Psychotic symptoms associated with superior vena cava syndrome consecutive to methamphetamine abuse
Marion Dubois, Department of Psychiatry, La Conception Hospital, Public Assistance-Marseille Hospitals, 13005 Marseille, France, Tel: +33491435102, Email: marion.dubois@ap-hm.fr
Received: 13-Oct-2017 Accepted Date: Oct 25, 2017; Published: 05-Feb-2018
Citation: Dircks S, Dubois M, Dassa D. Psychotic symptoms associated with superior vena cava syndrome consecutive to methamphetamine abuse. J Clin Psychiatry Neurosci. February-2018;1(1):5-6.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Use of Amphetamines is becoming increasingly frequent, inducing a wide range of complications, among which comes severe vascular conditions and psychiatric episodes.
Here we present the case of a 24 year old man admitted for psychotic symptoms whose physical examination revealed a Superior Vena Cava Syndrome.
Chest (CT)-scan showed up severe thrombosis and stenosis of superior vena cava. Malignancies, coagulation disorders, auto-immune diseases were ruled out. Thrombus could not be removed despite several radiological intervention attempts. Psychosis was treated successfully with atypical anti-psychotic (Clozapine). When reviewing history, the patient reports an intense crystal Methamphetamine abuse in the past. We retained Methamphetamine as the most relevant etiology for both psychosis and thrombosis. This unexpected association between Methamphetamine, psychotic symptoms and vascular condition raises the question of a tendency to abnormal vascular and inflammatory processes in schizophrenia.
This case aims at enjoining practitioners to be cautious and proposing systematic radiological exams in psychotic patients with a Methamphetamine abuse history.
Keywords
Methamphetamine; Schizophrenia; Superior vena cava syndrome; Thrombosis; Vascular diseases
Introduction
Superior Vena Cava Syndrome (SVCS) is a manifestation arising from compression or obstruction of Superior Vena Cava (SVC), characterized by edema of face, neck, trunk, upper extremities as well as collateral venous distension of neck and anterior chest wall [1].
Mostly caused by mediastinal malignancies, SVCS can be secondary to SVC thrombosis with a prevalence of 1-5% [2].
Amphetamine-type stimulants can cause systemic effects [3] including vascular conditions, psychotic and manic episodes [4].
Here, we describe a previously unrecognized association between psychosis and SVCS in a patient with history of Methamphetamine abuse.
Case Report
A 24 year old man presented acute agitation, aggressive behavior. He showed self-neglect, delusional speech, auditory and cenesthetic hallucinations, inappropriate uncontrolled laughter, perseveration and misrecognition.
Physical examination: face and neck edema and voluminous collateral blood-flow network of the anterior chest wall veins, consistent with SVCS.
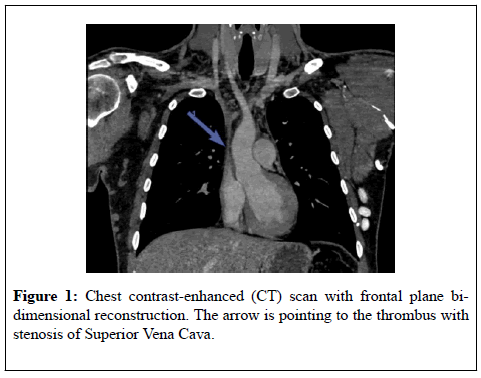
Chest CT-scan (Figure 1) revealed SVC thrombosis with distended collateral vasculature and stenosis of SVC. Intramuscular Heparin (Tinzaparine: 14000 UI/d) was delivered to prevent further complications.
Coagulation tests were normal, thrombophilia screening negative.
No evidence for cryoglobulinemia, antiphospholipid syndrome neither ANCA-vasculitis.
Myeloproliferative neoplasm, celiac, Biermer and Behçet diseases were ruled out.
Paraneoplastic etiology was rejected: Thoracic CT-scan and full body PETscan found no evidence of neoplasia.
Brain CT and electroencephalography were normal. Brain SPECT showed mild frontal cortex and anterior cingulum hypo-perfusion.
Schizophrenia was diagnosed according to Mini-DSM [5]. PANSS total score was 133.
The patient received first Risperidone 6 mg/d without success. Olanzapine 20 mg/d was stopped because of weight gain and Aripiprazole 15 mg/d discontinued after Akathisia.
Eventually, symptoms resolved with Clozapine 350 mg/d facilitating history-taking: acute rheumatic fever at 11. First drug abuse at 18: occasional cannabis and cocaine abuse. At 22, high doses of sniffed crystal Methamphetamine (ice), over 10 days.
