The association of self-efficacy and self-management behavior in adult patients with chronic kidney disease: an integrative review
Received: 01-Jun-2018 Accepted Date: Jun 11, 2018; Published: 17-Jun-2018
Citation: Sorait W. The Association of Self-Efficacy and Self-Management Behavior in Adult Patients with Chronic Kidney Disease: An Integrative Review. J Kidney Treat Diagn 2018;1(1):33-40.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Objectives: The objective of this integrative review was to examine the relationship between self-efficacy and self-management behavior in CKD patients and identify components of self-efficacy that may improve selfmanagement behavior in adults diagnosed with stage 1-5 CKD.
Background: Chronic kidney disease (CKD) is rising in prevalence worldwide, as shown by increases of attributive disease, as well as increases in incidence and prevalence of end-stage kidney disease. Best practice guidelines describe the beneficial outcomes of self-management intervention and indicate that a targeted self-management program is successful in enhancing patient selfmanagement and patient-centered outcomes. The essential elements of self-efficacy and self-management for CKD patients should be identified correctly in the early stage of CKD. However, it is not clear how to identify those relevant and sufficiently validated self-efficacy components that can lead to the development of a self-efficacy and self-management instrument or intervention suitable for patients with CKD. Design: An integrative literature review was conducted.
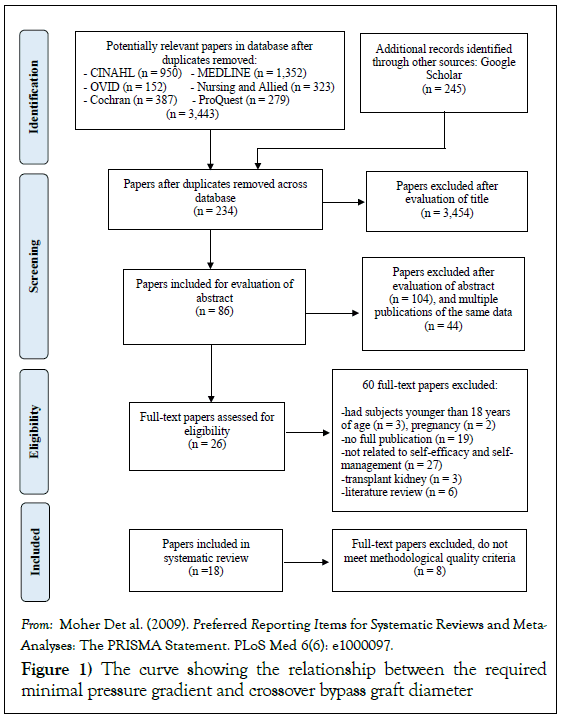
Methods: A search was conducted using CINAHL, PubMed/MEDLINE, Cochrane, ProQuest, Ovid, and Google Scholar. Published qualitative and quantitative studies, abstracts or dissertations describing the components and factors of self-efficacy associated with outcomes of self-management behaviors and interventions for people with CKD, and published in English between 2007 to 2017, were included. The associations were identified and described, and evidence was presented using Whittemore and Knafl’s framework [1] and Cooper’s method [2] to guide each stage of the review.
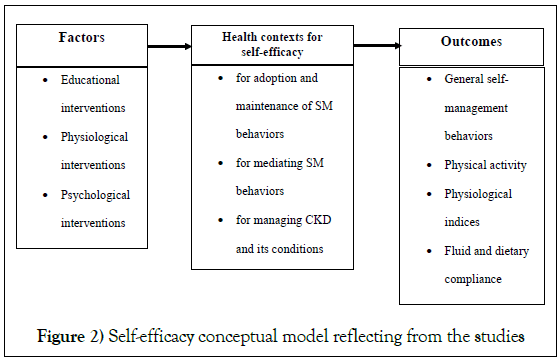
Results: Eighteen publications related to self-efficacy and self-management behaviors in patients with a variety of CKD stages were identified. Selfefficacy was mostly found to involve educational interventions. Educational, physical and psychological interventions to improve self-efficacy were evident, but few interventions led to significantly improved self-efficacy. Self-efficacy health contexts reflected in the studies were found as associations with selfmanagement behaviors related to management of CKD and its condition, adoption and maintenance of self-management behaviors, and mediation or modification of self-management behaviors to improve the effectiveness of self-care.
Conclusions: Various forms of self-efficacy can support self-management behaviors by persons with CKD. Understanding the function and concept of self-efficacy is important in developing simple and targeted implementations and supporting the efforts of CKD patients to manage their illness.
Keywords
Chronic kidney disease; Self-efficacy; Self-management; Integrative review
Chronic kidney disease (CKD) is prevalent worldwide and is ranked as one of the top ten chronic illnesses. CKD is defined as kidney damage occurring as proteinuria, hematuria, or an anatomical abnormality [1-3]. It is indicated by the estimated Glomerular Filtration Rate (eGFR) being less than 60 ml/min/1.73 m2 presented on at least two occasions at least 90 days apart [4-6]. Currently, the burden of CKD is shown by increases in attributive disease, as well as increases in incidence and prevalence of endstage renal disease (ESRD) [3,4]. Historically, CKD treatment mainly focused on individuals with ESRD, dialysis treatment, or kidney transplants [7]. More recently, as increasing rates of CKD incidence have become evident, nephrologists and nephrology nurses have assumed more responsibility for taking care of persons with CKD before ESRD occurs [8,9]. Additionally, patients who fall within the CKD stages 1 to 2 (GFR greater than 60 mL/ min/1.73 m2), should have a focused exam identifying factors driving CKD [3]. Living with kidney disease usually requires changes in the person’s lifestyle, especially in the early stage of CKD [5,9].
Prevention programs will function best when they operate as part of a national non-communicable disease strategy, with more involvement of general practitioners being recommended [10,11]. Bonner et al. [12], Ferris et al. [13], Lee et al. [14], and Lin et al. [15] strongly posit the beneficial outcomes of self-management interventions and suggest that a targeted selfmanagement program can improve patient self-management and patientcentered outcomes. In addition, researchers have found clinically significant differences in eGFR levels in patients engaged in self-management programs [14-16]. It appears that a self-management intervention can decelerate the progression of CKD. The approaches of self-management have been widely accepted and adopted by health care providers, patients, and families who enter into partnerships to manage health care across all aspects of treatment in order to delay the progression of CKD and increase survival [17,18].
