-carbon bond and thus to the pronounced chemical, biological and physical stability. Because of this, PFCs are neither lipophilic nor hydrophilic and are chemically as well as metabolically inert [33]. Due to the weak intermolecular interactions, PFCs have a high solubility for respiratory gases such as O2 or CO2 [34]. According to Henry's law, the solubility is proportional to the respective gas partial pressure and is therefore independent of other factors such as the pH or the temperature [32,35,36]. Because of their high oxygen solubility (40-56 ml O2 per 100 ml PFC at 760 torr and 25°C) [37], the lack of metabolism as well as the germ-free and unlimited production, PFCs represent an attractive substance class for use in medicine and research. Medically used PFCs can be exhaled due to their vapor pressure if not applied externally from the beginning. For PFCs to be administered intravenously, they must be emulsified or encapsulated beforehand. Some of the perfluorocarbons described herein are or were already approved for clinical use, either in the context of artificial oxygen carriers, ultrasonic contrast agents or for intravitreal use [38,39]. For instance, the artificial oxygen carrier Perftoran® (perfluorodecalin) is clinically available in Russia (artificial oxygen carrier).
Current applications of PFCs in PDT and PTT
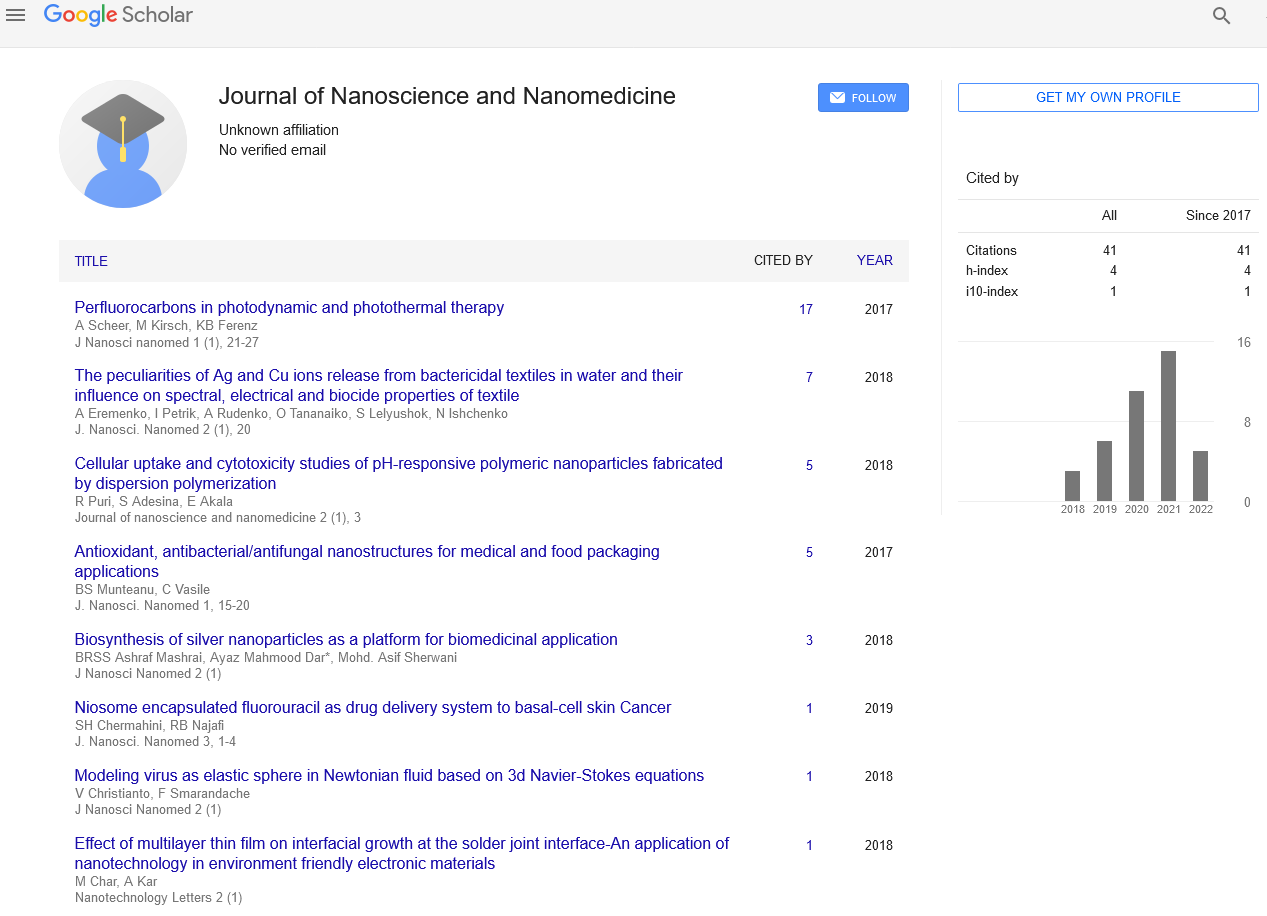
This section presents PFCs currently used in (pre-)clinical research approaches, the data are summarized in Table 1.
