Rhabdomyosarcoma of the testis, epididymis and spermatic cord: A review and update
Received: 27-Sep-2018 Accepted Date: Dec 26, 2018; Published: 28-Dec-2018
Citation: Venyo AKG. Rhabdomyosarcoma of the testis, epididymis and spermatic cord: A review and update. Pulsus J Surg Res. 2018;2(2):78-86.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Rhabdomyosarcoma of the testis, epididymis, spermatic cord and rhabdomyosarcomas that are classified as para-testicular rhabdomyosarcomas tend to be rare and sporadically reported; hence many clinicians may not be familiar with the biological behaviour and management of the disease.
Aim: To review the literature on rhabdomyosarcoma of the testis, epididymis, spermatic cord including all tumours that are referred to as para-testicular rhabdomyosarcoma. Method: Various internet data bases were searched.
Results/Review: Rhabdomyosarcomas tend to represent primitive malignant round cell tumours that have skeletal muscle differentiation determined by immunohistochemistry and ultrastructural studies. Rhabdomyosarcomas of the testis, epididymis, spermatic cord and the para-testicular region are rare and they tend to represent about 7% of all rhabdomyosarcomas and about 6% of all para-testicular tumours. One out of about 20 million males in one year tends to develop these types of tumours. No preference for race or side has been established. These tumours tend to spread via the lymphatic system to iliac lymph nodes; nevertheless, spread via the blood stream to the liver and lungs do occur. These tumours most commonly tend to present as painless lump or mass within the testis/para-testicular region and the history tends to be short of few days to weeks duration. Occasionally patients may present with pain, fever, vomiting, and abdominal distension as well. On examination there tends to be a palpable lump related to the testis or epididymis, spermatic cord or para-testicular region and the lump could be inguinoscrotal. One third to half of these tumours may be associated with metastases. Diagnosis of a tumour within the testis, epididymis, spermatic cord or para-testicular region tends to be suspected on clinical examination, radiology imaging and this tends to be confirmed by means of histopathology examination an immunohistochemistry studies. Routine haematology and biochemistry test results tend to be normal and serum ß-HCG, AFP, and LDH tend to be normal. In some cases associated with liver metastases the liver function test results could be abnormal. Children and adults could develop the tumour. Ultrasound scan would tend to show a mass in the testis or para-testicular region with increased vascularity or mass compressing the testis. MRI scan could show a heterogeneously enhancing mass within the testis or a mass in the para-testicular region compressing the testis. CT TAP or MRI TAP could be utilized to stage the tumour. Treatment options tend to include surgical excision and chemotherapy; radiotherapy for local disease control could be offered; retroperitoneal lymph node dissection tends to be undertaken when there is radiology imaging evidence of lymph node enlargement. Gross examination of the specimen tends to show encapsulated, lobulated, smooth, grey-whitish tumour and these may have foci of haemorrhage, necrosis or cystic degeneration. Microscopic examination may show rhabdomyoblasts and undifferentiated primitive cells, tadpole cells, spindle cells and variable mitotic activity. Immunohistochemistry studies may show positive staining for Desmin, myoglobin, myosin, MSA, MyoD1, Myogenin, and rarely they may express cytokeratin. The outcome following treatment for localized disease tends to be better than when there are metastases. Poor prognosis tends to be related to age especially when he patients are aged less than one year or equal to or more than 10 years. Prognosis also tends to be affected by the classification of the tumour based upon the Intergroup Rhabdomyosarcoma Study Group’s International Classification of Rhabdomyosarcoma.
Conclusion: Rhabdomyosarcoma of the testis, epididymis, spermatic cord including all tumours classified as para-testicular rhabdomyosarcoma are rare tumours with aggressive potential that tend to present with a short history; these tumours tend to be associated with normal tumour makers; diagnosis tends to be confirmed by the histopathology features and typical immunohistochemistry features (some of which include (positive staining for myogenin, desmin, actin, vimentin, and others as stated in the paper); treatment tends to be by means of surgical excision and chemotherapy; prognosis tends to be worse for advanced metastatic disease and in patients who are less than 1 year-old or equal to or greater than 10 years old as well as upon the classification of the tumour.
Keywords
Rhabdomyosarcoma; testis; epididymis; spermatic cord; paratesticular; desmin; myogenin; actin; chemotherapy; surgical excision; orchidectomy
Introduction
Rhabdomyosarcoma of the testis, epididymis, and spermatic cord are rare malignant tumors that tend to be encountered sporadically globally. In view of the rarity of rhabdomyosarcoma of the testis and para-testicular region, it would be envisaged that many clinicians would not be familiar with the disease and they could possibly not be familiar with the biological behavior as well as the management of the disease. The ensuing review article on rhabdomyosarcoma of the testis, epididymis, and spermatic cord is divided into two parts: (A) Overview, and (B) Miscellaneous narrations and discussions from reported cases, case series and studies on rhabdomyosarcoma of the testis and para-testicular region.
Results
Overview
Definition/general comment: Rhabdomyosarcoma is a terminology which had been coined for a primitive malignant round cell tumor which has skeletal muscle differentiation evidenced by its immunohistochemistry features and by its characteristic ultrastructure.
Epidemiology: The epidemiology of rhabdomyosarcoma of the testis, and epididymis, as well as the spermatic cord, have been summated as follows:
• Rhabdomyosarcoma of the testis, epididymis and spermatic cord tends to be quite rare, and this tends to represent 7% of all the rhabdomyosarcomas, as well as it tends to represent 6% of all para-testicular tumors. It still tends to be the commonest non-germinal malignant tumor within the para-testicular area
• The incidence of rhabdomyosarcoma of the testis/epididymis/ spermatic cord tends to approximate 1 per 20 million males in one year
• Para-testicular area tends to be commonest for the development of rhabdomyosarcoma in among teenagers
• There has not been any documentation of preference of a tumor for any particular side (left or right side) or for any particular race
• Within the region of the testis, epididymis and spermatic cord, embryonal rhabdomyosarcoma which includes is variant the spindle cell type of rhabdomyosarcoma tends to be the commonest sub-type of rhabdomyosarcoma, although, any sub-type of rhabdomyosarcoma can develop within the area:
• Rhabdomyosarcoma of the testis/epididymis/spermatic cord tends to occur within all age groups; nevertheless, it tends to be most commonly encountered in children
• About Eighty percent (80%) of rhabdomyosarcomas of the testis/ epididymis/spermatic cord tend to occur prior to the age of 21 years; About twenty percent (20%) of rhabdomyosarcomas of the testis/epididymis/spermatic cord tend to be equally distributed among the older age groups [1]
• Alveolar rhabdomyosarcoma and orphic rhabdomyosarcoma of the testis/epididymis/spermatic cord, tend to be less common, and pleomorphic rhabdomyosarcoma of the testis/epididymis/spermatic cord tends to be the least common [1]:
• Alveolar rhabdomyosarcoma of the testis/epididymis/spermatic cord tends to occur mainly in young adults and among adolescent men [1]
• Pleomorphic rhabdomyosarcoma of testis/epididymis/spermatic cord tends to develop mainly in adults
Sites: Generally, the majority of rhabdomyosarcomas of the testis/ epididymis/spermatic cord tend to be centered within the para-testicular soft tissue and there tends to be variability with regards to testicular involvement by a tumor.
Pathophysiology: It has been stated that rhabdomyosarcoma of the testis/ epididymis/spermatic cord tends to generally spread via the lymphatic system into the iliac lymph nodes; nevertheless, spread by means of the haematogenous route into the lungs and liver also does occur.