Self-management is defined as a person’s ongoing attempts to regulate and contribute to health care maintenance for good health in their daily lives [19]. It also includes individual endeavors based on well-defined roles that improve emotional management to enhance health, avoid complications, regulate symptoms, establish medical resources, and diminish disturbances from the disease through carefully chosen lifestyles [13,15,20]. Therefore, Lorig and Holman [20] recommend that self-management and its roles should be applied as interventions when providing health care benefits to people with chronic diseases. The consequence of self-management behaviors in CKD is related to the requirement that individuals increase their confidence in their own capability to monitor a self-care routine in CKD by increasing their self-efficacy [15,17]. Researchers studying self-management have concluded that, by developing effective approaches to deal with illness and associated conditions, individuals can improve their healthy behavior [12,13,21-24].
The theory of self-efficacy verifies the descriptive and predictive powers of self-management in various areas of life to reduce the severity of disease burden for chronically ill patients [25]. The efficacy of individual beliefs can also help justify the maintenance of complex relationships that occur among self-management endeavors necessary for healthy lifestyle changes in patients with chronic diseases [16,17]. Patients with greater self-efficacy have been shown to practice more self-management behaviors, leading to better disease control, and better physical functioning [19]. Also, self-efficacy has been identified as a moderator or mediator of self-management [14].
Self-efficacy, which plays an important role in the reduction of CKD progression, has been included in various approaches for use with persons diagnosed with CKD in all stages, specifically with patients on hemodialysis and peritoneal dialysis [26-28]. Although many studies have focused on searching for factors of self-efficacy that influence CKD patients’ behaviour [29-31] and its implementation for ESRD patients [8,13,18,22,23,26], studies describing the relationship between self-efficacy and self-management behaviors that can be used specifically in the early stage of CKD are few, and their implications are not clear. Information on such topics can be useful for properly selecting relevant and sufficiently validated self-efficacy components that can lead to the development of a self-efficacy and selfmanagement instrument or intervention suitable for patients with earlystage CKD. To address these important issues, this integrative review will examine the recent literature relating to self-efficacy and self-management components associated with CKD in early stages [1-3]. The overall results of the integrative review may inform clinical healthcare personnel, and provide an alternative to traditional health education programs designed to delay disease progression.
Purpose/Objectives
The aim of this integrative literature review is to examine the relationship between self-efficacy and self-management behavior in CKD patients and identify components of self-efficacy reported to improve self-management behavior in adults diagnosed with CKD. This review will help to determine which aspects of perceived self-efficacy and self-management can be implemented in order to improve the outcomes of people with CKD. An integrative literature review combines the evidence of multiple studies regarding a specific problem and is the method of option for evidencebased practice initiatives [1]. Therefore, the results of this integrative review will utilize well-specified clinical questions and a comprehensive search for relevant primary studies.
Research Questions
This analysis aims to answer the following questions:
1. What are the health contexts of self-efficacy related to CKD?
2. What factors improve self-efficacy in the CKD patient group?
3. Does perceived self-efficacy of CKD patients promote self-management behaviours to delay the progression of CKD?
Methods
Design
An integrative review of the literature was selected, as this type of analysis can help to explore the relationship between self-efficacy and self-management behavior in CKD patients. The method of an integrative review based on the framework of Whittemore and Knafl [1] was adopted. To enhance rigor in integrative reviews, the research review was conducted through application of the framework as encompassing a problem identification stage, a literature search stage, a data evaluation stage, and a presentation stage [1].
Search Strategy
The systematic search strategy aimed to find relevant studies published between 2007 and 2017, using a three-step approach. First, a systematic review was conducted based on analysis of text words in the following databases: CINAHL, PubMed/MEDLINE, Cochrane, ProQuest, Ovid, and Google Scholar. This step helped to identify optimal search terms, which were used to perform a comprehensive search of all relevant databases [32]. The four index-terms were “Chronic Kidney Disease,” “Kidney Disease,” “self-efficacy,” and “self-management.” If those terms were contained in the title and abstract, the study was selected and reviewed. Moreover, whenever these words were combined used the words “or” and “and,” they were examined self-efficacy and self-management regarding chronic kidney disease contexts. These terms were searched as title, abstract, or keyword. A second search used all identified keywords, and index terms were then taken across all included databases. Third, the reference list of each identified article was searched for additional studies. Published studies were reviewed in May 2017. Reference lists of relevant articles were also considered in order to determine additional reviews. All abstracts and full articles were independently read, as necessary.
Inclusion and Exclusion Criteria
The reviewer considered whether to include or exclude an article according to selection criteria. Articles were incorporated if they were written in English and they met all the following criteria: (1) they were original studies with qualitative, quantitative, descriptive, analytical or experimental designs, (2) they studied adult human populations (aged ≥ 18 years) with CKD at all disease stages, and (3) they studied the association of CKD, self-management, and self-efficacy. The exclusion criteria were used to eliminate any case series, studies of children, studies of pregnant women, and studies of patients with acute kidney injury (AKI) and kidney transplant (KT).
Method of the Review
An integrative review method is a systematic approach using a detailed search procedure to find relevant evidence of varying levels and perspectives to reply to a specific scientific question [1]. Evidence may be obtained from studies that used quantitative and qualitative research methods and from observational studies. Additionally, this paper used the integrative review approach to present a diverse number of sources that might increase the understanding of self-efficacy in CKD patients, hoping to inform nursing practice.
This study also used Cooper’s [2] guidelines for completing an integrative review. At the start, papers selected for retrieval were considered by the reviewer for methodological quality. Selected papers were assessed using a problem formulation that included identifying the topic to be inspected, clarifying the question to be answered, and demonstrating whether the inclusion and exclusion criteria for the search method had been met. Second, for the step of data collection, the reviewer screened titles and abstracts and deleted those published studies that did not meet the inclusion criteria and also identified all publications on the identified problem/topic and gathered information from the search using keywords. Then, the full texts of presumably relevant studies were obtained and assessed for eligibility. To evaluate the data, results were extracted from studies by assessment of the quality or hierarchy of evidence. Next, the data analysis and interpretation were examined by interpreting information such as findings, themes or concepts from selected publications. Later, the extracted data were presented in a table. Finally, a report was prepared, including developing tables, graphs, or narratives of results for publication and presentation. The primary outcomes of selected articles were presented in a PRISMA 2009 Flow Chart (Figure 1).