| Perfluorocarbon | Chemical Formula | Status | Delivery System | Combined Photosensitizer/ Combined Drug | Reference |
|---|---|---|---|---|---|
| Perfluorooctyl bromide | C8BrF17 | Preclinical | Double Nanoemulsion | ICG/ DOX, PEI | [43] |
| Preclinial | Double-Nanoemulsion (Nanocapsules) | GO, Gd-DTPA | [53] | ||
| Preclinical | Nanocapsules | Gold Nanoshell, | [46] | ||
| Preclinical | Nano-/Microcapsules | Pyrrole | [83] | ||
| Perfluorohexane | C6F14 | Preclinical | Nanocapsules | Fe3O4 | [64] |
| preclinical | Nanodroplet | IR780 | [63] | ||
| Perfluoropentane | C5F12 | Preclinical | Nanocubes | HPB | [84] |
| Preclinical | Double emulsion | ICG | [85] | ||
| Perfluorodecalin | C10F18 | Preclinical | Liquid | Hypericin | [70] |
| Perfluorotributylamine | C12F27N | Preclinical | Nanoparticles | ICG | [80] |
| Perfluoropropane | C3F8 | Clinical | Gas | Verteporfin/Alteplase, Ranibizumab | [82] |
| Clinical | Gas | Verteporfin | [81] |
Table 1: Different perfluorocarbons currently used in preclinical and clinical PDT and PTT research approaches
• Perfluoro octylbromide
In the treatment of breast cancer, chemotherapy with a variety of different drugs e.g. doxorubicin (DOX) is well established [40]. However, the clinical use of DOX is severely restricted due to its significant side effects caused by the high dose rate necessary to reach therapeutic effects [40,41]. To circumvent the mentioned drawbacks and to improve bioavailability, stability and safety, a combination of nanomedicine + chemotherapy + specific targeting to the tumor cells (e.g. realized by specific antibodies attached to the drug carrier molecule) persuaded many researchers [42]. However, the therapeutic success is still not satisfying. To further improve the susceptibility of target tissue, chemotherapy should be combined with photodynamic therapy (PDT) as proposed by Lee and colleagues [43]. Because photosensitizers necessary for PDT such as ICG are highly sensitive to (i) degradation in aqueous environment [44] and (ii) plasma clearance [45], the group of Lee combined nanomedicine with specific targeting and noninvasive infrared (NIR)-based phototherapy by producing a type of anti-HER2 ICG-DOXloaded polyethyleneimine (PEI)-coated PFC double nanoemulsion (HIDPPDNEs) [43]. As described above, perfluoro octylbromide (PFOB) was added to the preparation to increase the generation of singlet oxygen species in the target tissue, thus to boost the effect of PDT. Lee et al. demonstrated that HIDPPDNEs generated 10-fold more singlet oxygen than free ICG in equal concentration; whereupon preoxygenation of HIDPPDNEs did not further increase the concentration of singlet oxygen [43]. Unfortunately, it was not investigated yet, if this finally affects the survival rate of HER2- overexpressing breast cancer cells as expected.
Besides PDT, also the concept of PTT is a promising alternative to conventional forms of cancer therapy [46-49]. Many nanomaterials with strong NIR absorption were already tested [47,50]. US imaging and magnetic resonance imaging (MRI) are supportingly used for effective PTT [51,52]. Li et al. fabricated nanocapsules by loading PFOB into polylactic acid (PLA) nanocapsules (NCs) followed by surface functionalization with graphene oxide (GO) and gadolinium-chelate (Gd- DTPA) (PFOB@PLA/GO/Gd-DTPA) [53]. This multifunctional material combined US imaging with MRI capabilities for use in PTT. Graphene oxide has shown high efficacy for photothermal ablation of cancer [54]. Liquid PFOB provided US contrast enhancement, Gd-DTPA served as MRI contrast agent and GO coating for a favorable NIR-absorbing property. Significant cell death could be detected with PFOB@PLA/GO/Gd-DTPA NCs in cells treated with NIR laser irradiation for 10 min. The combination of PFOB@PLA/GO/Gd-DTPA NCs and NIR was therefore capable of killing tumor cells. Furthermore, the PFOB@PLA/GO/Gd-DTPA NCs showed excellent contrast enhancement for US imaging as well as for MRI and therefore unite a great potential for cancer diagnosis [53].