Clinical manifestations: Rhabdomyosarcomas of the testis/epididymis/ spermatic cord tend to diagnosed pursuant to the ensuing presentations:
• The commonest presentation tends to be a history of painless swelling within the scrotum which tends to be of a short duration of a few days or weeks
• History of pain in the testicular area or scrotum as well as trauma to the testicular area or scrotum tends to be a very rare manifestation which tends to be the presentation in about 7% of each of the two presentations (history of pain in 7%, history of testicular/scrotal trauma in 7%) of cases
• Clinical examination tends to reveal a large tumor which quite often tends to reach the inguinal-scrotal region
• Investigations tend to show that in one third (1/3) to half (1/”) of cases of rhabdomyosarcoma of testis/epididymis/spermatic cord, the presence of metastasis at the presentation of the disease:
• Ferrari et al., [1] reported that out of 216 patients who had rhabdomyosarcomas of the testis/epididymis/spermatic cord, 18 patients did present with distant metastases
• It had been iterated that adults tend to have a higher prevalence of metastases at the time of initial presentation of rhabdomyosarcoma of the testis/epididymis/spermatic cord [2-4]
Diagnosis: It is not straightforward to clinically establish a diagnosis of rhabdomyosarcoma of the testis, epididymis, spermatic cord or anywhere within the scrotum. Nevertheless, the first thing a clinician does is to determine whether a mass within a scrotum is a pure scrotal swelling or an inguinoscrotal swelling and if clinically the clinician can clearly palpate a cord separately and clearly above the mass then the clinician becomes satisfied that the mass is purely a scrotal mass. Having decided that the mass is purely a scrotal mass the next thing a clinician does is to palpate to find out if the mass is related to the testis and if the mass in the testis is confined to the testis alone. The clinician also palpates to feel the epididymis from the head down to the tail of the epididymis to see if the epididymis feels normal or abnormal including whether the head, body, and tail feel normal in size, shape and consistency and whether or not the mass is related to the epididymis alone or not involving the epididymis. The clinician also palpates the cord for its consistency and to see if there is a mass related to the cord and if the mass related to the cord is solid, or cystic and if the mass is attached also to the epididymis and or testis. Quite often the scrotal lump or mass may be so large that the clinician cannot feel the testis and the epididymis separately because the mass has encompassed these structures. The clinician also decides whether the lesion contains a hydrocele fluid by undertaking a trans-illumination test. A cystic lesion does trans-illuminate but a solid mass does not transilluminate. A tumor within the testis with secondary hydrocele may give a clinical feeling of a mass within the testis associated with the signs of fluid. By clinical examination quite of the clinician can provisionally say a palpable intra-scrotal is confined to the testis, epididymis, or the cord but other times the clinician may not feel so confident in saying if the mass is precisely confined to the testis or the para-testicular tissue. When a clinician suspects testicular tumor laboratory tests including serum Beta Human Chorionic Gonadotrophin, Alpha fetoprotein, and lactate dehydrogenase levels are elevated but these also would usually be normal. A through general and systematic examination are generally undertaken and noting all clinical findings including whether or not the inguinal lymph nodes are enlarged. Having formed an impression of a mass related to the testis, epididymis, spermatic cord, the clinician would then request an ultrasound urgent scan of the scrotal content. If the ultrasound scan shows a testicular tumour this would make the surgeon decide upon undertaking trans-inguinal radical orchidectomy. If the ultrasound scan does show a tumour not related to the testis but to the epididymis of the spermatic cord the features of the lesion and its involvement or noninvolvement would be carefully studied and discussed with regards to the option of treatment of curative intent including: Radical orchidectomy, excision of the spermatic cord lesion alone or excision of the epididymis and the epididymal tumour for histology examination. Without histology tissue diagnosis treatment initially is usually undertaken for a testicular tumour, a spermatic cord tumour, a tumour of the epididymis, or a paratesticular tumour and after surgical excision of the tumour a definitive diagnosis is made and definite management options are discussed by the multi-disciplinary team discussion. In summary:
• Diagnosis of a tumor within the testis, epididymis, and spermatic cord area or the para-testicular tends to suspected based upon the presentation of a mass within the testis/para-testicular region as well as based upon the clinical examination finding of a mass in the testicular and para-testicular region
• Radiology investigation especially ultra-sound scan finding of a mass within the testis/para-testicular region with features suggestive of a tumor. Staging of a tumor would be undertaken by doing Computed Tomography (CT) scan of thorax abdomen and pelvis or Magnetic Resonance Imaging (MRI) scan of thorax abdomen and pelvis to plan the full management and post-operative follow up of the patient
• Histopathology examination of the excised specimen of a tumor tends to be the confirmatory way to diagnose rhabdomyosarcoma of the testis/epididymis/spermatic cord which tends to exhibit microscopy and immunohistochemistry features of rhabdomyosarcoma
Laboratory investigations
Microbiology investigations: Urine analysis, urine microscopy and culture tend to be undertaken in cases of rhabdomyosarcoma of the paratesticular and testis as part of the general assessment of patients with rhabdomyosarcoma of the testis/para-testicular region but the results would not be diagnostic of the disease but there is evidence of urinary tract infection then the infection tends to be treated appropriately.
Hematology investigations: Full blood count, and coagulation screen tend to be undertaken as part of the general assessment of all patients but the results would tend not to be diagnostic of the disease; nevertheless, if there is any impairment of the hematology profile then this would b treated accordingly.
Biochemistry investigations: Serum urea and electrolytes, serum glucose and liver function tests would tend to be normal in many cases but when there are extensive metastases to the liver, then there may be impairment of the liver function. If a patient is diabetic then the serum glucose results would enable clinicians to about the level of control of the blood sugar.
Serum Beta Human chorionic gonadotrophin, serum alpha fetoprotein, and lactic dehydrogenase levels tend to be assessed as part of the general workup of testicular or scrotal masses and the results would tend to be within the normal range.
Radiology investigations: Ultrasound scan of testes, scrotal contents, inguinal region, abdomen, and pelvis.