Results
Description of Studies
The process of paper selection and exclusion is illustrated in Figure 1 through literature searching, 41,561 articles were identified as related to CKD, and 4,672 were identified as related to self-efficacy and self-management. Then, 3,688 of those papers were identified as associated with CKD, self-efficacy, and self-management. Eighty-six articles met the inclusion criteria of being written in the English language and being published between the years 2007 and 2017. Twenty-six of these papers were retrieved for detailed examination after review of their abstracts and removal of duplicates. After eight were excluded on the basis of screening the abstracts and the full-text articles, the final number of included papers was eighteen. Eight studies were conducted in the U.S. [8,21,33-37], three in Taiwan [15,38,39], two in China [40,41], and two in Japan [42,43]. One study was performed in the Philippines [44], one in Thailand [7], and one in the Netherlands [45]. The total number of participants was 1,898. The stage of CKD varied across the studies. Most of the studies (n=6) focused on CKD patients with end-stage or HD. Two studies included only people with early-stage CKD (1-3a) [15,45]. As for the study design, nine studies were RCTs, and nine were cross-sectional studies.
The use of theory to guide study design or intervention development was reported. Self-efficacy was involved in several types of theory. The study of Patterson et al. [36] and Wu et al. [39] used social cognitive theory (SCT) to examine the effect of self-management on CKD outcomes. Based on SCT, Bandura’s self-efficacy theory was used in the study of Balaga [44], Sritarapipat and colleagues [7], and John and associates [34], and self-regulation theory was applied in the studies done by Lin et al. [15], Kauric-Klien et al. [35], and Meuleman et al. [45]. One intervention study used the Precaution Adoption Process Model (stages of change) and Health Belief Model theory (HBM) to assess individual health belief, and action stages related to dietary adherence focused on a low-phosphorus diet in patients on HD [33]. Also, one study [38] applied the theory of cognitive-behavioral therapy (CBT) with a group intervention to improve the quality of life in hemodialysis patients. It was not clear; however, how fundamental constructs of the theories were integrated into the intervention or study design. Moreover, intervention mechanisms were not tested in these studies. Use of a particular theory to guide the studies or intervention development was not reported in eight studies [8,21,28,37,41-43].
Self-efficacy, as measured in the eighteen studies, varied. Sixteen studies applied the original version of a self-efficacy tool that included the selfefficacy scale for health behaviors in patients with chronic diseases [42,43], the CKD Self-Efficacy Scale [15,39] the Self-Efficacy for Managing Chronic Disease 6-Item Scale [28], the Self-efficacy for Exercise (SEE) scale [41], the Chronic Disease Self-Efficacy Scales to Manage Disease in General [40,45], the Strategies Used by People to Promote Health (SUPPH) [38], Self- Efficacy and Self-Management Behaviors in Patients with Chronic Kidney Disease tool [7,8]; the Perceived Efficacy in Patient-Physician Interaction Questionnaire (PEPPI) [21]; the Spinal Cord Injury Exercise Self-Efficacy Scale [36]; the Chronic Disease Self-Management Program’s (CDSMP) Diabetes Self-efficacy Scale [37]; a modified version of the Your Health and Well-Being Questionnaire [34]; and the Chronic Kidney Disease Self- Efficacy Scale [33]. Kauric-Klien and associates [35] used the BP Control in HD Self-Efficacy Scale adapted from the original scale of self-efficacy in the management of Type II Diabetes mellitus developed by Bijl, Peoelgeest- Eeltink, and Shortridge-Baggett [18]. One study [44] did not report the selfefficacy instrument but self-efficacy was still measured.
Health Contexts for Self-efficacy Reflected in the Studies
Nine studies were classified into three categories of health contexts for selfefficacy. The first category was a health context for self-efficacy to manage CKD and it’s underlying, such as physiological indicators related to the CKD conditions that affect illness [44], fluid and diet compliance with HD patients and barriers that prevent patient compliance [34], and serum phosphorus level [33]. In two studies [34,44], the researchers did not discuss the components of self-efficacy. However, they used a tool that consisted of a general self-efficacy term to assess patients’ beliefs about controlling and managing CKD, physiological indices of the level of diet adherence and medical compliance (e.g., albumin, pre-blood urea nitrogen, interdialytic weight gain, phosphorus, hemoglobin, and hematocrit) [44], and fluid and dietary restriction compliance [34]. Participants who reported high selfefficacy were more likely to self-report fluid and dietary restriction compliance [34]. Only Elliott et al. [33] described the details of self-efficacy that focused on aspects of lifestyle management regarding diet and medication adherence. Additionally, the investigators suggested that building patients’ self-efficacy may help them to achieve both improved phosphorus dietary adherence and better serum phosphorus control [33].
The second category was a health context for self-efficacy to adopt or maintain healthy behaviors. This group consisted of four studies. General self-management skills [21,40] and exercise self-efficacy [36,37] were examined in patients with CKD, ESRD, and HD. Most of the researchers reported that the relationship between self-efficacy and self-management behaviors was significant [21,36,40]. Thus CKD patients with high self-efficacy ratings were highly likely to be interested in maintaining their current well-being or preventing its decline [21,36,40]. Although Washington et al. [37] reported no significant relationship between self-efficacy and exercise, the researchers documented that participants with high self-efficacy had a good outcome in managing and maintaining healthy behaviors such as communicating better with physicians, spending more time exercising per week, and successfully managing fluid restriction.
The third category was a health context for self-efficacy to mediate selfmanagement behaviors that can improve the effectiveness of self-care. This category consisted of two studies [7,39] both of which used self-efficacy as a mediator in the conceptual framework to investigate the relationship between knowledge, modifying factors, and self-management behaviors. The researchers identified predictors that increased the knowledge and self-care behaviors in CKD patients if self-efficacy was used as a mediator [7,39]. Wu and colleagues [39] revealed that self-efficacy was a crucial mediator between knowledge and self-care behaviors. Similarity, Sritarapipat and associates [7] indicated that self-efficacy was a mediator for overall self-management behaviors as well as its components (e.g., communication with health care provider, partnership in care, self-care activities, and self-advocacy behaviors). The component of self-efficacy was not clearly described in both studies. However, Wu et al. [39] described four subscales of self-efficacy in the section on the self-efficacy instrument: autonomy, self-integration, problem-solving, and social support.