To increase the effectiveness of PTT, an exact localization and size of the tumor is necessary. Compared to Li et al., the group of Ke et al. combined US imaging and computed tomography (CT) with PTT for better diagnostics [46]. The already frequently used gold nanostructures show strong absorption in the NIR and are also an ideal agent for CT imaging. PFOB was used to enhance US contrast while the gold nanoshell served as CT contrast agent and PTT photoabsorber. The so constructed pegylated gold nanoshell PFOB nanocapsules (PGsP NCs) could be easily heated from a temperature of 37°C to a temperature of above 42°C, a temperature where tumor cells are killed [55]. PGsP NCs reduced the cell viability to about 10% cell viability at a concentration of 0.1 mg mL-1 capsules. In vivo studies showed a successful systemic circulation of the PGsP NCs with accumulation in the liver and kidneys. The local temperature rapidly increased up to 60°C with the irradiation of NIR laser and the tumor growth was inhibited by 96.7% compared to the control group [46].
In PTT polypyrrole (PPy) materials are often used because of their stability, biocompatibility and high conductivity [56-58]. Furthermore, in vivo studies indicated that low concentrations of PPy show low long-term cytotoxicity [59]. Because PPy is insoluble in organic solvent [60,61], the complicated fabrication process and poor dispersity hindered further applications. Synthesis of PPy nanoparticles with high photohermal conversion efficiency is one option. Zha et al. carried out a facile preparation of water-dispersible PPy via an oil-in-water emulsion by generating PPy nanocapsules and microcapsules with a liquid PFOB core (PPyPFOBNCs/PPyPFOBMCs) [62]. The combination of PPy with its favorable NIR-absorbing property and PFOB with its established US imaging capability led to a multifunctional photothermal agent for realtime US imaging guided PTT treatment. PPyPFOBMCs alone, laser alone or the negative control without laser but with PPyPFOBMCs did not lead to any change in cell viability and density. On the other hand, cells treated with PPyPFOBMCs and laser showed increased cell death. The effect could be magnified applying prolonged laser exposure. The cytotoxicity of PPyPFOBMCs was dose-dependent and irradiation time-dependent. By a concentration of 10 μg mL-1 only 20% of cells remained viable. An in vivo study showed that the distribution of PPyPFOBMCs could be easily monitored via a real-time mode and that tumor volume could be affected after treatment with PPyPFOBMCs and laser light.
• Perfluorohexane
A low oxygen concentration affects the performance and efficiency of PDT in killing cancer cells during hypoxia. The group of Tang et al. established a method to increase the 1O2 yield of photosensitizers [63]. To investigate if this technique can eliminate cancer cells, the NIR photosensitizer IR780 was combined with a perfluorohexane (PFH) core resulting in nanodroplets (LIP (IR780 + PFH)). The generated 1O2 was released into the tumor matrix and at the same time O2 was recovered in the PFH phase [63]. The results showed an increased efficacy of LIP (IR780 + PFH) compared to LIP (IR780) alone. Most informatively, LIP (IR780 + PFH) in 1% O2 generated more 1O2 than LIP (IR780) in 21% O2. It could be demonstrated that PFH increases the efficiency of PDT dose-dependently. The size of tumors treated with LIP (IR780 + PFH) + NIR was significantly inhibited [63].
Temperature-sensitive and NIR photo-absorption polymeric nanocapsules (perfluorohexane (PFH)@PLGA/Fe3O4) were designed by the group of Zhao [64]. The nanocapsules could not only be used to increase the local tumor temperature by absorbing NIR energy, but were also capable of enhancing tumor therapy via a phase-shift thermoelastic expansion effect [64]. The temperature-sensitive nanocapsules could be converted from liquid into gas by high temperatures and / or infrared radiation. When using infrared irradiation, the Fe3O4 incorporated in the capsule shell absorbed the infrared light and increased the kinetic energy of the surrounding water molecule. This facilitates the evaporation of the PFH and was called NIR radiation droplet vaporization. In vitro and in vivo results showed that PFH@PLGA/Fe3O4 nanocapsules are suitable for MR imaging. The highest rate of apoptosis were obtained in an experimental setting of a temperature between 50.3 ± 0.28°C to 59.24 ± 0.71°C at an irradiation distance of 15 cm. PFH@PLGA/Fe3O4 nanocapsule groups showed a significantly higher apoptosis rate than control groups [64].
• Perfluoropentane
The intrinsic instability and potential toxicity of various photothermal conversion agents, e.g. Prussian Blue [PB], limited further clinical translations. In addition, hollow mesoporous PB (HPB) NPs were already synthesized [48]. However, a loading of the HPB NPs with phase-change materials was not carried out. Therefore, HPB NPs loaded with perfluoropentane (PFP) (HPB-PFP) were designed to enhance contrast in US imaging and thus improving efficiency of PTT in cancer therapy. Administration of HPB did not mediate in any significant harmful effects after 24 and 48 hours of incubation. In contrast, the HPB-PFP NPs showed an efficient laser-light absorption that leads to heating and efficient killing of cancer cells. The liquid to gas phase-change of PFP, induced by the conversion of the NIR light energy to heat mediated by HPB, led to the intended photoactivated US imaging effect of HPB-PFP. HPB-PFP NPs showed an excellent in vivo photothermal transformation performance and could inhibit tumor growth significantly [49].