• Ultrasound scan of the scrotal contents and the inguinal region could show in cases of a para-testicular tumor, a heterogenous abnormal soft tissue mass within the para-testicular region either displacing or encasing the testis. The extent of the soft-tissue mass could be defined by the ultrasound scan as to its upper limit within or near the inguinal canal as well as if there are any enlarged lymph nodes in the inguinal region it would show it
• In cases of a tumor that is confined to the testis, ultrasound scan would show the lesion within the testis, its size and whether the lesion is confined to the testis or the lesion had extended beyond the testis as well as if there is any secondary hydrocele and furthermore ultrasound scan of abdomen and pelvis would show whether or not there are enlarged lymph nodes in the groin, abdomen, and pelvis and whether there is involvement of the liver
• If a tumor is confined to the spermatic cord, the ultrasound scan would show the lesion within the cord not affecting or affecting the epididymis or testis and whether a tumor has extended into the inguinal canal
Computed tomography (CT) scan: When a diagnosis of rhabdomyosarcoma of the testis/epididymis/spermatic cord is made following pathology examination of the radical orchidectomy specimen, epididymectomy specimen, excision of spermatic cord specimen, the multi-disciplinary team tends to recommend staging of the tumour which could take the form of CT scan of abdomen, pelvis and thorax to confirm or negate presence/absence of nodal disease or metastases
CT scan of thorax abdomen and pelvis are also undertaken during the follow-up of patients who have undergone treatment for rhabdomyosarcoma of testis, epididymis or spermatic cord to exclude or confirm metastatic disease
Magnetic resonance image (MRI) scan
• When a diagnosis of rhabdomyosarcoma of the testis/epididymis/ spermatic cord is made following pathology examination of the radical orchidectomy specimen, the multi-disciplinary team tends to recommend staging of the tumour which could take the form of MRI scan of abdomen, pelvis and thorax to confirm or negate presence/ absence of nodal disease or metastases
• MRI scan of the testes and scrotal contents would tend to show a heterogeneously enhancing well-defined soft-tissue mass which would classically tend to encase or be displacing the testis suspicious of malignancy
• Apart from staging MRI scan of thorax, abdomen and pelvis for the initial planning of treatment for patients who have rhabdomyosarcoma of the testis, epididymis, spermatic cord, or para-testicular region, MRI scan of thorax, abdomen, and pelvis can be undertaken during the regular follow-up of the patients to establish if there is any evidence of metastasis or not
Treatment: When there is confirmation of the diagnosis of rhabdomyosarcoma of the testis/epididymis/spermatic cord, the multidisciplinary team meeting tends to recommend the following:
• Surgical excision in addition to chemotherapy which tends to be VAC based as the standard of care
• There tends to be significant toxicity related to the chemotherapy but despite this majority of clinicians favor chemotherapy
• Ferrari and associates had suggested that patients who are found to have low-risk disease, should be treated by means of low-dose anthracycline-free regimens without any loss of benefit;
• Ferrari and associates [1] did report 216 patients who had pediatric para-testicular rhabdomyosarcoma that had an over-all 5-year survival of 85.5%, 95% for localized disease 2% metastatic disease
• It had been iterated that radiotherapy could be administered for local control of the disease
• It had also been advised that retroperitoneal lymph node dissection should not be undertaken unless there is radiology imaging evidence of lymph node enlargement
• Detailed approaches, as well as stratification for treatment, has been outlined by some authors [2-6]
Macroscopic features: The macroscopic features of para-testicular rhabdomyosarcoma had been summated as follows:
• A tumor tends to be encapsulated, a lobulated, smooth, greyish white, glistening mass which tends to displace the testicular parenchyma but characteristically, does tend not to invade the testicular tissue
• A tumor tends to measure between 1cm and 20 cm and tends to have foci of hemorrhage, and cystic degeneration
Microscopic features: It has been summated that microscopic examination of rhabdomyosarcoma of the testis/epididymis/spermatic cord tends to show the ensuing features:
• A mixture of rhabdomyoblasts that are arranged haphazardly as well as undifferentiated primitive cells
• Primitive cells which tend to be small and round that have minimal cytoplasm, and dark nuclei
• Strap cells, that tend to be variable with regards to numbers, and these cells tend to have or not have cross-striations and bizarre “tadpole cells”
• Spindle cell morphology tends to appear more commonly at this site
• Mitotic activity tends to be variable
Immunohistochemistry features:
Positive immunohistochemistry staining: Rhabdomyosarcoma of the testis/epididymis/spermatic cord tend to exhibit positive immunohistochemistry staining for:
• Desmin, myoglobin, myosin, MSA (which tend to be non-specific)
• MyoD1 (nuclear expression; regulatory protein in skeletal muscle nuclear differentiation)-This tends to be a confirmatory marker
• Myogenin (nuclear expression; regulatory protein in skeletal muscle differentiation)-This tends to be a confirmatory marker
• On rare occasions, a tumor may exhibit positive staining with cytokeratin
Negative immunohistochemistry staining: Rhabdomyosarcoma of the testis/epididymis/spermatic cord tends to exhibit negative immunohistochemistry staining with:
• TdT lymphoid markers
Electron microscopy features: Electron microscopy examination of rhabdomyosarcoma of the testis/epididymis/spermatic cord tends to show the ensuing features:
• Thin actin as well as thicker myosin filaments
• No evidence of neurosecretory granules
Molecular/cytogenetic features: It has been summated that molecular and cytogenetic studies of rhabdomyosarcoma of the testis/epididymis/ spermatic cord tend to show the following:
• Partial monosomy of chromosome 11, loss of heterozygosity (LOH) at 11p characterizes embryonal rhabdomyosarcoma (RMS);
• LOH by the loss of maternal copy and duplication of paternal copy of 11p tends to result in activation of IGF2 (IGF2 has been known to show genomic imprinting, with silencing of the maternal allele)
• Alveolar rhabdomyosarcoma (RMS) tends to be characterized by t(2;13)(q35;q14) or t(1;13)(q36,q14); which results in PAX3-FKHR or the PAX7-FKHR fusion proteins, detectable in 75% to 80% of alveolar rhabdomyosarcomas but these tend to be absent in other subtypes of rhabdomyosarcomas
• Some cases of alveolar rhabdomyosarcomas tend to have loss of imprinting of the IGF2 gene with re-expression of the normally silent maternal allele
Differential diagnoses: The differential diagnoses of rhabdomyosarcoma of the testis/epididymis/spermatic cord have been stated to include the ensuing:
• Other small round tumors;
• Extraosseous PNET/Ewing tumors
• Lymphoblastic lymphoma
• Leiomyosarcoma;
• Smooth muscle tumors of the para-testicular region need to be differentiated from rhabdomyosarcoma of the testicular region and this would be achieved by pathology findings of smooth muscle tumor features in the tissue rather than skeletal muscle tissue features
Factors for prognostication: Some of the factors of prognostication ensuing treatment for or encountering rhabdomyosarcoma of include:
• Poor or inferior prognosis tends to be related to:
• The age of the patient of greater than/equal to 10 years or less than 1 year (≥10 years or <1 year)
• The site of origin of a tumor, para-meningeal, urinary bladder, prostate, abdomen, trunk, extremities, tend to be associated with inferior prognosis; orbital, para-testicular, and vaginal locations tend to be associated with better outcome
• Tumour size with the largest diameter of greater than 5 cm (>5 cm).
• Locally invasive tumor (a T2 tumor)
• Incomplete resection of a tumor
• Presence of distant metastases at the time of the initial diagnosis of a tumor
• The number of metastatic sites or tissues involved
• Presence of regional lymph node involvement (N1)
• The histopathology sub-type of a tumor; pleomorphic rhabdomyosarcoma tends to have a worse outcome in comparison with the alveolar type, and worse than the embryonal sub-type. Prognostic factors and clinical outcomes in children and adolescents with a metastatic rhabdomyosarcoma-a report from the Intergroup Rhabdomyosarcoma Study IV [7]
Intergroup Rhabdomyosarcoma Study Group’s International Classification of Rhabdomyosarcomas and related sarcomas. Pathologic aspects and proposal for a new classification-an Intergroup Rhabdomyosarcoma Study [8].