Factors Improved Self-efficacy
In the chronic kidney disease population, factors related to self-efficacy were classified into three different types of interventions: physical, psychological, and educational (Table 1).
| Author/year | Study design/sample | Objective/intervention | Self-efficacy context/Instrument | Outcome assessed | Results |
|---|---|---|---|---|---|
| Educational intervention | |||||
| 1. Joboshi & Oka, 2017 [42] | An RCT, single-blind trial with one-to-one allocation into two groups. / A total of 65 CKD patients | To examine the effectiveness of the Encourage Autonomous Self-Enrichment patient education program | -Active coping behavior with disease and controllability for health /The self-efficacy scale for health behaviors in patients with chronic diseases | - primary outcomes: perceived self-efficacy and self-management behavior. - secondary outcomes: systolic and diastolic blood pressure and renal function data (creatinine, estimated glomerular filtration rate, serum potassium, and hemoglobin levels) |
The mean perceived self-efficacy score of the intervention group increased from 80.5 (75.0–86.5) at baseline to 85.0 (77.3– 91.0) after 12 weeks. The median self-management behavior score (interquartile range) in the intervention group increased to 57.0 (52.3–59.0) after 12 weeks from a baseline value of 51.5 (46.3–58.8). |
| 2. Kazawa, & Moriyama, 2013. | An RCT/ A total of 30 patients with type 2 diabetic nephropathy |
To provide an overview of the effects of a six-month educational program aimed at the acquisition of self-management skills on diabetic nephropathy patients. | - Active coping behavior with disease and controllability for health / The self-efficacy scale for health behaviors in patients with chronic illness | Self-management behaviors: engaged in the dietary, exercise, oral intake, and injection of prescribed drugs. | Significant difference: Self-efficacy (p<.01), exercise target behaviors (p <.05), frequency of self-monitoring (p<.001), frequency of drug intake and injection (p<.01) HbA1C (p<.05). No statistical difference: Albumin and B/P |
| 3. Lin et al., 2013 [15] |
Quasi-experimental; single-group pre-test/post-test; pilot study/A total of 37 CKD patients with stage 1-3a. |
To develop a self-management education program and to evaluate its effects on self-efficacy, self-management behavior, and CKD progression among patients with early-stage CKD. | Autonomy, self-integration, problem-solving, social support / The CKD Self-Efficacy (Lin et al., 2012) | Self-management behavior: self-integration, problem-solving, seeking social support, and adherence to the recommended regimen. | Significant difference: Self-efficacy (p<0.05) No statistical difference: eGFR using MDRD, self-management, and serum creatinine |
| 4.Slesnick et al. 2015 [28] | Quasi-experimental; single-group; pilot study/ 14 patients with ESRD |
To examine and evaluate the feasibility and effectiveness of the Chronic Disease Self-Management Program (CDSMP) in CKD patients with ESRD | Self-efficacy includes symptom control, role function, emotional functioning, and communication with physicians / Self-Efficacy for Managing Chronic Disease 6-Item Scale | Health status, self-efficacy, self-management behaviors, and health care utilization | During the 6-month period, self-efficacy was significantly increased. This means confidence levels in self-management increased among participants. |
| Physical interventions | |||||
| 1. Kauric-Klein et al. 2017. [35] | A RCT / A total of 118 participants were randomized to usual care (n=59) or intervention group (n =59). | To examine the effects of an education, self-regulation intervention on blood pressure self-efficacy, self-care outcomes, and blood pressure control in adults receiving hemodialysis. |
BP self-efficacy / The BP Control in HD Self-Efficacy Scale adapted from original scale of self-efficacy in the management of Type II Diabetes Mellitus (Bijl, et al. 1999) [18] | Self-management behaviors focused on dietary adherence and fluid compliance. | At 12 weeks, there was no significant increase in self-efficacy scores within or between groups. The overall self-efficacy was significantly related to some self-care outcomes, including decreased salt intake, lower IDWG, increased adherence to B/P medications, and fewer missed hemodialysis appointments. |
| 2. Tang et al. 2017 [41] | An RCT/ A total of 90 CKD patients were randomly assigned to the experimental group (n=45) and the control group (n=45). | To inspect the effects of a 12‐week home‐based exercise program on physical function, psychological dimensions, and health related QoL for patients with chronic kidney disease. | Self-efficacy for exercise / The Self‐Efficacy for Exercise (SEE) scale (Lee et al., 2009) [14] | Psychological dimensions, physical function, and quality of life | The differences between the exercise group and the control group were statistically significant for 6‐minute walk distance, the time to complete ten repetitions of the set-to stand test, self-efficacy for exercise, anxiety, and depression, and all domains of quality of life after a 12- week exercise program. Patients in the exercise group determined significant improvements in self‐efficacy scores compared with those in the control group: mean change 6.64 (6.92) versus −3.72 (6.80). |
| 3.Meuleman et al., 2017 [45] | An open RCT / A total of 138 patients with moderately decreased kidney function and hypertension. |
To evaluate the effectiveness and sustainability of self-managed sodium restriction in patients with chronic kidney disease. | Self-efficacy of managing the disease/ the Chronic Disease Self-Efficacy Scales to Manage Disease in General Scale | - sodium excretion and BP Secondary outcomes - protein excretion - kidney function - antihypertensive medication - Self-efficacy - QoL |
At three months and six months, self-efficacy score was increased in the intervention group compared to the control group. |
| Psychological interventions | |||||
|
A two-group, RCT / A total of 96 dialysis patients. | To improve effectively adaptive strategies for varying a patient’s misperceptions and to evaluate the effects of group psychosocial therapy in dialysis patients. |
Self-care self-efficacy / The Strategies Used by People to Promote Health (SUPPH) | -Self-care self-efficacy -Depression -Quality of life |
Most of the hemodialysis patients initially possessed a low level of self-care self-efficacy, suffered from depression and had a low quality of life. The hemodialysis patient group who received psychosocial intervention showed statistically significant improvement in their perceived self-care self-efficacy, depression and in the physical component of the quality of life indices. |
| Other factors | |||||
| 1. Montoyae et al. 2016 [8] | A two-group, repeated-measure experimental design/ A total of 26 patients from two sites of an outpatient nephrology practice: an intervention group (n=13) and a usual care group (n=13) |
To evaluate the feasibility of a NP-facilitated CKD group visit model versus the usual nephrology care in patients with stage 4 CKD. | NR/ Instrument: Self-Efficacy and Self-Management Behaviors in Patients with Chronic Kidney Disease tool (Curtin et al., 2008) [21] | Self-management skills: communication with caregivers, partnership in care, self-care, and self-advocacy. - CKD group visit model |
No significant time effects or group were detected for all subscales of self-management skills and self-efficacy. |
Table 1: Factors improved self-efficacy
Educational interventions: Four studies used an education intervention expected to influence self-efficacy in a CKD population [15,28,42,43]. Implementations such as class sessions, group sessions, and education programs were used. All studies found that self-efficacy increased significantly in the intervention group. Self-efficacy components were described in the section of the instrument. The studies of Kazawa and Moriyama [42] and Joboshi and Oka [43] used self-efficacy components that focused on psychological issues related to active coping behavior in response to disease and controllability for health, or perceived self-efficacy. Self-management behavior outcomes were evaluated in terms of medical compliance (injection of prescribed drugs), physical conditions (blood pressure, body weight) drinking and smoking, nutrition, exercise, and infection prevention [42,43].