The therapy of Rheumatoid arthritis (RA) is currently limited to the exploitation of proapoptotic effects, which however, limited efficiency and are non-targeted. Likewise, attempts were made to improve the effects of RA treatments by minimizing the local hypoxia. In the last few years PDT was proposed as a new strategy to treat RA. Since PDT therapy is hampered due to the limited light penetration, again, a combination of US and PDT was investigated by Tang et al. The photosensitizer ICG can be activated by both, light and US. However, as already mentioned above, ICG is unstable, has high protein binding and can lead to photobleaching [44,45,65]. Again, nanotechnology was used to overcome these difficulties. Various studies showed that ICG-charged poly(lactide coglycolide) (PLGA) nanoparticles increase the stability of ICG and display an effective transport system [66-69]. The group of Tang Q et al. now investigated the combination of a PLGA nanosystem with PFP and ICG (OI-NPs) [63]. They demonstrated that intracellular fluorescence signals in cells incubated with OI-NPs are much stronger than compared to control (free ICG). Quantitative results showed a 16-fold greater fluorescence intensity in the OI-NPs group than in the free ICG group. This underlines that the encapsulation of ICG in PLGA could increase the cellular uptake of ICG [63]. Furthermore, an augmented generation of reactive oxygen species due to the presence of PFP could be detected when applying OI-NPs. Those effects probably are responsible for the higher rate of cell apoptosis under treatment with OI-NPs compared to control [63].
• Perfluorodecalin
The treatment of superficial bladder tumors is based mainly on endoscopic resection combined with chemo-or immunotherapy by intravesical instillation [70]. Bacillus Calmette Guerin (BCG) is often used in therapy to prevent progression and to ensure survival. However, the resistance to BCG of different bladder tumors leads to therapeutic problems [71,72]. Previous studies demonstrated that transitional cell carcinoma (TCC) of the bladder can efficiently be treated by PDT [73-75]. Interestingly hypericin, a clinical diagnostic tool for the detection of tumors [76,77], was established for treating bladder tumors photodynamically. Previous work of the group of Kamuhabwa and co-workers suggests that although TCC tumor cells take up hypericin in a sufficient concentration tumors are not destroyed after PDT [70]. Most likely the phototoxicity of hypericin seems to be oxygen-dependent and therefore should be mediated via the production of singlet oxygen [78]. Because of this conclusion, the group used perfluorodecalin (PFD) as an oxygen carrier to enhance the hypericin-mediated efficacy of PDT. It was demonstrated that the spheroid cells in the absence of PFD did not adequately respond to hypericin-PDT. However, the increased oxygenation with PFD led to a dramatic improvement in hypericin-PDT-dependent cell killing [70]. Furthermore, the number of apoptotic cells in the presence of both, hypericin-PDT and PFD, could be significantly increased compared to hypericin-PDT alone [70]. The results suggest that only the combination leads to an efficient and selective photodynamic treatment.
• Perfluorotributylamine
The efficacy of PDT and PTT is generally still limited because of rapid degradation of photosensitizers such as ICG, even when packed in nanoparticles to increase half-life. In order to prevent the rapid degradation of such ICG-containing nanoparticles by the reticuloendothelial system (RES), the group of Ren developed a novel oxygen self-enriched biomimetic red blood cell (RBC). For this purpose, albumin nanoparticles containing ICG and the PFC perfluorotributylamine (PFTBA) with RBC membranes were produced (IPH@RBC) [60]. Previous studies with PFD showed an increased 1O2 production [1,79]. The designed IPH@RBC successfully enhanced PTT and PDT in vitro as the clearance of IPH@RBC by macrophages was reduced. This resulted in a prolonged intravascular circulation time in vivo (mice) and thus a high accumulation in the tumor tissue [80].However, it is questionable whether this approach ever will be transferred to clinics: In contrast to what is affirmed by Ren and collegues, PFTBA is NOT FDA-approved because of its inacceptable organ retention time (e.g. 2.5 years in rat) [32]. Ironically, the authors cited precisely this review article of Jean G. Riess to proof FDA-approval [80].
• Perfluoropropane
PDT with verteporfin, which is a popular and successful therapy for patients with polypoidal choroidal vasculopathy (PCV) to regain visual acuity, was an ineffective procedure to the subgroup of patients presenting with PCV in combination with extensive submacular hemorrhage. This is due the fact, that the applied laser light is not able to penetrate through the massive blood clot and thus does not reach the residual active polypoidal lesions located underneath the clot. Only the preceding replacement of the clot by intravitreally injected optically inert perfluoropropane provided access to the promising PDT for patients suffering from PCV+ massive hemorrhage. In contrast to all other approaches described in this review the special optical properties (instead of gas-dissolving qualities) of the perfluorocarbon were exploited. Additionally, Chan et al. demonstrated that in previously non-treatable (at least with PDT) subgroups perfluoropropane injection followed by standard PDT was as effective as in patients without or with only marginal submacular hemorrhage and PCV [81].