• Group 1 which tends to be associated with the better outcome; this group of tumors includes botryoid and spindle cell variety of tumors
• Group II tends to be associated with intermediate prognosis; the tumors in this group are constituted by embryonal NOS
• Group III, tumors tend to be associated with worse prognosis and this group of tumors and constituted by the alveolar sub-type of tumors
• Group IV tumors have been stated to be associated with unclear. It has been stated that this Group is constituted by the following: Rhabdomyosarcomas with rhabdoid features, embryonal rhabdomyosarcomas that have anaplastic features, and sclerosing rhabdomyosarcomas
Miscellaneous narrations and discussions from some reported cases/series/studies
Para-testicular rhabdomyosarcoma: Ferrari et al. [1] reported the experience of the German-Italian Cooperative Group with 216 patients that had para-testicular rhabdomyosarcoma which had been treated over 20 years. Ferrari et al. [1] did report that at the time of diagnosis of the tumors, 198 patients did have localized disease and 18 patients did have distant metastases. Ferrari et al., [1] stated the following:
• Out of the patients who had the non-metastatic disease, complete resection of a tumour had been undertaken in 83% of cases
• Evaluation of the retroperitoneal lymph nodes had changed over the years from routine surgical staging to radiology assessment
• All patients had been treated by means of chemotherapy, which had been reduced in intensity and duration for patients who had low-risk features in subsequent protocols
• Radiotherapy had been had been administered to 10% of the patients
Ferrari et al. [1] summated the results as follows:
• Out of 72 patients who had negative retroperitoneal computed tomography (CT) scan, surgical assessment detected nodal involvement in only one case
• Out of 23 patients who had enlarged nodes on CT scans, surgery had confirmed nodal spread in 65% of these patients
• They did not observe any differences with regards to the rate of nodal involvement over the years
• With a median follow-up of 110 months, the 5-year survival was 85.5% for the series of patients as a whole, 94.6% for patients who had localized disease, and 22.2% for patients who had metastatic disease. Retroperitoneal lymph node recurrence had been the major cause of treatment failure. Univariate analysis did reveal the prognostic value of tumor invasiveness, size of a tumor, ability to completely resect a tumor (resectability of a tumor), as well as of lymph node involvement and age, in patients with the localized tumor
Ferrari et al., [1] made the ensuing conclusions:
• The prognosis of patients who have localized para-testicular rhabdomyosarcoma is excellent, despite the reduction in chemotherapy over the years; an alkylating agent-free and anthracycline-free regimen is adequate treatment for low-risk patients
• Surgical assessment of the retroperitoneum should be reserved for patients who have enlarged lymph nodes on CT scans
• Children who are older than 10 years do carry a higher risk of lymph node involvement and relapse
Keskin et al., [2] reported their experience with 8 consecutive adults who had undergone treatment for para-testicular rhabdomyosarcoma between 2000 and 2010. They reported that pursuant to surgical excision, 7 patients had been classified into Group I according to the Intergroup Rhabdomyosarcoma Study Group (IRSG) Postsurgical Grouping Classification, and 1 patient was classified into IIB. Retroperitoneal lymph node dissection was not a required staging procedure staging procedure. Seven (7) of the 8 patients did receive adjuvant chemotherapy. No additional radiotherapy was administered to any of the patients. Keskin et al., [2] summated the results as follows:
• The ages of the patients had ranged between 18 years and 60 years and the median age was 24 years
• The commonest histology sub-type of a tumour was embryonal rhabdomyosarcoma which id constitute 75% of the tumors
• During the follow-up of the patients, 3 of the patients did experience local relapse and 5 distant metastases. The median progression-free and overall survival times were 17.0 +/- 9.9 months (and this had ranged between 5 and 31 months), and 27.3 (+/- 1.3 months (this had ranged between 16 months and 58 months) respectively
Keskin et al., [2] made the following conclusions:
• Para-testicular rhabdomyosarcoma is not a common malignancy in adults
• They had confirmed that patients who have localized para-testicular rhabdomyosarcoma could have different prognoses
• Retroperitoneal lymphadenectomy could be avoided as a treatment for para-testicular rhabdomyosarcoma pursuant to radical inguinal orchidectomy
Kumar et al., [3] retrospectively reviewed 10 patients who had been treated from July 2004 to December 2010. They noted the clinical characteristics and treatment modality in the form of surgery and chemotherapy (CCT). They did undertake statistical analysis with regards to Progression-Free Survival (PFS) and Overall Survival (OS) with the utilization of Kaplan-Meier survival analysis. Kumar et al. [3] summarized their results as follows:
• The median age of the patients was 16.5 years and the median duration of symptoms was 5 months
• Five patients did have retroperitoneal lymphadenopathy. (RPLAP) and three patients did have lung metastases, and one patient did have orbital metastases
• All patients did undergo high inguinal orchidectomy which was followed by systemic chemotherapy (CCT). Retroperitoneal lymph node dissection was not a required staging procedure
• Four patients did have a partial response to treatment and six patients did have a complete response
• The mean duration of Progression-Free Survival (PFS) was 48 months and the mean overall survival (OS) was 56 months
Kumar et al. [3] made the ensuing conclusions:
• Para-testicular rhabdomyosarcomas (RMS) are rare tumors that are associated with aggressive growth patterns
• Cure rates for para-testicular rhabdomyosarcoma have improved dramatically and 60% of patients in their series did have a complete response
• This success has been attributed to the development of multi-modality and risk-adapted treatment approaches
Breneman et al., [7] undertook a study to identify risk factors that are associated with metastatic Rhabdomyosarcoma (RMS) treated on the fourth Intergroup Rhabdomyosarcoma Study (IRS-IV). Breneman et al., [7] stated that patients who had metastatic Rhabdomyosarcoma (RMS) had been treated with one of two regimens that had incorporated a window of either Ifosfamide and Etoposide (IE) with vincristine, dactinomycin, and cyclophosphamide (VAC) or vincristine, melphalan (VM) and VAC. The study endpoints were Failure-Free Survival (FFS) and Overall Survival (OS). The clinical factors had included: age, histology, sites of primary and metastatic disease, and the number of sites of metastases were correlated with those endpoints. With regards to the results, Breneman et al., [9] reported the following:
• One hundred and twenty-seven patients had been eligible for analysis
• The estimated 3-year Overall Survival (OS) and Progress-Free Survival (PFS) for all patients were 39% and 25% respectively
• With the utilization of univariate analysis, the 3-year Overall Survival (OS) was significantly influenced by histology (47% for embryonal sub-type in comparison with 34% for all other types, P=0.026) and an increasing number of metastatic sites (P=0.028). With the utilization of multivariate analysis, the presence of two or fewer metastatic sites had been the only significant predictor (P =0.007 and 0.006, respectively). The combination of embryonal histology with two or fewer metastatic sites had identified a sub-group with 3-year Failure- Free Survival (FFS) of 40% and Overall Survival (OS) of 47%
Breneman et al. [9] made the ensuing conclusions:
• Children who have group IV rhabdomyosarcoma (RMS) and who were treated on the IRS-IV study did have improved overall survival (OS) and Failure-Free Survival (FFS) if they had two or fewer metastases and embryonal histology
• This favorable subset of patients did have outcomes that approached those that were observed in selected patients who had localized disease. These patients might not be appropriate candidates for regimens that include experimental agents that are associated with substantial toxicities or unproven anti-tumor activity
Newton et al., [8] stated that there was the need to develop a single prognostically significant classification of rhabdomyosarcoma (RMS) and other related neoplasms of children, adolescents, and young adults which would be a current guide for their diagnosis, allow valid comparison of outcomes between protocols that are carried out anywhere globally and should enhance recognition of prognostic subsets. Newton et al, [8] reported that 16 pathologists from eight different pathology groups, representing six countries and several cooperative groups, classified by four histopathologic classification schemes 800 representative tumors of the 999 eligible cases that had been treated on Intergroup Rhabdomyosarcoma Study II.
