Short note on intestinal ischemia
Received: 03-Nov-2021 Accepted Date: Nov 17, 2021; Published: 24-Nov-2021
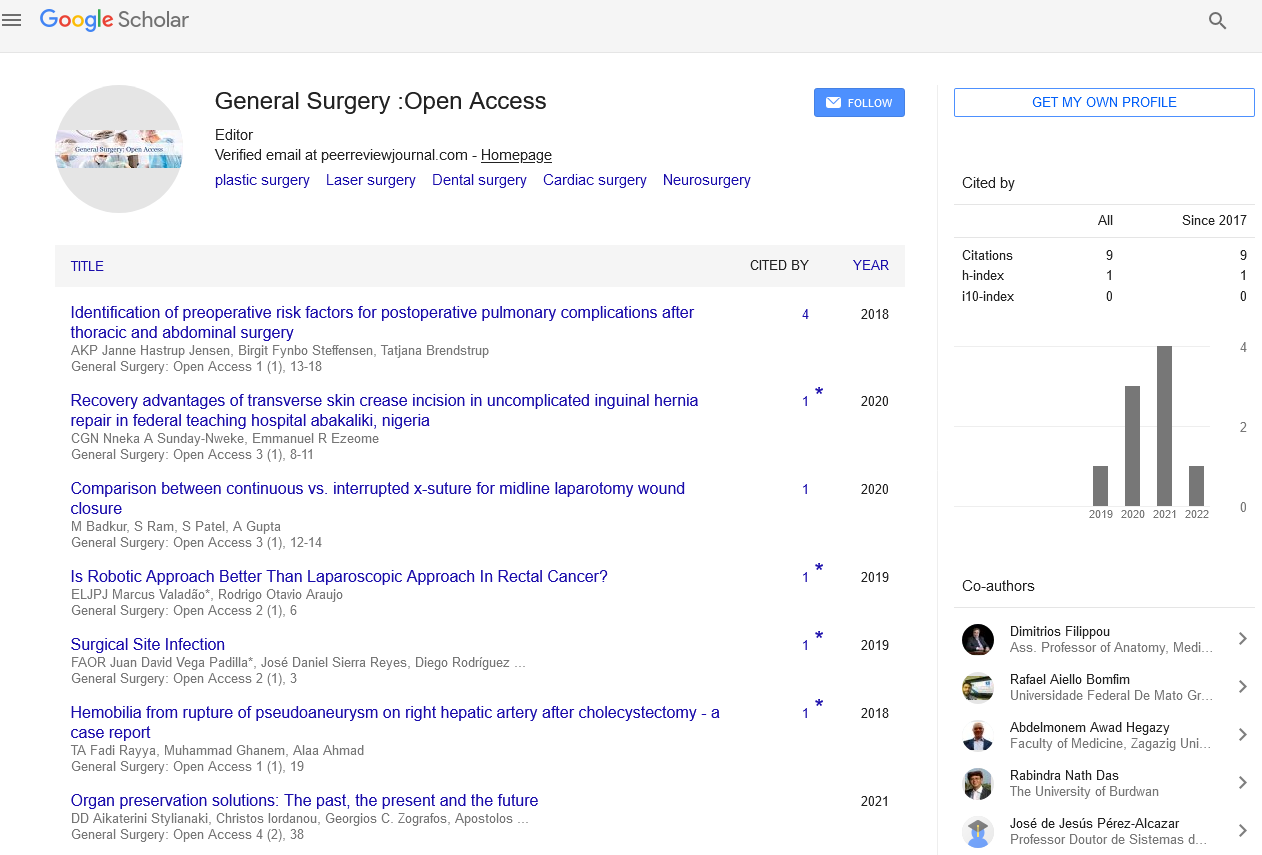
Citation: Rattan V. Short note on intestinal ischemia. Gen Surg: Open Access. 2021;4(6):52.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Description
Small intestinal ischemia (also called mesenteric ischemia) is a group of potentially life-threatening disorders that reduce blood flow to the superior mesenteric artery intestine (duodenum, jejunum, ileum, etc). Symptoms range from mild to severe, depending on the cause. If you have severe stomach pain, early diagnosis and treatment are essential for the best possible results in the recovery of digestive function.
Intestinal ischemia can be classified into superior mesenteric artery intestinal ischemia, commonly known as mesenteric ischemia, and colonic ischemia, commonly known as Large intestine ischemia. Intestinal ischemia occurs when intestinal blood flow is reduced by at least 75% over a period of 12 hours or more. Abdominal pain is the most common symptom in people with intestinal ischemia. Intestinal ischemia can affect the superior mesenteric artery or large intestine and can occur for any reason, resulting in reduced blood flow to the intestine. This is a rare condition, but it has a high mortality rate. The intestine is primarily supplied by two large arteries including the superior mesenteric artery (SMA) and the inferior mesenteric artery (IMA). Superior mesenteric artery supplies the intestine from the lower duodenum to two-thirds of the transverse colon. Inferior mesenteric artery supplies the large intestine to the rectum from the distal third of the transverse colon. Celiac disease also has collateral to supply the intestines. Two major areas of the colon, including the flexion of the splenic flexure (Griffith point) and the recto sigmoid junction (Sudek’s point) are susceptible to ischemia. These are also known as "water shed areas” which mean the regions in the colon between 2 major arteries that supplying colon. Splenic flexure is the area between superior mesenteric artery and inferior mesenteric artery supplies, and the recto sigmoid junction is the region between the inferior mesenteric artery and the superior rectal artery supplies. The splenic flexure is the area between the superior mesenteric artery and the inferior mesenteric artery supply, and the rectal sigmoid junction is the area between the inferior mesenteric artery and the superior rectal artery supply. These areas are primarily inferior mesenteric artery supplied by the marginal arteries. However, in 50% of the population, this artery is underdeveloped. The catchment area accounts for about 70% of cases of ischemic colitis. The venous drainage of the large intestine is parallel to the arterial supply. The superior mesenteric vein drains the area supplied by the superior mesenteric artery, and the inferior mesenteric vein drains the left side of the colon and rectum. A sharp decrease in mesenteric artery blood flow accounts for 60%-70% of patients with mesenteric ischemia. The remaining causes are associated with colonic ischemia and CMI. Abdominal pain is the most common symptom in people with intestinal ischemia. Some characteristics of the patient help to distinguish between acute superior mesenteric artery intestinal and colonic ischemia. Patient characteristics such as age over 60 years, no serious clinical picture, slight abdominal pain, tenderness, rectal bleeding, and bloody diarrhea are more common features in acute colonic ischemia. Computed tomography of the abdomen is commonly used in hemodynamically stable patients with acute abdominal pain. CT and MR angiography are the first tests in patients with a high suspicion of intestinal ischemia. Various drug treatments have been proposed based on the acute mesenteric ischemia subtype. Papaverine can be used through angiographic catheters with all arterial morphology of AMI and the mechanism of relaxation of vascular vasospasm in nonobstructive mesenteric ischemia.
Necrosis of the mucosal villi is the first change and usually occurs within 3-4 hours of intestinal ischemia. This can leads to transmural, mural, or mucosa infarction. Splenic flexure and rectal sigmoid junction are often prone to decreased blood flow and hypoxia. The first reaction to an injury is an obstruction of the intestinal wall. It then appears to be edematous, fragile, and hemorrhagic. Without intervention, bowel bleeding can occur within 1 to 4 days. The gut bacteria then cause intestinal gangrene and perforation.