The positive study results of patients with PCV [81] were confirmed and extended to patients with neovascular age-related macular degeneration by Papavasileiou and collegues [82]. Importantly, both studies involved patients rather than animals or cultured cells.
Conclusion
PDT is dependent to the action of a photosensitizer, light and oxygen in order to remove cancer cells or modulate cell cycle. More precisely, in PDT, the intermediacy of 1O2 is the limiting factor to effectively destroy cells. Because of this, so far hypoxic tumor domains were inaccessible by this therapy. The same applies to situations, where the light is not able to reach the target cells, e.g. light absorbing clots of blood in patients with massive submacular hemorrhage. In both cases PFCs are of great help; either because of their excellent oxygen-dissolving properties or because of their optical inertness.
Furthermore, PDT and PTT are most effective when selectively applied to target cells. Because of their brilliant US and MRI contrast enhancement features, PFCs allow perfectly for selective targeting thus rendering PDT and PTT more effective.
The discussed research approaches do in fact combine different wellestablished methods such as oxygen delivery by PFCs, US and MRI imaging, nanomedicine and PDT/ PTT to a new and most effective research strategy. This was only possible because the strong potential of perfluorocarbons was recognized and transferred to the context of PDT and PTT.
Conflict of Interest
The authors declare no conflict of interest. This research did not receive any specific grant from funding agencies in the public, commercial or notfor- profit sector.
REFERENCES
- Cheng Y, Cheng H, Jiang C, et al. Perfluorocarbon nanoparticles enhance reactive oxygen levels and tumour growth inhibition in photodynamic therapy. Nature communications 2015;6:8785.
- Lui H, Anderson RR. Photodynamic therapy in dermatology. Shedding a different light on skin disease. Arch Dermatol. 1992;128:1631–6.
- Fuchs J, Thiele J. The role of oxygen in cutaneous photodynamic therapy. Free Radic Biol Med. 1998;24:835–47.
- Agostinis P, Berg K, Cengel KA, et al. Golab J. Photodynamic therapy of cancer: An update. CA Cancer J Clin. 2011;61:250-81.
- Dougherty TJ, Grindey GB, Fiel R, et al. Photoradiation therapy. II. Cure of animal tumors with hematoporphyrin and light. J Natl Cancer Inst. 1975;55:115-21.
- Zoepf T, Jakobs R, Arnold JC, et al. Palliation of nonresectable bile duct cancer: Improved survival after photodynamic therapy. Am J Gastroenterol. 2005;100:2426–30.
- Berg K, Selbo PK, Weyergang A, et al. Porphyrin-related photosensitizers for cancer imaging and therapeutic applications. J Microsc. 2005;218:133-47.
- Demyanenko SV, Uzdensky AB, Sharifulina SA, et al. PDT-induced epigenetic changes in the mouse cerebral cortex: A protein microarray study. Biochim Biophys Acta. 2014;1840:262-70.
- Juzeniene A, Nielsen KP, Moan J. Biophysical aspects of photodynamic therapy. J Environ Pathol Toxicol Oncol. 2006;25:7–28.
- Schmidt R. Photosensitized generation of singlet oxygen. Photochem Photobiol. 2006;82:1161-77.
- Clo E, Snyder JW, Ogilby PR, et al. Control and selectivity of photosensitized singlet oxygen production: Challenges in complex biological systems. Chembiochem. 2007;8:475-81.
- Filatov MA, Karuthedath S, Polestshuk PM, et al. Generation of Triplet Excited States via Photoinduced Electron Transfer in meso-anthra-BODIPY: Fluorogenic Response toward Singlet Oxygen in Solution and in Vitro. J Am Chem Soc. 2017;139:6282-5.
- Foote CS. Mechanisms of photosensitized oxidation. There are several different types of photosensitized oxidation which may be important in biological systems. Science 1968;162:963-70.
- Babilas P, Landthaler M, Szeimies R-M. Photodynamic therapy in dermatology. Eur J Dermatol. 2006;16:340-8.
- Colussi VC, Feyes DK, Mukhtar H. Perspectives of photodynamic therapy for skin diseases. Skin Pharmacol Appl Skin Physiol. 1998;11:336-46.
- Zou Z, Chang H, Li H, et al. Induction of reactive oxygen species: An emerging approach for cancer therapy. Apoptosis 2017;22:1321-35.
- Buytaert E, Dewaele M, Agostinis P. Molecular effectors of multiple cell death pathways initiated by photodynamic therapy. Biochim Biophys Acta. 2007;1776:86-107.