Each a tumour was classified based upon each of the four systems by each of the pathologists. Additionally, two independent sub-samples of 200 of the 800 patients had been reviewed based upon the new system, so that 343 distinct patients had been reviewed once, and 57 of these had been reviewed twice. Newton et al., [8] summated their results as follows:
• A study of the survival rates of all subtypes in the sample of 800 patients had led to the formation of a new system. This had been tested on two independent sub-sets of 200 of the original cases and had been found to be reproducible and productive of the outcome by utilization of univariate analysis
• A multivariate analysis of the 343 patients that had been classified based upon the new system had indicated that a survival model which includes pathological classification and known prognostic factors of the primary site, clinical group, and tumor size, had been significantly better at predicting survival in comparison with a model that had only the known prognostic factors
Newton et al. [8] made the ensuing conclusions:
• The new classification, which had been termed International Classification of Rhabdomyosarcoma (IRC) by the authors, had been reproducible and predictive of outcome among patients who had differing histology types of tumors that had been treated uniformly on the Intergroup Rhabdomyosarcoma II protocols
• They believe it should be used by all pathologists and cooperative groups to classify rhabdomyosarcomas so as to provide comparability among and within multi-institutional studies
Rypens et al., [10] stated that pediatric para-testicular primary malignant tumors are rare, and the majority of them tend to correspond to rhabdomyosarcoma (RMS). They also stated that:
• Para-testicular rhabdomyosarcomas (RMS) tend to have a better prognosis in comparison with RMS that originates from other locations, because of its favorable histology and possible early diagnosis
• The diagnosis tends to rely upon ultrasound scan findings of paratesticular hyper-vascular mass in an adequate clinical setting
Rypens et al., [10] reported the unusual appearance of an infiltrating rhabdomyosarcoma (RMS) a tumour in a 3-year-old boy. A tumor did present as a thickening of the tunica vaginalis. The atypical ultrasound scan appearance and discordance with clinical features did raise the suspicion of a tumoral process which enabled early diagnosis and treatment.
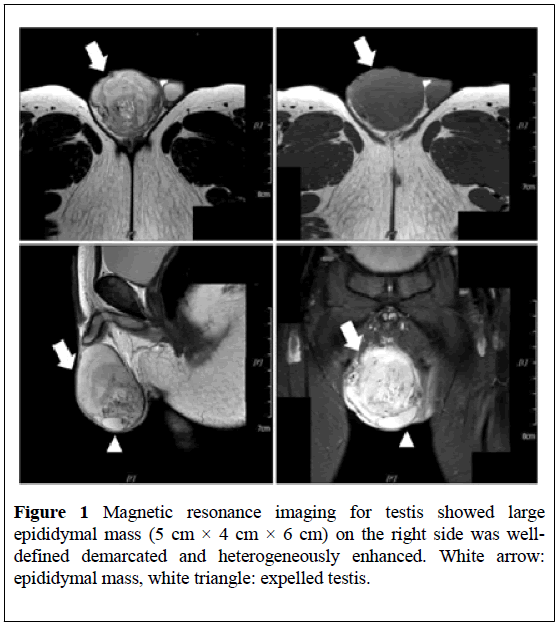
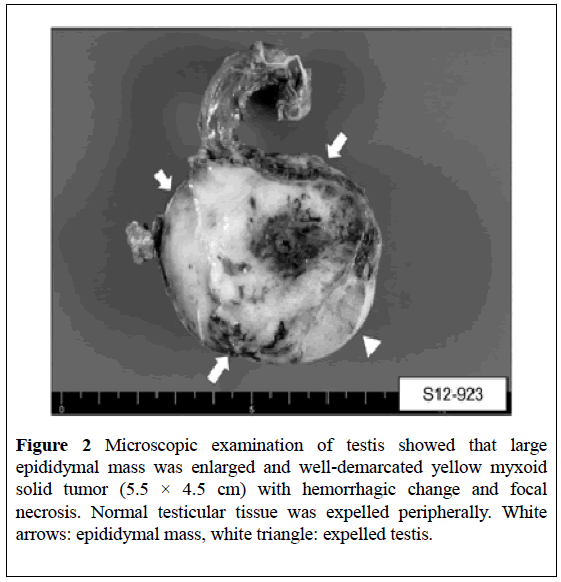
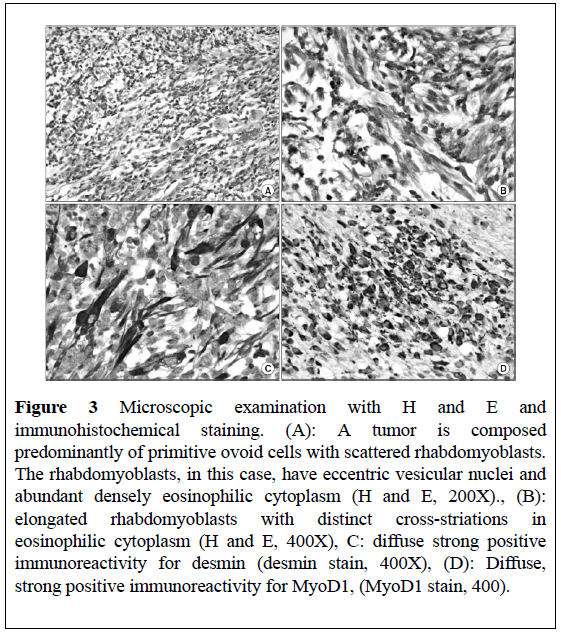
Kim et al., [11] reported a 10-year-old boy who had presented with a painful swelling in his scrotum on the right side which had lasted for 2 to 3 days. On examination he was found have mild tenderness and erythema of the right hemi-scrotum on the right side. He had ultrasound scan of scrotum at presentation which was reported to have shown that the right epididymis had a massive swelling that measured 4 cm × 3 cm that had markedly increased vascularity and that was considered to be suspicious for the diagnosis of severe epididymitis with the need to diagnose an epididymal tumor mass as a differential diagnosis with an adenomatoid tumor being considered a possible differential diagnosis. He was put on antibiotics as a treatment for epididymal-orchitis and discharged home on antibiotics and to be followed up in case the symptoms had persisted. After two weeks his pain and scrotal swelling had persisted and hence he was admitted for further investigation and exploration of the scrotum. The results of his blood test did show mild leucocytosis and normal lactate dehydrogenase, alpha-fetoprotein, and beta human chorionic gonadotrophin. He underwent scrotal exploration which excluded an abscess, but this showed mild adhesion due to inflammation as well as a hard epididymal mass in the right hemi-scrotum. An excision biopsy of the mass was undertaken. The tissue specimen was not large enough for the pathologist to confirm a definite diagnosis but a provisional diagnosis of at least a low-grade sarcoma was made. He subsequently had computed tomography scan of thorax, abdomen, and pelvis which did not reveal any metastases. He had Magnetic Resonance Imaging (MRI) scan of the testis which did show a large epididymal mass that measured 5 cm × 4 cm × 6 cm on the right side and this was adjudged to be well-demarcated and it did have heterogeneous enhancement (Figure 1). He subsequently underwent right radical orchidectomy and Hemi-scrotectomy due to tumor invasion of the scrotal wall. The gross examination did show that the large epididymal mass was an enlarged and well-demarcated yellow-myxoid solid tumor that measured 5.5 cm × 4.5 cm with hemorrhagic change and focal necrosis. Normal testicular tissue was expelled peripherally (Figure 2). The tunica albuginea and the testis had not been invaded by a tumor and the surgical margins were free of a tumour. Microscopy examination of the specimen did show a highly cellular tumor which was composed of rhabdomyoblasts as well as pleomorphic cells with ovoid hyperchromatic nuclei and containing eosinophilic cytoplasm (Figure 3). Immunohistochemistry staining of a tumor did show that a tumor had exhibited diffusely and strongly positive staining for desmin and MyoD1. The patient was classified into group I of the Intergroup Rhabdomyosarcoma Study (IRS) due to the fact that there was no metastasis. He received 3 cycles of adjuvant chemotherapy (VAC regimen. At his 1-year follow-up, he was free of disease.