He remembers clearly the sudden swelling of upper limbs, face, neck and trunk the day after and persistent ever since.
Despite several radiological interventions, thrombus was unremovable. Tinzaparine was relayed by oral anticoagulant: Rivaroxaban.
Discussion
To our knowledge this is the first case of schizophrenia with deep venous thrombosis, prior to psychotropic medication and without coagulation disorders.
But Amphetamines can induce both psychotic symptoms [5] and venous thrombosis (cerebral [6] or renal [7]).
Here, Methamphetamine was taken in crystal form, supposed to be particularly harmful because of its high potency compared to other forms [8].
The sudden swelling in the patient’s reports highlights the chronological relationship between ice-Methamphetamine and thrombosis. In point of fact, SVCS occurs more abruptly in thrombotic cases than compressive ones, often resulting in medical emergencies [9].
Amongst many complications, Amphetamines have a direct vascular toxicity their neurotoxic effects appear to be due to induction of inflammatory genes in small vessel endothelial cells [10].
In 2005 Hanson and Gottesman [11] proposed that some psychosis resulted of damage to the micro-vascular system in the brain, initiated by genetically influenced abnormal inflammatory processes, in response to environmental factors. Inflamed micro-vessels lose their coupling with astrocytes, leading to disregulated cerebral blood flow, and damaged Blood-Brain Barrier (BBB).
In 2015, Turowski and Kenny [12] suggested that the direct action of Methamphetamine on vascular endothelium induces acute opening of BBB while striatal effects and resultant neuro-inflammatory signaling could lead to its chronic dysfunction.
This case raises the question of a tendency to abnormal inflammatory processes in schizophrenia. The risk of serious vascular complications should be emphasized and prevention developed. Systematic radiological exams (contrast enhanced CT scans f.i) could be prescribed in psychotic patients with Methamphetamine abuse history, to detect thrombosis that normally goes unnoticed.
Conflict of Interest
None declared.
REFERENCES
- Straka C, Ying J, Kong FM, et al. Review of Evolving Etiologies, Implications and Treatment Strategies for the Superior Vena Cava Syndrome. Springer Plus. 2016;5(1).
- Rice TW, Rodriguez RM, Light RW. The Superior Vena Cava Syndrome: Clinical Characteristics and Evolving Etiology. Medicine. 2006;85(1):37-42.
- Lineberry TW, Bostwick JM. Methamphetamine Abuse: A Perfect Storm of Complications. Mayo Clinic Proceedings. 2006;81(1):77-84.
- Hermens DF, Lubman DI, Ward PB, et al. Amphetamine psychosis: A Model for Studying the Onset and Course of Psychosis. Med J Aust. 2009;190(4):22-5.
- Bramness JG, Gundersen OH, Guterstam J, et al. Amphetamine-induced Psychosis- A Separate Diagnostic Entity or Primary Psychosis Triggered in the Vulnerable. BMC Psychiatry. 2012;12(1).
- Rothwell PM, Grant R. Cerebral Venous Sinus Thrombosis Induced by “Ecstasy”. Journal of Neurology, Neurosurgery and Psychiatry. 1993;56(9):1035.
- Eldehni MT, Roberts ISD, Naik R, et al. Case Report of Ecstasy-Induced Renal Venous Thrombosis. Clinical Kidney Journal. 2010;3(5):459-60.
- Lappin JM, Roxburgh A, Kaye S, et al. Increased Prevalence of Self-Reported Psychotic Illness Predicted by Crystal Methamphetamine Use: Evidence from a High-Risk Population. International Journal of Drug Policy. 2016;38:16-20.
- Cohen R, Mena D, Carbajal-Mendoza R, et al. Superior Vena Cava Syndrome: A Medical Emergency. The International Journal of Angiology : Official Publication of the International College of Angiology, Inc. 2008;17(1):43-6.
- Lee YW, Hennig B, Yao J, et al. Methamphetamine Induces AP-1 and NF-B Binding and Transactivation in Human Brain Endothelial Cells. Journal of Neuroscience Research. 2001;66(4):583-91.
- Hanson DR, Gottesman II. Theories of Schizophrenia: A Genetic-Inflammatory-Vascular Synthesis. BMC Medical Genetics. 2005;6(1).
- Turowski P, Kenny BA. The Blood-Brain Barrier and Methamphetamine: Open Sesame. Frontiers in Neuroscience. 2015;9.