- Kessel D, Castelli M. Evidence that bcl-2 is the target of three photosensitizers that induce a rapid apoptotic response. Photochem Photobiol. 2001;74:318-22.
- Xue LY, Chiu SM, Oleinick NL. Photochemical destruction of the Bcl-2 oncoprotein during photodynamic therapy with the phthalocyanine photosensitizer Pc 4. Oncogene 2001;20:3420-7.
- Usuda J, Chiu S-m, Murphy ES, et al. Domain-dependent photodamage to Bcl-2. A membrane anchorage region is needed to form the target of phthalocyanine photosensitization. J Biol Chem. 2003;278:2021-9.
- Alkilany AM, Thompson LB, Boulos SP, et al. Gold nanorods: Their potential for photothermal therapeutics and drug delivery, tempered by the complexity of their biological interactions. Adv Drug Deliv Rev. 2012;64:190-9.
- Shanmugam V, Selvakumar S, Yeh C-S. Near-infrared light-responsive nanomaterials in cancer therapeutics. Chem Soc Rev. 2014;43:6254-87.
- Chen Q, Wang C, Zhan Z, et al. Near-infrared dye bound albumin with separated imaging and therapy wavelength channels for imaging-guided photothermal therapy. Biomaterials 2014;35:8206-14.
- Su S, Ding Y, Li Y, et al. Integration of photothermal therapy and synergistic chemotherapy by a porphyrin self-assembled micelle confers chemosensitivity in triple-negative breast cancer. Biomaterials 2016;80169-78.
- Wang Y, Yang T, Ke H, et al. Smart Albumin-Biomineralized Nanocomposites for Multimodal Imaging and Photothermal Tumor Ablation. Advanced materials 2015;27:3874-82.
- Wang C, Xu L, Liang C, et al. Immunological responses triggered by photothermal therapy with carbon nanotubes in combination with anti-CTLA-4 therapy to inhibit cancer metastasis. Advanced materials (Deerfield Beach, Fla.) 2014;26:8154-62.
- Chen Q, Liang C, Wang C, et al. An imagable and photothermal "Abraxane-like" nanodrug for combination cancer therapy to treat subcutaneous and metastatic breast tumors. Advanced materials 2015;27:903-10.
- Melancon MP, Zhou M, Li C. Cancer theranostics with near-infrared light-activatable multimodal nanoparticles. Acc Chem Res. 2011;44:947-56.
- Huang YF, Sefah K, Chang HT, et al. Selective photothermal therapy for mixed cancer cells using aptamer-conjugated nanorods. Langmuir 2008;24:11860-5.
- Jelínková H. Introduction: The history of lasers in medicine. In: Lasers for Medical Applications: Woodhead Publishing Series in Electronic and Optical Materials: Woodhead Publishing; 2013:1-13.
- Zou L, Wang H, He B, et al. Current Approaches of Photothermal Therapy in Treating Cancer Metastasis with Nanotherapeutics. Theranostics 2016;6:762-72.
- Riess JG. Oxygen carriers ("blood substitutes")--raison d'etre, chemistry, and some physiology. Chem Rev. 2001;101:2797-920.
- Krafft MP. Fluorocarbons and fluorinated amphiphiles in drug delivery and biomedical research. Adv Drug Deliv Rev. 2001;47:209-28.
- Riess JG. Perfluorocarbon-based oxygen delivery. Artif Cells Blood Substit Immobil Biotechnol. 2006;34:567-80.
- Dinkelmann S, Northoff H. Artificial Oxygen Carriers – a Critical Analysis. Infus Ther Transfus Med. 2002;29167-74.
- Sloviter HA, Petkovic M, Ogoshi S, et al. Dispersed fluorochemicals as substitutes for erythrocytes in intact animals. J Appl Physiol. 1969;27:666-8.
- Wilhelm E, Battino R. Thermodynamic functions of the solubilities of gases in liquids at 25.deg. Chemical reviews 1973;73:1-9.
- Zhou Y, Wang Z, Chen Y, et al. Microbubbles from gas-generating perfluorohexane nanoemulsions for targeted temperature-sensitive ultrasonography and synergistic HIFU ablation of tumors. Advanced materials 2013;25:4123-30.
- Wang X, Chen H, Chen Y, et al. Perfluorohexane-encapsulated mesoporous silica nanocapsules as enhancement agents for highly efficient high intensity focused ultrasound (HIFU). Advanced materials 2012;24:785-91.
- Tacar O, Sriamornsak P, Dass CR. Doxorubicin: an update on anticancer molecular action, toxicity and novel drug delivery systems. The Journal of pharmacy and pharmacology 2013;65:157-70.
- Chatterjee K, Zhang J, Honbo N, et al. Doxorubicin cardiomyopathy. Cardiology 2010;115:155-62.