Figure 2: Microscopic examination of testis showed that large epididymal mass was enlarged and well-demarcated yellow myxoid solid tumor (5.5 × 4.5 cm) with hemorrhagic change and focal necrosis. Normal testicular tissue was expelled peripherally. White arrows: epididymal mass, white triangle: expelled testis.
Figure 3: Microscopic examination with H and E and immunohistochemical staining. (A): A tumor is composed predominantly of primitive ovoid cells with scattered rhabdomyoblasts. The rhabdomyoblasts, in this case, have eccentric vesicular nuclei and abundant densely eosinophilic cytoplasm (H and E, 200X)., (B): elongated rhabdomyoblasts with distinct cross-striations in eosinophilic cytoplasm (H and E, 400X), C: diffuse strong positive immunoreactivity for desmin (desmin stain, 400X), (D): Diffuse, strong positive immunoreactivity for MyoD1, (MyoD1 stain, 400).
Lee and associates [12] reported a 16-year-old boy who presented with a palpable mass of the left testis. He was asymptomatic otherwise. On examination, he was found to have a hard and mildly tender left scrotal mass. The results of his serum alpha-fetoprotein and serum beta human chorionic gonadotrophin levels were within normal range. He had scrotal ultrasound scan which showed left extra-testicular masses with compression of the left testis. He had Computed Tomography (CT) scan of abdomen and pelvis which did show a left, extra-testicular, soft tissue mass in the scrotum with external compression of the left testis and associated with central necrosis and no evidence of any definite lymphadenopathy or metastasis. He underwent left intra-scrotal excision of a tumor and left orchidopexy with preservation of his left testis and spermatic cord. Histology examination of the specimen did reveal alternating areas of dense compact cellularity and loose myxoid tissue.
Majority of areas were found to have spindle cells that exhibited blunted central nuclei and tapered end nuclei with cytoplasmic cross-striations that had been arranged in densely arrayed whorls or fascicular patterns. Additionally, primitive ovoid cells that had scant cytoplasm and differentiated rhabdomyoblasts that had eccentric nuclei and dense eosinophilic cytoplasm were also observed. Immunohistochemistry studies of a tumor revealed the ensuing results:
• CK Negative (CK (-))
• Myogenin-Positive (Myogenin (+))
• Desmin-Positive (desmin (+))
• S-100-focal positive (S-100 (focal positive))
• Alpha smooth muscle actin-focal positive ((alpha smooth muscle actin (focal positive))
• CD 34-negative (CD 34 (-))
A final diagnosis of mixed embryonal and alveolar rhabdomyosarcoma was made and the surgical was free o tumor. He had a chromosomal analysis which was normal. He also had bone marrow examination which also did reveal normal cellularity with adequate megakaryocytes. He did receive combination chemotherapy pursuant to his operation that included vincristine, dactinomycin, and cyclophosphamide. He had follow-up CT scan of the abdomen and at the time of report of the case, there was no evidence of recurrent disease.
Valen et al., [13] a case of para-testicular rhabdomyosarcoma which was diagnosed by means of Fine Needle Aspiration (FNA) in an 18-year-old gentleman who had presented with enlargement of the right testis. The FNA did show mainly isolated small to medium-sized malignant cells with various shapes. Out of these, large rhabdomyoblasts were identified. Some tumor cells had shown longitudinal striations. Immunohistochemistry studies of the specimen showed the ensuing immunohistochemistry features:
• Strongly positive staining against
• Vimentin
• Desmin
• Negative immunohistochemistry staining against:
• Cytokeratins
• Smooth muscle antibody
• Epithelial-membrane antigen
• S-100
• Neuron-specific enolase
Histology examination findings of the surgical specimen were reported to be consistent with results of the FNA. Valen et al., [13] concluded that FNA represents a safe and accurate pre-operative procedure which is not associated with implications and FNA could be utilized in the outpatient setting which would enable a preliminary, pre-operative diagnosis, even for soft tissue tumors.
Manwah et al., [14] reported a 19-year-old gentleman who had presented with painless left scrotal mass and features of acute intestinal obstruction. The results of his serum alpha fetoprotein, beta human chorionic gonadotrophin and Lactic Dehydrogenase (LDH) were normal. He underwent laparotomy which revealed a small nodule in the sigmoid mesentery that was adjudged to be the cause of the obstruction. The nodule was excised and left orchidectomy was performed. Histopathology examinations of both specimens showed features of embryonal rhabdomyosarcoma. He was treated by means of chemotherapy but he died after 3 months.
Raney et al., [5] did enumerate lessons learned from studying 4292 patients who had rhabdomyosarcoma (RMS) in the Intergroup Rhabdomyosarcoma Study Group (IRSG) between 1973 and 1977. They did review the pathology materials and treatments the patients had received to ascertain compliance and to confirm response and relapse status. The patients in this study group were untreated patients who were aged less than 21 years at the time of diagnosis of the tumors and who had received systemic chemotherapy, with or without radiotherapy (XRT) and/or surgical removal of a tumor. Raney et al., [5] summated the results as follows:
• Survival at 5 years had increased from 55% to 71% over the period
• Important lessons that were learned included:
• The extent of disease at diagnosis affects prognosis
• Re-excising an incompletely removed tumor tends to be worthwhile if an acceptable and function can be preserved
• The eye, vagina, and urinary bladder can usually be saved
• Radiotherapy tends not to be necessary for children with localized, completely excised embryonal rhabdomyosarcoma
• Hyper-fractionation radiotherapy has thus so far not produced superior local control rates in comparison with conventional, once daily radiotherapy
• Patients who have non-metastatic cranial para-meningeal sarcoma could usually be cured with localized radiotherapy and systemic chemotherapy, without whole-brain radiotherapy and intra-thecal drugs
• Addition of doxorubicin, cisplatin, etoposide, and ifosfamide had not improved significantly the survival of patients who have gross residual or metastatic disease beyond that which had been achieved with VAC (vincristine, actinomycin D, cyclophosphamide) and radiotherapy
• Majority of patients who have alveolar rhabdomyosarcoma have a tumor-specific translocation
• Mature rhabdomyoblasts pursuant to the treatment of patients who have rhabdomyosarcoma of the bladder are not necessarily malignant, provided that a tumor has shrunk and the malignant cells have disappeared
Raney et al., [5] concluded that:
• Current IRSG-V protocols which they had summarized had incorporated recommendations for risk-based management
• Two new agents topotecan and irinotecan, are being investigated for patients that have an intermediate or high risk of developing recurrence
Kelly et al., [15] reported a 33-year-old man who had presented with a 2- months history of left-sided hemi-scrotal swelling which had increased in size. He had scrotal ultrasound scan which did show a heterogeneous large tumor within his left testis that had foci of calcifications. The levels of his tumor markers that included Beta-Human Chorionic antigen, alpha fetoprotein, and Lactate dehydrogenase were within normal range. He also had computed tomography scan of thorax, abdomen, and pelvis (CT TAP) which did not reveal any metastasis. He underwent left radical orchidectomy and histopathology examination of the specimen revealed an 11 cm poorly differentiated embryonal rhabdomyosarcoma of the testis which had focally involved the full thickness of the tunica albuginea but which had not involved the tunica vaginalis. The resected margin and the spermatic cord were free of a tumour. Immunohistochemistry staining of a tumor did exhibit negative staining for the ensuing markers:
• Alpha fetoprotein (AFP)
• Human Chorionic Gonadotrophin (HCG)
• Placental Alkaline Phosphatase
• C-kit
• CD30, and
• Desmin
Immunohistochemistry studies did show that a tumor had exhibited positive staining for the following tumor markers:
• Myogenin, and
• Phosphotungstic acid hematoxylin
The immunohistochemistry staining features of a tumor were adjudged to be diagnostic of Embryonal Rhabdomyosarcoma (ERMS) of the testis.