In the intervention of Lin et al. [15], self-efficacy was related to other concepts regarding mediators, or moderators of self-care, self-management, and selfregulation. The self-efficacy tool developed by Lin and colleagues [15], used to evaluate the CKD patient’s self-efficacy, contained four components: autonomy, self-integration, problem-solving, and social support. Efforts to enhance self-efficacy were included. Modeling of self-management behaviors, vicarious experience by observing others, and recognition of outcome performance were used to improve self-efficacy [15].
A quasi-experimental study performed by Kazawa and Moriyama [43] used positive feedback when changes in target behaviors were achieved. Strategies to improve self-efficacy were not described in two other studies [28,42]. Even though self-efficacy was significantly different in the intervention and the control group, there were no significant improvements in blood pressure (Table 1).
Physical interventions: Physical interventions that have been proposed to have an impact on self-efficacy were the focus of three studies. Kauric-Klein and colleagues [43] examined the effects of a self-regulation intervention on blood pressure self-efficacy, self-care outcomes, and blood pressure control in HD patients. The authors evaluated two self-management outcomes: dietary adherence and fluid intake compliance.
A study of Tang et al. [41] used a two-group, randomized controlled trial to examine the effects of a 12-week home-based exercise program among patients with CKD. Even though the components of self-efficacy were not clearly described, a particular tool, the self-efficacy for exercise scale, was used to assess self-efficacy for exercise. Patients in the exercise group demonstrated significant improvements in self-efficacy scores [41].
Meuleman and associates [45] applied an open randomized controlled trial to evaluate the effectiveness and sustainability of self-managed sodium restriction in patients with moderately decreased kidney function and hypertension. At three months and six months, self-efficacy score was increased in the intervention group compared to the control group.
Psychological interventions: Psychological factors are a third area that may impact self-efficacy. The impact of a psychological intervention was examined in a study by Lii et al. [38] that investigated the effects of group intervention on depression, self-efficacy, and quality of life in patients with hemodialysis. The authors used cognitive-behavioral therapy (CBT) and self-efficacy theory as a basis of group intervention. In the implementation step, strategies used to motivate patients consisted of performance accomplishment, modeling, verbal persuasion and interpretation of physiological symptoms. The authors applied these motivational approaches derived from Bandura’s self-efficacy theory [19]. Psychosocial intervention significantly enhanced self-care selfefficacy of the hemodialysis patients. Also, a more recent study reported that most hemodialysis patients with a low level of self-care self-efficacy suffered from depression and had a poor quality of life [38]. After implementation, the treatment group showed statistically significant improvement in their perceived self-care self-efficacy, in their level of depression and in the physical component of the quality of life indices [38]. In sum, a psychological intervention appears to be able to promote self-efficacy.
Other factors: The above studies described specific interventions. Another factor was represented by only one study; Montaya, Sole, and Norris [8] focused on a group visit associated with self-efficacy. The authors compared the feasibility of a NP-facilitated CKD group-visit model with the usual nephrology care in stage 4 CKD patients. The findings showed no significant group effect on the self-efficacy and self-management subscales regarding communication, partnership in care, self-care, and self-advocacy.
Outcomes Related to Self-efficacy
The important outcomes related to self-efficacy of patients with CKD varied among studies. Self-efficacy might be used as a mediator or predictor to answer the question of patient involvement with outcomes. Outcomes following intervention, shown in Table 2, indicated that different outcomes were assessed and reported. They were classified into four groups of targeted outcomes: general self-management behaviors or skills [7,21,37,39,40]; physical activity [36]; physiological indices [33,44]; and fluid and dietary compliance [34]. Significant findings were lacking in only one study [37].
| Author/year | Study design/sample | Objective/intervention | Self-efficacy context/Instrument | Outcome assessed | Results |
|---|---|---|---|---|---|
| SE for adoption and maintenance of self-management behaviors | |||||
| 1.Curtin et al., 2008 [21] | Cross-sectional survey/174 patients with CKD | To explore the relationship between perceived self-efficacy and self-management behaviors in patients with CKD. | NR / the Perceived Efficacy in Patient-Physician Interaction Questionnaire (PEPPI) |
Self-management behavior: communication with caregivers, partnership in care, self-care, self-advocacy, medication adherence | Perceived self-efficacy was positively associated with four of the five categories of self-management behavior, controlling for patient age, education, diabetic status, hypertension, serum creatinine level, mental component summary and physical component summary. |
| 2.Li et al. 2014 [40] | A descriptive study/ A convenience sample of 198 patients undergoing hemodialysis was recruited from dialysis centers in three tertiary hospitals in Beijing. | To examine self-management levels, and explore factors influencing self-management behaviors in patients undergoing hemodialysis. | NR / Chronic Disease Self-Efficacy Scale (Lorig et al., 1996) [20] | Self-management behavior: problem-solving, emotional management, self-care, partnership | Self-efficacy was significantly associated with overall self-management and its subscales. Self-efficacy was a predictor of the partnership (25.9% of the variance), problem-solving (18.2% of the variance), and emotional management (26% of the variance). |
| 3. Patterson et al., 2014 [36] | A cross-sectional design/ A total of 115 patients with ESRD undergoing chronic hemodialysis | To use SCT constructs self-efficacy, outcome expectations, and self-regulation to better understand associations of physical activity (PA) behaviors among dialysis patients after controlling for demographic and health-related factors. | Exercise self-efficacy / the Spinal Cord Injury Exercise Self-Efficacy Scale. |
Physical activity (PA) behaviors |
Physical activity had a significant relationship with self-efficacy (r=336), self-regulation (r=.280), and outcome expectations (r=.265) among people on dialysis in bivariate analyses. The findings revealed significant increases in variance explained by the addition of self-efficacy, self-regulation, and covariates (p<.01). Younger age, self-efficacy, and self-regulation were associated (p<.10) with greater participation in physical activity in the final model (R2=0.272). |