- Hossain MK, Cho HY, Kim KJ, et al. In situ monitoring of doxorubicin release from biohybrid nanoparticles modified with antibody and cell-penetrating peptides in breast cancer cells using surface-enhanced Raman spectroscopy. Biosensors & bioelectronics 2015;71300-5.
- Lee YH, Ma YT. Synthesis, characterization, and biological verification of anti-HER2 indocyanine green-doxorubicin-loaded polyethyleneimine-coated perfluorocarbon double nanoemulsions for targeted photochemotherapy of breast cancer cells. Journal of nanobiotechnology 2017;15:41.
- Saxena V, Sadoqi M, Shao J. Degradation kinetics of indocyanine green in aqueous solution. Journal of pharmaceutical sciences 2003;92:2090-7.
- Desmettre T, Devoisselle JM, Mordon S. Fluorescence properties and metabolic features of indocyanine green (ICG) as related to angiography. Survey of ophthalmology 2000;45:15-27.
- Ke H, Yue X, Wang J, et al. Gold nanoshelled liquid perfluorocarbon nanocapsules for combined dual modal ultrasound/CT imaging and photothermal therapy of cancer. Small 2014;10:1220-7.
- Tian Q, Tang M, Sun Y, et al. Hydrophilic flower-like CuS superstructures as an efficient 980 nm laser-driven photothermal agent for ablation of cancer cells. Advanced materials 2011;23:3542-7.
- Rai P, Mallidi S, Zheng X, et al. Development and applications of photo-triggered theranostic agents. Advanced drug delivery reviews 2010;62:1094-124.
- O'Neal DP, Hirsch LR, Halas NJ, et al. Photo-thermal tumor ablation in mice using near infrared-absorbing nanoparticles. Cancer letters 2004;209:171-6.
- Liu X, Tao H, Yang K, et al. Optimization of surface chemistry on single-walled carbon nanotubes for in vivo photothermal ablation of tumors. Biomaterials 2011;32:144-51.
- Goldberg SN, Grassi CJ, Cardella JF, et al. Image-guided tumor ablation: standardization of terminology and reporting criteria. Journal of vascular and interventional radiology: JVIR. 2005;16:765-78.
- Huber PE, Jenne JW, Rastert R, et al. A new noninvasive approach in breast cancer therapy using magnetic resonance imaging-guided focused ultrasound surgery. Cancer research 2001;61:8441-7.
- Li Z, Ke H, Wang J, et al. Graphene Oxide and Gadolinium-Chelate Functionalized Poly(lactic acid) Nanocapsules Encapsulating Perfluorooctylbromide for Ultrasound/Magnetic Resonance Bimodal Imaging Guided Photothermal Ablation of Cancer. Journal of nanoscience and nanotechnology 2016;16:2201-9.
- Jin Y, Wang J, Ke H, et al. Graphene oxide modified PLA microcapsules containing gold nanoparticles for ultrasonic/CT bimodal imaging guided photothermal tumor therapy. Biomaterials 2013;34:4794-802.
- Hahn GM, Braun J, Har-Kedar I. Thermochemotherapy: synergism between hyperthermia (42-43 degrees) and adriamycin (of bleomycin) in mammalian cell inactivation. Proceedings of the National Academy of Sciences of the United States of America 1975;72:937-40.
- Jang J, Yoon H. Multigram-scale fabrication of monodisperse conducting polymer and magnetic carbon nanoparticles. Small 2005;1:1195-9.
- Hong J-Y, Yoon H, Jang J. Kinetic study of the formation of polypyrrole nanoparticles in water-soluble polymer/metal cation systems: A light-scattering analysis. Small 2010;6:679-86.
- Oh W-K, Yoon H, Jang J. Size control of magnetic carbon nanoparticles for drug delivery. Biomaterials 2010;31:1342-8.
- Ramanaviciene A, Kausaite A, Tautkus S, et al. Biocompatibility of polypyrrole particles: An in-vivo study in mice. The Journal of pharmacy and pharmacology. 2007;59:311-5.
- Carson JL. Blood transfusion and risk of infection: new convincing evidence. Jama 2014;311:1293-4.
- Jang KS, Ko HC, Moon B, et al. Observation of photoluminescence in polypyrrole micelles. Synthetic Metals 2005;150:127-31.
- Zha Z, Yue X, Ren Q, et al. Uniform polypyrrole nanoparticles with high photothermal conversion efficiency for photothermal ablation of cancer cells. Advanced materials 2013;25:777-82.
- Tang X, Cheng Y, Huang S, et al. Overcome the limitation of hypoxia against photodynamic therapy to treat cancer cells by using perfluorocarbon nanodroplet for photosensitizer delivery. Biochemical and biophysical research communications 2017;487:483-7.