He had Computed Tomography (CT) scan of the brain which was normal. He had a course of adjuvant chemotherapy upon the advice from a multi-disciplinary team discussion having taken into consideration that a tumor was poorly differentiated. He had CT TAP at 3 months and his CT TAP images up to the time of the report of the case had not shown any evidence of metastasis or nodal recurrence.
Duduyemi et al., [16] reported a 22-year-old man who had presented with 3 weeks history of left inguinoscrotal swelling which had suddenly become painful 2 days preceding his presentation, as well as he had a fever, vomiting, abdominal distension, and urinary symptoms. He was found to be ill-looking, febrile with a temperature of 37.8 degrees centigrade, moderately pale, not icteric, and no evidence of lymphadenopathy. He had a uniformly distended abdomen that was tender and dull on percussion and hypoactive bowel sounds. The inguinoscrotal mass was found to be irreducible and he also was found to have a palpable left testicular mass. He had an ultrasound scan of abdomen and pelvis which did reveal massive ascites and a mass within his right lumbar region. A provisional diagnosis of obstructed left inguinoscrotal hernia which was associated with peritonitis and a right lumbar mass was made. He underwent laparotomy, right nephrectomy and left orchidectomy. Macroscopic examination of the specimens revealed that the renal mass had measured 16 cm × 10 cm × 4 cm and had weighed 230 grams; the left testicular mass had measured 10 cm × 6 cm × 4 cm which had weighed 55 grams. Cut sections of both the renal mass and the testicular mass did show grey-white fleshy appearances with that had been associated with focal areas of hemorrhage and necrosis. Microscopy examination of the testicular and renal tissues revealed features that had been adjudged to be consistent with the diagnosis of rhabdomyosarcoma with a differential diagnosis of sarcomatoid renal cell carcinoma. Immunohistochemistry studies of the testis and kidney tumor tissues exhibited the following features:
• Negative Immunohistochemistry staining with:
• S100
• Pancytokeratin
• OCT3/4
• AFP
• Strongly Positive Immunohistochemistry staining with:
• Actin.
• Desmin
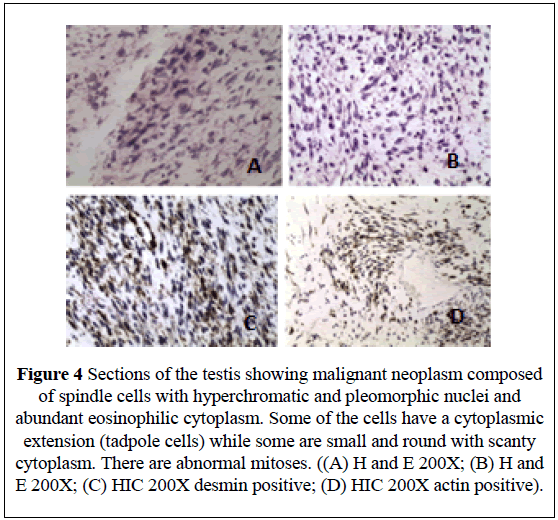
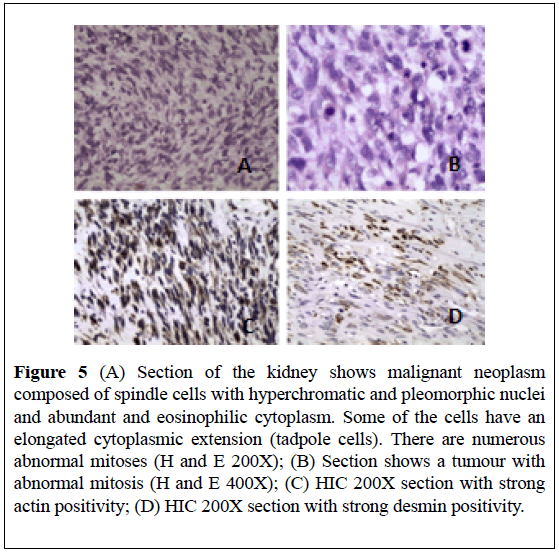
The strongly positive immunohistochemistry staining for Actin and Desmin was adjudged to be consistent with the diagnosis of rhabdomyosarcoma (Figures 4 and 5). He was discharged on the 14th postoperative day but was lost to follow-up and attempts to find him had failed. Lessons to learn from this case report include: Rhabdomyosarcoma of the testis could occasionally be associated with a synchronous rhabdomyosarcoma elsewhere in the body; nevertheless, in view of the fact that staging computed tomography scans of the thorax, abdomen, and pelvis tend to be undertaken for the full assessments of patients who have rhabdomyosarcoma of the testis it should be unlikely these days that globally a synchronous rhabdomyosarcoma elsewhere in the body would be missed; the fact that the reported patient was missed from follow-up should be evidence for clinicians to take steps to ensure that patients with rhabdomyosarcomas and other malignant tumors should be thoroughly counseled in hospital before they are discharged and the contact details of the patients and their next of kin’s should be well documented as well as the patients should be provided with the contact details of a responsible nurse that would provide support to each patient any time.
Figure 4: Sections of the testis showing malignant neoplasm composed of spindle cells with hyperchromatic and pleomorphic nuclei and abundant eosinophilic cytoplasm. Some of the cells have a cytoplasmic extension (tadpole cells) while some are small and round with scanty cytoplasm. There are abnormal mitoses. ((A) H and E 200X; (B) H and E 200X; (C) HIC 200X desmin positive; (D) HIC 200X actin positive).
Figure 5: (A) Section of the kidney shows malignant neoplasm composed of spindle cells with hyperchromatic and pleomorphic nuclei and abundant and eosinophilic cytoplasm. Some of the cells have an elongated cytoplasmic extension (tadpole cells). There are numerous abnormal mitoses (H and E 200X); (B) Section shows a tumour with abnormal mitosis (H and E 400X); (C) HIC 200X section with strong actin positivity; (D) HIC 200X section with strong desmin positivity.
Delto et al., [17] reported a 24-year-old man who had presented with a painless right scrotal mass of 3 weeks duration. He was found on examination to have a non-tender right epididymal mass which had measured about 1 cm. He had a scrotal ultrasound scan which showed a small mass in his right epididymal tail that had questionable vascularity. Both his testes were normal. He was placed on surveillance with the provisional assumption that the lump was a benign lesion. At his 3 months follow-up, it was discovered that the lump had enlarged. He then had a repeat ultrasound scan of the scrotum which had shown enlargement of the right epididymal tail lesion together with 2 new additional lesions that measured up to 3 cm.