| 4. Washington,et al. 2016 [37] | Mixed method/ A total of 107 end-stage CKD patients undergoing hemodialysis. | To identify factors associated with self-management in end-stage CKD patients undergoing hemodialysis. | NR / The Chronic Disease Self-Management Program’s (CDSMP) Diabetes Self-Efficacy Scale | Self-management behavior: exercise behaviors, communication with physicians, cognitive symptom management, and fluid and diet management. | Self-efficacy had no significant relationship with self-management behavior. Although not significantly different, the high self-efficacy group spent more time exercising per week, communicated better with physicians, and spent more days over a 2-week period successfully managing their fluid restrictions. |
| SE for managing a CKD and its condition | |||||
| 1.Balaga, 2012 [44] | A descriptive-correlational study/ A total of 50 patients acquiring hemodialysis | To determine the relationship between self-efficacy and self-care management outcome of CRF patients as a basis for developing self-care management guidelines. | Magnitude and strength of diet adherence, compliance with hemodialysis treatment and medications. Instrument: NR |
Physiological indicators: Albumin, pre BUN, IDWG correlated to diet adherence; Kt/V level and URR pertained to compliance with hemodialysis treatment; and phosphorus, hemoglobin, and hematocrit associated with compliance with medications. | Albumin (p=0.023) and IDWG (p=0.029) had a significant relationship to diet adherence and self-efficacy. Kt/V (p=0.469) and URR (p=0.865) had no significant association with compliance to dialysis treatment. Hemoglobin and hematocrit had a significant positive relationship to compliance with HD medications. Phosphorus levels had an inverse relationship to patient’s compliance with medications. |
| 2. Johnet al. 2013 [34] | A descriptive-correlation study design/A total of 100 eligible ESRD patients who receive routine hemodialysis three times a week | To determine the relationship between self-efficacy and fluid and dietary compliance in hemodialysis patients, as well as to identify the barriers that prevent patient compliance. | NR / the modified version of Your Health and Well-Being questionnaire | fluid and dietary compliance | Self-efficacy had a strong positive correlation with daily fluid restriction and dietary restriction compliance. As predicted, the more self-efficacy the participant reported, the higher the self-reported dietary and fluid restriction compliance. |
| 3. Elliott et al. 2015 [33] | Cross-sectional survey/A total of 95 hemodialysis patients | To examine the stages of change and dietary adherence in patients undergoing HD. | - aspects of lifestyle management regarding diet and medication adherence / The Chronic Kidney Disease Self-Efficacy Scale | Serum phosphorus level | Individual health beliefs associated with diet adherence involved with perceived benefits OR 3.18 (1.47-6.88), and self-efficacy OR 1.22 (1.09-1.38). Individual health beliefs correlated with phosphorus control included self-efficacy OR 1.08 (1.01-1.16). |
| SE for mediating the self-management behaviors to improve the effectiveness of self-care. | |||||
| 1.Wu et al. 2016 [39] | A cross-sectional and correlational design / A total of 247 purposive CKD patients in the renal outpatient clinics and dialysis center of two teaching hospitals in northern Taiwan. | To investigate the relationships among knowledge, self-efficacy and self-care behavior in CKD patients and examine whether self-efficacy was a predictive mediator of self-care behavior. | SE: autonomy, self- integration, problem- solving, and seeking social support / Chronic Kidney Disease Self-Efficacy Instrument (CKD-SE) | Self-care behavior | Self-efficacy was a crucial mediator between self-care behavior and knowledge. Self-efficacy was positively correlated with self-care. Self-efficacy fully mediated the relationship between knowledge and self-care and the effect was 50%. |
| 2. Sritarapipat et al., 2012 | A cross-sectional, predictive study/ A total of 216 elderly Thais with pre-dialysis chronic kidney disease | To examine directly and indirectly factors affecting elderly Thais’ self-management behaviors of pre-dialysis chronic kidney disease. | NR / Perceived Self-Management Self-Efficacy Questionnaire (PSMESEQ) [21] |
Self-management behaviors: communication with a partnership in care, health care providers, self-care activities, self-advocacy behaviors, medication adherence behavior. | The subjects’ self-efficacy was found to be a mediator between overall self-management behaviors as well as its components: communication with health care providers, partnership in care, self-care activities, and self-advocacy behaviors. |
Table 2: Self-efficacy health contexts reflected in the studies
Regarding the first targeted outcome, self-management skills, Li et al. [40] included problem-solving, emotional management, self-care, and partnership. Curtin et al. [21] and Sritarapipat et al. [7] also used outcomeindicated components of self-management skills: self-care, self-advocacy, communication with caregivers, partnership in care, and medication adherence. Self-management skills in the study by Washington et al. [37] consisted of exercise behaviors, communication with physicians, fluid and diet management, and cognitive symptom management. Only Wu et al. [39] omitted the details of self-care components.
Physical activity was the principal outcome that Patterson and associates [36] measured in dialysis patients. They used an instrument designed specifically to assess a population undergoing long-term treatment to evaluate the CKD patient’s confidence with regard to exercise. The results of multivariate analyses revealed that self-efficacy had the strongest relationship to physical activity, compared with other social cognitive variables in people receiving dialysis treatment, followed by self-regulation [36].
Fluid and dietary compliance were used as the outcomes in the study by John et al. [34]. Non-adherence to fluid and dietary limitations compromises the outcomes of patients receiving hemodialysis and can lead to negative longterm outcomes such as cardiovascular disease, heart failure, and hypertension [34]. Also, the authors concluded that improving patient self-efficacy levels and self-management capacities can help to decrease barriers that typically prevent dietary and fluid restriction compliance in ESRD patients [34].
The studies by Balaga [44] and Elliott et al. [33] used physiological indicators of CKD as the dependent variables. They measured numerous kinds of indicators such as albumin, pre-blood urea nitrogen (BUN), interdialytic weight gain (IDWG), Kt/V level, urea reduction ratio (URR), phosphorus, hemoglobin, and hematocrit. Researchers have linked these CKD indicators with self-efficacy in efforts to determine how self-efficacy associated with physiological indicators affected self-management behaviors. In the study by Balaga [44], self-efficacy was evaluated in three domains of managing CRF: diet adherence, compliance with hemodialysis treatment and medications. Each self-efficacy domain was measured in terms of its magnitude and strength. The overall strength of all domains transferred to the generality of patient’s self-efficacy. As a result, the relationship of self-efficacy to albumin and to IDWG was found to be significant [44]. Similarly, Elliott and associates [33] used serum phosphorus level as the outcome to determine the relationship between self-efficacy and serum phosphorus control. Self-efficacy was shown to be associated with diet adherence and serum phosphorus control [33].