- Zhao Y, Song W, Wang D, et al. Phase-Shifted PFH@PLGA/Fe3O4 Nanocapsules for MRI/US Imaging and Photothermal Therapy with near-Infrared Irradiation. ACS applied materials & interfaces 2015;7:14231-42.
- Yoneya S, Saito T, Komatsu Y, et al. Binding properties of indocyanine green in human blood. Investigative ophthalmology & visual science 1998;39:1286-90.
- Zheng C, Zheng M, Gong P, et al. Indocyanine green-loaded biodegradable tumor targeting nanoprobes for in vitro and in vivo imaging. Biomaterials 2012;33:5603-9.
- Xu RX, Huang J, Xu JS, et al. Fabrication of indocyanine green encapsulated biodegradable microbubbles for structural and functional imaging of cancer. Journal of biomedical optics 2009;14:34020.
- Saxena V, Sadoqi M, Shao J. Polymeric nanoparticulate delivery system for Indocyanine green: biodistribution in healthy mice. International journal of pharmaceutics 2006;308:200-4.
- Manchanda R, Nagesetti A, McGoron AJ, et al. Preparation and characterization of a polymeric (PLGA) nanoparticulate drug delivery system with simultaneous incorporation of chemotherapeutic and thermo-optical agents. Colloids and surfaces B, Biointerfaces 2010;75:260-7.
- Kamuhabwa AR, Huygens A, Roskams T, et al. Enhancing the photodynamic effect of hypericin in human bladder transitional cell carcinoma spheroids by the use of the oxygen carrier, perfluorodecalin. International journal of oncology 2006;28:775-80.
- Herr HW, Pinsky CM, Sogani PC, et al. Long-term effect of intravesical bacillus Calmette-Guerin on flat carcinoma in situ of the bladder. J Urol. 1986;135:265-7.
- Prout GR JR, Griffin PP, Daly JJ. The outcome of conservative treatment of carcinoma in situ of the bladder. J Urol. 1987;138:766-70.
- D'Hallewin MA, Baert L, Marijnissen JP, et al. Whole bladder wall photodynamic therapy with in situ light dosimetry for carcinoma in situ of the bladder. J Urol. 1992;148:1152-5.
- Kriegmair M, Waidelich R, Lumper W, et al. Integral photodynamic treatment of refractory superficial bladder cancer. J Urol. 1995;154:1339-41.
- Nseyo UO, DeHaven J, Dougherty TJ, et al. Photodynamic therapy (PDT) in the treatment of patients with resistant superficial bladder cancer: A long-term experience. J Clin Laser Med Surg. 1998;16:61-8.
- D'Hallewin MA, Witte PA de, Waelkens E, et al. Fluorescence detection of flat bladder carcinoma in situ after intravesical instillation of hypericin. J Urol. 2000;164:349-51.
- D'Hallewin M-A, Kamuhabwa AR, Roskams T, et al. Hypericin-based fluorescence diagnosis of bladder carcinoma. BJU Int. 2002;89:760-3.
- Thomas C, Pardini RS. Oxygen dependence of hypericin-induced phototoxicity to EMT6 mouse mammary carcinoma cells. Photochem Photobiol. 1992;55:831-7.
- Ren H, Liu J, Su F, et al. Relighting Photosensitizers by Synergistic Integration of Albumin and Perfluorocarbon for Enhanced Photodynamic Therapy. ACS applied materials & interfaces 2017;9:3463-73.
- Ren H, Liu J, Li Y, et al. Oxygen self-enriched nanoparticles functionalized with erythrocyte membranes for long circulation and enhanced phototherapy. Acta Biomater. 2017;59269-82.
- Chan WM, Liu DT, Lai TY, et al. Extensive submacular haemorrhage in polypoidal choroidal vasculopathy managed by sequential gas displacement and photodynamic therapy: a pilot study of one-year follow up. Clinical & experimental ophthalmology 2005;33:611-8.
- Papavasileiou E, Steel DH, Liazos E, et al. Intravitreal tissue plasminogen activator, perfluoropropane (C3F8), and ranibizumab or photodynamic therapy for submacular hemorrhage secondary to wet age-related macular degeneration. Retina 2013;33:846-53.
- Zha Z, Wang J, Zhang S, et al. Engineering of perfluorooctylbromide polypyrrole nano/microcapsules for simultaneous contrast enhanced ultrasound imaging and photothermal treatment of cancer. Biomaterials 2014;35:287-93.
- Jia X, Cai X, Chen Y, et al. Perfluoropentane-encapsulated hollow mesoporous prussian blue nanocubes for activated ultrasound imaging and photothermal therapy of cancer. ACS applied materials & interfaces 2015;7:4579-88.
- Tang Q, Cui J, Tian Z, et al. Oxygen and indocyanine green loaded phase-transition nanoparticle-mediated photo-sonodynamic cytotoxic effects on rheumatoid arthritis fibroblast-like synoviocytes. International journal of nanomedicine 2017;12381-93.