The lesions were noted to be hypervascular and the testis were normal. His serum tumor marker levels were normal. He had computed tomography scan which did not reveal any lymphadenopathy or metastasis. He underwent exploration of the right hemi-scrotum which had revealed that the masses were related to his right epididymal tail. Frozen section examination of samples of the lesions were inconclusive but had revealed predominantly spindle cell neoplasm with sarcoma considered as a differential diagnosis. The lesions were excised but the right testis and the spermatic cord were preserved. The features of the lesions on pathology examination were adjudged to be consistent with the diagnosis of pretesticular embryonal rhabdomyosarcoma of the spindle cell type. The lesions on immunohistochemistry studies did exhibit the ensuing staining features:
Positive immunohistochemistry staining with:
• Myogenin, and
• Desmin;
• The positive immunohistochemistry staining features had been adjudged to be indicative of skeletal muscle differentiation
Negative immunohistochemistry staining with:
• Human Melanoma Black-45
• Smooth muscle actin, and
• S-100
The surgical resection margins were clear of a tumour. The aforementioned findings were adjudged to be consistent with a final diagnosis of T1N0M0 para-testicular rhabdomyosarcoma of the spindle cell type. The patient was offered the option of radical inguinal orchidectomy and ipsilateral nerve sparing lymph node dissection followed by chemotherapy upon the advice of the medical oncologist; nevertheless, the patient refused to undergo any further surgical operation but he did agree to have chemotherapy which had been initiated at the time of the report of the case. There was no long-term follow-up outcome of this case.
It would be pointed out that some of the lessons learned from this case report include:
Clinicians always need to accept patients a choice of self-determination after careful explanation of all treatment options available. The reported patient was advised to undergo radical orchidectomy and ipsilateral nerve sparing lymph node dissection as an additional precaution to provide treatment of curative intention after having taken into consideration the surgical margins were negative of a tumour and this surgical operation was to be followed by chemotherapy. Nevertheless, the patient declined to undergo any further surgery. The clinicians in this case correctly accepted the choice of the patient. It could be argued that chemotherapy pursuant to excision of the lesions with preservation of the right testis and spermatic cord followed by chemotherapy is a good alternative treatment of curative intent with regards to this case scenario. Nevertheless, it could be argued that the drawback with regards to the case report was published too early without waiting for the intermediate term and long-term outcome in that there it cannot be ascertained with regards to the case whether or not the surgical excision of the lesions with clear margin followed by chemotherapy was adequate treatment with long-term outcome. Based upon this anecdotal case report it would be argued further that the best way to determine whether surgical excision of para-testicular rhabdomyosarcoma with preservation of the testis and spermatic cord followed by chemotherapy does achieve similar long-term outcome as treating a para-testicular rhabdomyosarcoma by local excision plus radical orchidectomy plus ipsilateral lymph node dissection followed by chemotherapy, there would be the need to establish a large-scale multicentre study that would compare the two forms of treatment in order to establish a consensus opinion on the treatment options. Ipsilateral lymph node dissection and radical orchidectomy would provide apparent greater morbidity in comparison with local excision of the para-testicular lesion that has the additional advantage of preservation of the testis.
Conclusion
Rhabdomyosarcoma of the testis, epididymis, spermatic cord including all tumors classified as para-testicular rhabdomyosarcoma are rare tumors which have an aggressive potential which does present with a short history; these tumors generally are associated with normal serum tumor marker levels; diagnosis tends to be confirmed by the histopathology features of the tumors and typical immunohistochemistry features of the tumors (positive staining for myogenin, desmin, actin, vimentin, and others as stated in the paper); these tumors are generally treated by means of surgical excision and chemotherapy and radiotherapy would be given for local control of disease; prognosis tends to be worse for advanced metastatic disease and in patients who are less than 1-year-old or equal to or greater than 10 years old as well as upon the classification of a tumor.
REFERENCES
- Ferrari A, Bisogno G, Casanova M, et al. Paratesticular rhabdomyosarcoma: report from the Italian and German Cooperative Group. J Clin Oncol 2002;20:449-55.
- Keskin S, Ekenel M, Basaran M, et al. Clinicopathological characteristics and treatment outcomes of adult patients with paratesticular rhabdomyosarcoma (PRMS): A 10-year single-centre experience. Can Urol Assoc J 2012;6:42-5.
- Kumar R, Kapoor R, Khosla D, et al. Paratesticular rhabdomyosarcoma in young adults. A tertiary care institute experience. Indian J Urol 2013;29:110-13.
- Ferrari A, Casanova M. Current therapeutic strategies for rhabdomyosarcoma. Expert Rev Anticancer Ther 2005;9:283-294.
- Raney RB, Mauner HM, Anderson RJ, et al. The Intergroup Rhabdomyosarcoma Study Group (IRSG): Major lessons from the IRS-1 through IRS-IV studies as background for the current IRS-V treatment protocols. Sarcoma 2001;5:9-15.
- Terezakis SA, Wharam MD. Radiotherapy for rhabdomyosarcoma: indication and outcome. Can Oncol (R Coll Radiol) 2013;25:27-35.
- Breneman CJ, Lyden E, Pappo AS. Prognostic factors and clinical outcomes in children and adolescents with metastatic rhabdomyosarcoma-A report from the intergroup rhabdomyosarcoma study IV. J Clin Oncol 2003;21:78-84.
- Newton W A Jr, Gehan EA, Webber B L, et al. Classification of rhabdomyosarcoma and related sarcomas. Pathologic aspects and proposal for a new classification-an Intergroup Rhabdomyosarcoma Study. Cancer 1995;76:1073-88.
- Breneman JC, Lyden E, Pappo AS, et al. Prognostic factors and clinical outcomes in children and adolescents with metastatic rhabdomyosarcoma-a report from the Intergoup Rhabdomyosarcoma Study IV. J Clin Oncol 2003;21:75-84.
- Rypens F, Garel L, Frano-Guimond J, et al. Paratesticular rhabdomyosarcoma presenting as thickening of the tunica vaginalis. Pediatr Radiol 2009;39:1010-12.
- Kim YJ, Huh JS, Hyun CL, et al. A case of pediatric paratesticular rhabdomyosarcoma with epididymitis The World Journal of Men’s Health 2012;30:146-49.
- Lee HY, Tsai CC, Huang CH, et al. Mixed-type paratesticular rhabdomyosarcoma-A case report. Kaohiung Journal of Medical Sciences 2011;27:239-41.
- Valen RM, Papanikolaou A, Panagiolou A, et al. A rare case of paratesticular rhabdomyosarcoma diagnosed by fine needle aspiration: a case report. Acta Cytol 2009;53: 319-22.
- Manwah N, Marwah S, Gill M, et al. Adult Paratesticular Rhabdomyosarcoma Presenting as Acte Intestinal Obstruction-A case report. Indian J Surg 2013;75:143-44.
- Kelly B, Lundon D, Rowaiye B, et al. Embryonal rhabdomyosarcoma of the testis. Can Urol. Assoc Urol J 2011;5:E7-E10.
- Duduyemi BM, Yifieyeh AC, Afihene MY. Synchronous rhabdomyosarcoma of the testis and kidney. A case report and review of the literature. Alexandria Journal of Medicine. 2016;52:193-196.
- Delto JC, Wayne GF, Garces S, et al. An adult case of paratesticular spindle cell rhabdomyosarcoma. Urology Case Reports 2014;2:126-8.