The gap in the knowledge of self-efficacy in patients with CKD led to the present integrative review of the literature, which examines and reports on relationships between self-efficacy and self-management behaviors. Some reviews that involved self-efficacy features of CKD patients have reported that in the results, factors related to self-efficacy, health contexts for selfefficacy, and outcomes are less forthright, needing some examine. Thus, the discussions focused on factors related to self-efficacy, health contexts for selfefficacy, and the association of self-efficacy to self-management behaviors.
The consistently significant results reported providing evidence that selfefficacy might be influenced by educational, physiological, and psychological interventions. Educational programs for CKD patients aim to provide and test the effectiveness of their implementation in CKD. This type of program seems to be commonly used to improve the patient’s self-efficacy. A change of self-efficacy activation is often accompanied by changes in self-management behaviors. Thus, future researchers may need to consider tailoring or targeting interventions to the individual’s activation level. Strategies for increasing self-efficacy were mostly underdeveloped or not described. Further development is needed, as supported by findings from a descriptive study performed by Curtin et al. [21], in which higher self-efficacy was associated with better self-care.
All publications in this review were used in examining self-efficacy for CKD as reported in three categories of health contexts that required consideration of healthy behaviors to maintain and manage health conditions. The three groups included self-efficacy health contexts of adoption and maintenance of healthy behaviors, management of CKD and its condition, and mediation of self-management behaviors. These health contexts did not include acute renal failure or acute situations in which a behavior cannot be predicted easily. Consequently, self-efficacy is highly relevant in health contexts in which intermediate or long-term care for CKD patients is needed.
Researchers have demonstrated that self-efficacy played a role as a mediator, having a significant association with outcomes. Outcomes varied and were associated with vague findings across the reviewed studies. Therefore, health outcomes were categorized into four groups: general self-management skills, physical activity, dietary and fluid compliance, and physiological indicators. Self-management theory was frequently used in the study of CKD patients. To assess factors and modifiers or mediators related to self-management of healthy behaviors, self-efficacy was selected as an important aspect. Using sources of perceived self-efficacy information to influence self-management behavior among CKD patients may, therefore, be beneficial. For example, the intention to maintain a regular exercise program was best predicted by a high level of perceived self-efficacy [41]. Similarly, the intention to eat a low-salt diet was mainly determined by self-efficacy [35], although this effect was qualified by modifying factors. Further development of multiple intervention-comprising factors is warranted. To measure outcomes, psychometric properties of instruments were sometimes not thoroughly described and reported. Therefore, instrument of self-efficacy may need additional psychometric testing and more explanations of the reason for using them in studies of CKD.
Limitation
This integrative review, which examined relationships between self-efficacy and self-management behavior in patients with CKD, had several limitations. First, no qualitative study related to self-efficacy was identified in the search. Second, the search strategy used may have resulted in some journals being missed. Third, studies included in this integrative review used a variety of methodology quality, outcomes, and use of self-efficacy instruments. However, all were reviewed in accordance with the Whittemore and Knaft [1] framework and guided as outlined by Cooper [2].
Conclusion
Researchers have contributed to a growing body of evidence that supports the relationship between self-efficacy and CKD, with use of various research designs. The adoption of health-promoting behaviors and elimination of health-impairing behaviors need elements of self-efficacy as important variables. Among self-efficacy and self-management behavior, perceived selfefficacy plays a role as a major contributor that affects not only the decisionmaking process but also the initiation and maintenance process. Researchers have begun to identify a relationship between factor and outcome by using the role of perceived self-efficacy to improve self-management skills and behaviors of patients. Self-efficacy has been linked to intentions. Patients with CKD may have little confidence in their ability to manage their illness [8,29].
Currently, the important goal in caring for persons with CKD is to slow chronic kidney disease progression and maintain the kidney’s function as long as possible from the early stages. Guidelines to slow the progression promote to patients modification of their lifestyle, diet control, blood pressure monitoring and medication control [5]. To manage themselves, persons with CKD must be capable of applying self-management and selfefficacy strategies that help ensure appropriate health behavior to prevent deterioration of the kidneys as well as to avoid progression of the disease to end-stage renal disease [10].
Understanding the functions and concepts of self-efficacy is important in developing tailored and targeted interventions and supporting CKD patients in managing their illness. Also, it is important to consider self-efficacy as a mediator with self-care strategies to influence persons’ ability to self-manage their CKD. Additionally, the conceptual model of self-efficacy developed from the current integrative review illustrates the key elements suitable for allowing persons with CKD to influence their ability to maintain kidney function and slow the progression of the disease (Figure 2). This model highlighted the factors influencing self-efficacy, health contexts for selfefficacy, and self-management behaviors outcomes. Consequently, the findings will meet the complex and interrelated needs of this CKD group for conducting further perceived self-efficacy interventions. In future implementation, testing this model will be necessary.
Figure 2: Self-efficacy conceptual model reflecting from the studies
REFERENCES
- Whittemore R, Knafl K. The integrative review: updated methodology. J Adv Nurs. 2005;52:546-53.
- Cooper HM. Integrating research: A guide for literature reviews. Sage Publications. 1989
- Dobkowski D, Zuber K, Davis J. Updated guidelines for managing chronic kidney disease. JAAPA. 2013;26:27-31.
- Inker LA, Astor BC, Fox CH, et al. KDOQI US commentary on the 2012 KDIGO clinical practice guideline for the evaluation and management of CKD. Am J Kidney Dis. 2014;63:713-35.
- Eknoyan G, Lameire N, Eckardt KU. Kidney Disease Improving Global Outcomes (KDIGO) CKD Working Group. KDIGO 2012 clinical practice guidelines for the evaluation and management of chronic kidney disease. Kidney Int. 2013;2:1-163.
- Stevens PE, Levin A. Evaluation and management of chronic kidney disease: synopsis of the kidney disease: improving global outcomes 2012 clinical practice guideline. Ann Intern Med. 2013;158:825-30.
- Sritarapipat P, Pothiban L, Panuthai S, et al. Causal model of elderly Thais' self-management behaviors of pre-dialysis chronic kidney disease. Pacific Rim Int J Nurs Res. 2012;16:277-93.
- Montoya V, Sole M L, Norris AE. Improving the care of patients with chronic kidney disease using group visits: a pilot study to reflect an emphasis on the patients rather than the disease. Nephrol Nurs J. 2016;43:207-22.
- Vassalotti JA, Kaufman HW. New guidelines to evaluate and manage chronic kidney disease. Medical Laboratory Observer. 2013;45:24-6.
- Jha V, Garcia-Garcia G, Iseki K, et al. Chronic kidney disease: global dimension and perspectives. Lancet. 2013;382:260-72.
- Sinasac L. The community health promotion plan: a CKD prevention and management strategy. CANNT J. 2012;22:25-28.
- Bonner A, Havas K, Douglas C, et al. Self-management programs in stages 1-4 chronic kidney disease: A literature review. J Ren Care. 2014;40:194-204.
- Ferris ME, Cuttance JR, Javalkar K, et al. Self-management and transition among adolescents/young adults with chronic or end-stage kidney disease. Blood Purif. 2015;39:99-104.
- Lee MC, Wu SFV, Hsieh NC, et al. Self-Management programs on eGFR, depression, and quality of life among patients with chronic kidney disease: A meta-analysis. Asian Nurs Res. 2016;10:255-62.
- Lin C, Tsai F, Lin H, et al. Effects of a self-management program on patients with early-stage chronic kidney disease: A pilot study. Appl Nurs Res. 2013;26:151-6.
- Zimbudzi E, Lo C, Misso M, et al. Effectiveness of management models for facilitating self-management and patient outcomes in adults with diabetes and chronic kidney disease. Syst Rev. 2015;4:81-9.
- Walker R, Marshall MR, Polaschek N. Improving self-management in chronic kidney disease: A pilot study. Renal Soc Australasia J. 2013;9:116-25.
- Wierdsma J, van Zuilen A, van der Bijl J. Self‐efficacy and long-term medication use in patients with chronic kidney disease. J Ren Care. 2011;37:158-66.
- Bandura A. Self-efficacy in changing societies. Cambridge University Press 1997.
- Lorig KR, Holman HR. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med. 2003;26:1-7.
- Curtin RB, Walters BA, Schatell D, et al. Self-efficacy and self-management behaviors in patients with chronic kidney disease. Adv Chronic Kidney Dis. 2008;15:191-205.
- Enworom CD, Tabi M. Evaluation of kidney disease education on clinical outcomes and knowledge of self-management behaviors of patients with chronic kidney disease. Nephrol Nurs J. 2015;42:363-72.
- Flesher M, Woo P, Chiu A, et al. Self-management and biomedical outcomes of a cooking, and exercise program for patients with chronic kidney disease. J Ren Nutr. 2011;21:188-95.
- Murphree DD, Thelen SM. Chronic kidney disease in primary care. J Am Board Fam Med. 2010;23:542-50.
- Bandura A. Perceived self-efficacy in cognitive development and functioning. Educ Psychol 1993;28:117-48.
- Chen SH, Tsai YF, Sun CY, et al. The impact of self-management support on the progression of chronic kidney disease—a prospective randomized controlled trial. Nephrol Dial Transplant. 2011;26:3560-6.
- Moattari M, Ebrahimi M, Sharifi N, et al. The effect of empowerment on the self-efficacy, quality of life and clinical and laboratory indicators of patients treatedwith hemodialysis: a randomized controlled trial. Health Qual Life Outcomes. 2012;10:115.
- Slesnick N, Pienkos S, Sun S, et al. The chronic disease self-management program—A pilot study in patients undergoing hemodialysis. Nephrol News Issues. 2015;29:22-3.
- Drenzyk DE, Gardner M, Welch JL. Knowledge, Self-management, and Self-efficacy in CKD Patients. Nephrol Nurs J. 2014;41:202.
- Echouffo-Tcheugui JB, Kengne AP. Risk Models to Predict Chronic Kidney Disease and Its Progression: A Systematic Review. PLoS Med. 2012;9:e1001344.
- Tangri N, Kitsios GD, Inker LA, et al. Risk prediction models for patients with chronic kidney disease:A systematic review. Ann Intern Med. 2013;158:596-603.
- Garrard J. Health sciences literature review made easy. Jones & Bartlett Publishers. 2017.
- Elliott JO, Ortman C, Almaani S, et al. Understanding the associations between modifying factors, individual health beliefs, and hemodialysis patients' adherence to a low-phosphorus diet. J Ren Nutr. 2015;25:111-20.
- John A, Alpert PT, Kawi J, et al. The relationship between self-efficacy and fluid and dietary compliance in hemodialysis patients. Clin Scholars Rev. 2013;6:98-104.
- Kauric-Klein Z, Peters RM, Yarandi HN. Self-Efficacy and Blood Pressure Self-Care Behaviors in Patients on Chronic Hemodialysis. West J Nurs Res. 2017;39:886-905.
- Patterson MS, Umstattd Meyer MR, Beaujean AA, et al. Using the social cognitive theory to understand physical activity among dialysis patients. Rehabil Psychol. 2014;59:278-88.
- Washington T, Zimmerman S, Browne T. Factors associated with chronic kidney disease self-management. Soc Work Public Health. 2016;31:58-69.
- Lii YC, Tsay SL, Wang TJ. Group intervention to improve quality of life in hemodialysis patients. J Clin Nurs. 2007;16:268-75.
- Wu SF, Hsieh NC, Lin LJ, et al. Prediction of self‐care behavior on the basis of knowledge about chronic kidney disease using self‐efficacy as a mediator. J Clin Nurs. 2016;25:2609-18.
- Li H, Jiang YF, Lin CC. Factors associated with self-management by people undergoing hemodialysis: A descriptive study. Int J Nurs Stud. 2014;51:208-16.
- Tang Q, Yang B, Fan F, et al. Effects of individualized exercise program on physical function, psychological dimensions, and health-related quality of life in patients with chronic kidney disease: A randomized controlled trial in China. Int J Nurs Pract. 2017;23:e12519.
- Joboshi H, Oka M. Effectiveness of an educational intervention (the Encourage Autonomous Self-Enrichment Program) in patients with chronic kidney disease: A randomized controlled trial. Int J Nurs Stud. 2017;67:51-8.
- Kazawa K, Moriyama M. Effects of a self-management skills-acquisition program on pre-dialysis patients with diabetic nephropathy. Nephrol Nurs J. 2013;40:141-8.
- Balaga PAG. Self-efficacy and self-care management outcome of chronic renal failure patients. Asian J Health 2012;2:111-29.
- Meuleman Y, Hoekstra T, Dekker FW, et al. Sodium restriction in patients with CKD: a randomized controlled trial of self-management support. Am J Kidney Dis. 2017;69:576-86.